Antimicrobial agents
advertisement
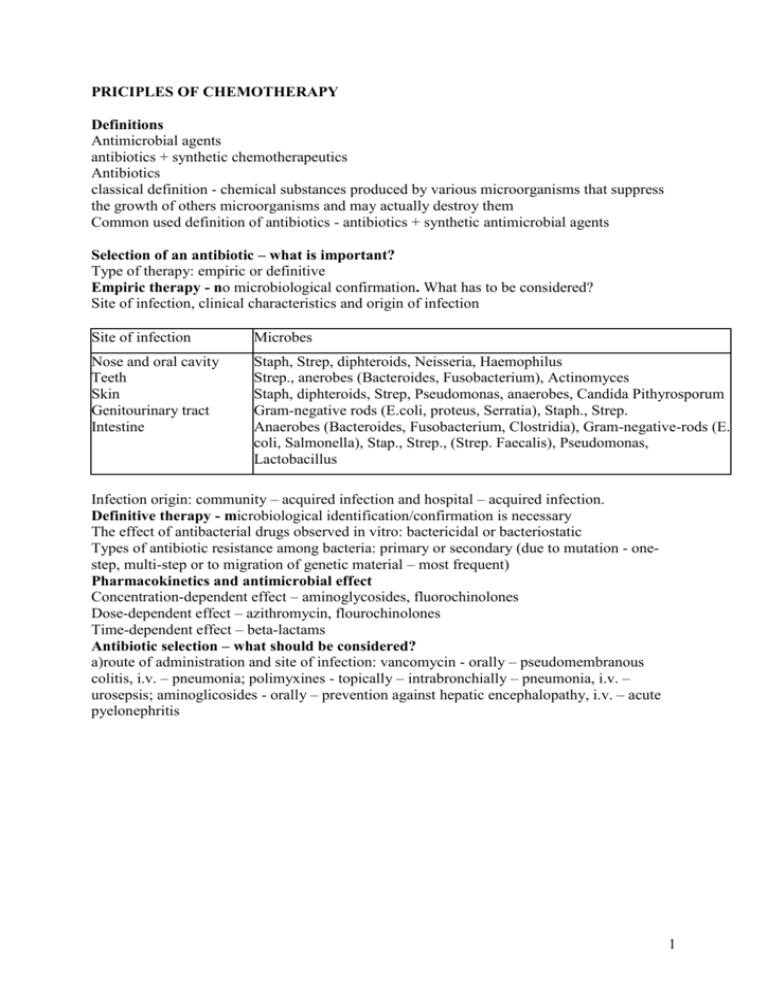
PRICIPLES OF CHEMOTHERAPY Definitions Antimicrobial agents antibiotics + synthetic chemotherapeutics Antibiotics classical definition - chemical substances produced by various microorganisms that suppress the growth of others microorganisms and may actually destroy them Common used definition of antibiotics - antibiotics + synthetic antimicrobial agents Selection of an antibiotic – what is important? Type of therapy: empiric or definitive Empiric therapy - no microbiological confirmation. What has to be considered? Site of infection, clinical characteristics and origin of infection Site of infection Microbes Nose and oral cavity Teeth Skin Genitourinary tract Intestine Staph, Strep, diphteroids, Neisseria, Haemophilus Strep., anerobes (Bacteroides, Fusobacterium), Actinomyces Staph, diphteroids, Strep, Pseudomonas, anaerobes, Candida Pithyrosporum Gram-negative rods (E.coli, proteus, Serratia), Staph., Strep. Anaerobes (Bacteroides, Fusobacterium, Clostridia), Gram-negative-rods (E. coli, Salmonella), Stap., Strep., (Strep. Faecalis), Pseudomonas, Lactobacillus Infection origin: community – acquired infection and hospital – acquired infection. Definitive therapy - microbiological identification/confirmation is necessary The effect of antibacterial drugs observed in vitro: bactericidal or bacteriostatic Types of antibiotic resistance among bacteria: primary or secondary (due to mutation - onestep, multi-step or to migration of genetic material – most frequent) Pharmacokinetics and antimicrobial effect Concentration-dependent effect – aminoglycosides, fluorochinolones Dose-dependent effect – azithromycin, flourochinolones Time-dependent effect – beta-lactams Antibiotic selection – what should be considered? a)route of administration and site of infection: vancomycin - orally – pseudomembranous colitis, i.v. – pneumonia; polimyxines - topically – intrabronchially – pneumonia, i.v. – urosepsis; aminoglicosides - orally – prevention against hepatic encephalopathy, i.v. – acute pyelonephritis 1 b) absorption Agent Disease Bioavailability Amoxicillin Celiac disease Erythromycin Leśniowski-Crohn disease Trimetoprim Celiac disease Vankomycin Ulcerative colitis Metronidazole Ulcerative colitis Clindamycin Leśniowski-Crohn disease c)distribution - proteins in plasma: hipoalbuminemia (hepatic failure, nephrotic syndrome) – Sulfonamides? Aminoglycosides? Leukocytosis (leukemia), anemia – Aminoglycosides? CNS infection - Penicillins? Metronidazole? Aminoglycosides? Bones infection. Clindamycin? Aminoglycosides? Prostatitis. Norfloxacin? Aminopenicillins? Biliary tract infection. Ampicillin? Natural penicillins? d) topical factors - hematoma, abscessus, urine pH, gastic acid pH, synthetic valves, vascular prostheses, catheters e)time of therapy - urethitis – 1-3 days, endocardistis – 30 days, pneumonia 7-21 days f) adverse effects Kidneys dysfunction – avoid: aminoglycosides, vancomycin, polipeptides, amphotericin B. Liver dysfunction - avoid: doxycyclin, clindamycin, erythromycin, ketokonazole, isoniasid Neurologic diseases. Attention: high doses of natural penicillins, nitrofurantoin, quinolones Hypersensitivity. Attention: beta-lactams, sulfonamides, macrolides Genetic problems. Sulfonamides, nitrofurantoin – glucose-6-phosphate dehydrogenase deficiency Neutropenia. Attention: metronidazole, aminopenicillins, cefalosporins Anemia. Attention: zidovudine, amphotericin B g) patient status - proteins in plasma • Organs function : GI tract, liver, kidneys • Age: neonates and infants – tetracyclines, quinolones, sulfonamides!!! Older persons: attention: tetracyclines, aminoglycosides, vancomycin, quinolones Pregnancy and lactation: acceptable –natural penicillins, aminopenicillins, 1st generation cephalosporins, erythromycin Contraindicated: quinolones, tetracyclines, sulfonamides • diabetic foot – angiopathy • immunosupression - neutropenia, limfopenia 2 Indications for the clinical use of antibiotics combinations • treatment of mixed infections • empiric therapy • achievement of synergism • doses reduction • resistance prevention Combination of: • ..cidal+..cidal - synergism or indifference (additive result), never antagonism • ..static+..static - additive effect, never synergism or antagonism • ..cidal+..static- indifference or antagonism when bacteria is high susceptible to ..cidal or synergism when bacteria is low susceptible to ..cidal The prophylaxis of infection with antibiotics • to protect healthy persons from acquisition of or invasion by specific microorganism to which they are exposed • to prevent secondary bacterial infections in patients who are ill with other diseases • to prevent endocarditis in patients with valvular or other structural lesions of the heart who are undergoing dental, surgical or other procedures that produce a high incidence of bacteriemia • to prevent wound infections after various surgical procedures Superinfections The appearance of bacteriological and clinical evidence of a new infection during chemotherapy of a primary one. • changes in the normal microbial population of the intestinal, upper respiratory and genitourinary tract • when broad-spectrum agents are used 3