Initial Trauma Resuscitation Guideline
advertisement
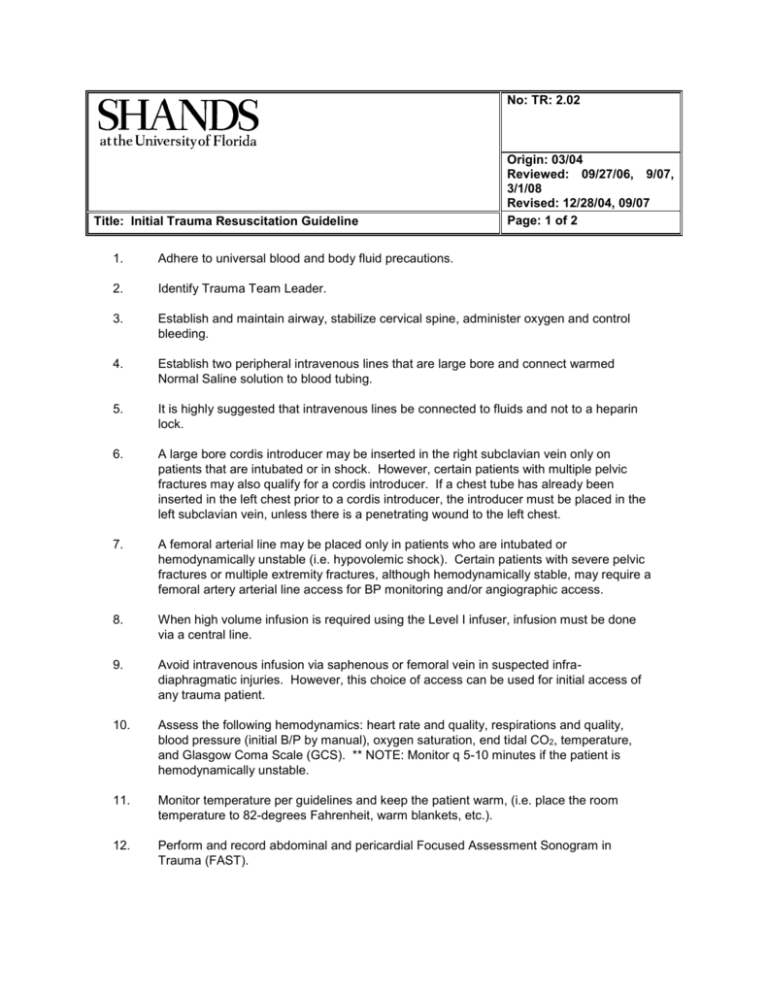
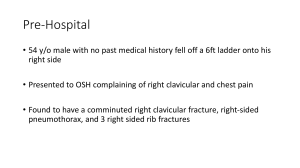
No: TR: 2.02 Title: Initial Trauma Resuscitation Guideline Origin: 03/04 Reviewed: 09/27/06, 9/07, 3/1/08 Revised: 12/28/04, 09/07 Page: 1 of 2 1. Adhere to universal blood and body fluid precautions. 2. Identify Trauma Team Leader. 3. Establish and maintain airway, stabilize cervical spine, administer oxygen and control bleeding. 4. Establish two peripheral intravenous lines that are large bore and connect warmed Normal Saline solution to blood tubing. 5. It is highly suggested that intravenous lines be connected to fluids and not to a heparin lock. 6. A large bore cordis introducer may be inserted in the right subclavian vein only on patients that are intubated or in shock. However, certain patients with multiple pelvic fractures may also qualify for a cordis introducer. If a chest tube has already been inserted in the left chest prior to a cordis introducer, the introducer must be placed in the left subclavian vein, unless there is a penetrating wound to the left chest. 7. A femoral arterial line may be placed only in patients who are intubated or hemodynamically unstable (i.e. hypovolemic shock). Certain patients with severe pelvic fractures or multiple extremity fractures, although hemodynamically stable, may require a femoral artery arterial line access for BP monitoring and/or angiographic access. 8. When high volume infusion is required using the Level I infuser, infusion must be done via a central line. 9. Avoid intravenous infusion via saphenous or femoral vein in suspected infradiaphragmatic injuries. However, this choice of access can be used for initial access of any trauma patient. 10. Assess the following hemodynamics: heart rate and quality, respirations and quality, blood pressure (initial B/P by manual), oxygen saturation, end tidal CO2, temperature, and Glasgow Coma Scale (GCS). ** NOTE: Monitor q 5-10 minutes if the patient is hemodynamically unstable. 11. Monitor temperature per guidelines and keep the patient warm, (i.e. place the room temperature to 82-degrees Fahrenheit, warm blankets, etc.). 12. Perform and record abdominal and pericardial Focused Assessment Sonogram in Trauma (FAST). No: TR: 2.02 Origin: 03/04 Reviewed: 02/06 Revised: 12/28/04, 09/07 Title: Initial Trauma Resuscitation Guideline Page: 1 of 2 13. Obtain the following radiographs: Chest Pelvis (high index suspicion) Mandatory on all falls from height of 6 feet or higher Complete spine CT with reconstruction (cervical, thoracic, lumbar) Bilateral wrist x-rays Bilateral ankle (calcanei) x-rays 14. Obtain following labs from ISTAT: ABG’s, Lactic Acid, hemoglobin & hematocrit NA, K, Ca, PT with INR. In patients greater then age 55 years old draw Creatinine. Draw blood alcohol on all drivers or when there is a high index of suspicion of alcohol use. Type and Screen and/or Type and Cross as directed by the physician. HCG test for females of childbearing age. 15. When indicated, insert oral/nasogastric tube, assure its position in the stomach, and irrigate with saline as needed to establish effective function and attach to suction. In mid and upper facial fractures as directed by physician. 16. Perform rectal exam. 17. Insert indwelling urinary catheter (unless evidence of bleeding from the urethra or abnormal rectal exam). Record volume and gross characteristics of urine and attach to urimeter. Use indwelling temperature probe for continuous monitoring of patient hemodynamics. 18. Apply pelvic binder for major unstable pelvic fractures. 19. Administer pain medication and sedation as ordered. 20. Perform stat EKG when indicated (i.e. geriatric trauma patient, cardiac history, hear rate irregularity). 21. Tetanus prophylaxis as indicated by age and history. 22. Call consults for emergent indications from the trauma room: a. Orthopaedic Surgeon for dislocations of hip, elbow, knee or crushed extremities b. Neurosurgeon for focal neurologic sign (i.e. blown pupil, paralysis or GCS less than 8).