H. influenza, Moraxella

ANTIBIOTICS
LauraLe Dyner MD
Pediatric Infectious Disease Fellow
March 2009
PREP Question
A 14-year-old boy with a h/o CF is admitted with a pulmonary exacerbation. His sputum grows Pseudomonas.
What is the most appropriate therapy (+ an aminoglycoside)?
A. Ampicillin
B. Ceftriaxone
C. Cefuroxime
D. Pipericillin
E. Vancomycin
PREP Question
A 10-year-old boy with a h/o short gut syndrome has coagulase-negative Staph bacteremia. What is the most appropriate antibiotic therapy?
A. Cephalothin
B. Clindamycin
C. Nafcillin
D. Penicillin G
E. Vancomycin
PREP Question
Of the following, the greatest advantage of using a 3 rd generation cephalosporin over an aminoglycoside, is a lower rate of:
A. Hypersensitivity reactions
B. Nephrotoxicity
C. Pseudomembraneous colitis
D. Thrombocytopenia
E. Thrombophlebitis
PREP Question
A 2-year-old girl develops meningococcal meningitis. Family members are prescribed rifampin.
What medication may be less effective when taking rifampin?
A. Amoxicillin
B. Furosemide
C. Oral contraceptives
D. Ranitidine
E. Salicylates
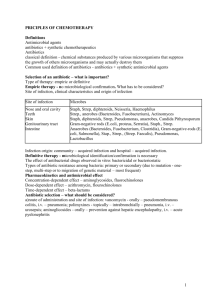
History of Antibiotics
Molds were used in ancient cultures
1880s: Search for antibiotics began after acceptance of the germ theory
1929: The mold penicillium was found to inhibit bacterial growth of Staph aureus
1935: Synthetic antimicrobial were discovered
(sulfonamides)
1942: Penicillin G Procaine was manufactured & sold
1940s-1960s: Natural antibiotics (streptomycin, chloramphenicol, tetracycline, etc) were discovered
Microbial
Sources of
Antibiotics
Classes of Antibiotics
Spectrum of Activity
Gram-positives
Gram-negatives
Anaerobes
Atypicals
Mycobacteria
Chemical structure
Mechanism of Action
1955
1962
1985
1940
2000
1962
1947
1959
1990
1955
1950
1948
1944
1963
Choice of Antibiotics
Identify the infecting organism
Evaluate drug sensitivity
Antibiotogram
Specific sensitivities of the organism
Target the site of infection
Drug safety/side effect profile
Selective toxicity: drugs that kill microorganisms but do not affect the host
DRUG INTERACTIONS
Patient factors
Age
Genetic or metabolic abnormalities
Renal or hepatic function
Mechanism of Action
Bacteria have their own enzymes for:
Cell wall formation
Protein synthesis
DNA replication
RNA synthesis
Synthesis of essential metabolites
Antibiotics target these sites
Minimal Inhibitory Concentration
(MIC)
Lowest concentration of antimicrobial that inhibits the growth of the organism after an
18 to 24 hour incubation period
Interpreted in relation to the specific antibiotic and achievable drug levels
Can not compare MICs between different antibiotics
Discrepancies between in vitro and in vivo
MIC
Time Above MIC
Effectiveness of beta-lactams, macrolides, clindamycin, & linezolid is optimal when the concentration of the antibiotics exceeds the
MIC of the organism for > 40% of the dosing interval at the site of the infection
Concentration Dependent Killing
Effectiveness of fluoroquinolones and aminoglycosides is greatest when peak levels of the drug are high
Peak/MIC ratios of > 8
Supports the idea of daily aminoglycoside dosing
Inhibitors of Cell Wall Synthesis
Penicillins
Penicillin G
Aminopenicillins
Penicillinase-resistant
Anti-pseudomonal
Cephalosporins
Monobactams
Carbapenems
Bacitracin
Vancomycin
Isoniazid
Ethambutol
Beta-Lactams
Beta-Lactams
Bactericidal
Inhibits synthesis of the mucopeptides in the cell wall of multiplying bacteria
Cell wall defects lead to lysis & death
Penicillins
Derived from the fungus Penicillum
Therapeutic concentrations in most tissues
Poor CSF penetration
Renal excretion
Side effects
Hypersensitivity (5% cross react with cephalosporins), nephritis, neurotoxicity, platelet dysfunction
Penicillins
Structure
Natural Penicillins
Active against Strep, some Staph,
Enterococcus, Neisseria, Actinomyces,
Listeria, Treponema
Bacteriocidal
Binds to & competitively inhibits the transpeptidase enzyme
Cell wall synthesis is arrested
Susceptible to penicillinase (beta-lactamase)
Side effects: hypersensitivity/anaphylaxis
Aminopenicillins
Ampicillin & amoxicillin
Effective against Strep, Enterococcus
Better penetration through the outer membranes of gram-negative bacteria & better binding to transpeptidase
Offer better coverage of gram-negative bacteria
H. influenza, Moraxella, E.coli, Proteus, Salmonella
First line therapy for otitis media/sinusitis
Still inhibited by penicillinase, therefore less effective against Staph
Aminopenicillins
Side effects: rash with mononucleosis infection
Semi-synthetic Penicillins
Penicillinase-resistant penicillins
Monobactams
Carbapenems
Extended-spectrum penicillins
Penicillins + beta-lactamase inhibitors
Penicillinase-Resistant Penicillins
Methicillin, nafcillin, oxacillin, cloxacillin, dicloxacillin
Gram-positive bacteria, particularly Staph
No activity against gram-negatives
These are the drugs of choice for Staph aureus when it is resistant to penicillin
Natural penicillins are more efficacious if the organism is penicillin sensitive
Anti-Pseudomonal Penicillins
Ureidopenicillins (piperacillin & mezlocillin)
Good gram-positive and gram-negative coverage
Including Pseudomonas & Citrobacter
Carboxypenicillins (ticarcillin & carbenicillin)
Less gram-positive coverage & more gramnegative coverage
Pseudomonas, Proteus, E. coli, Enterobacter,
Serratia, Salmonella, Shigella
Often used with aminoglycosides
Beta-Lactamase Inhibitors
Clavulanic acid, sulbactam, tazobactam
Enzymes that inhibit beta-lactamase
Clavulanic acid irreversibly binds beta-lactamase
Given in combination with penicillins
Augmentin = amoxicillin + clavulanic acid
Timentin = timentin + clavulanic acid
Unasyn = ampicillin + sulbactam
Zosyn = piperacillin + tazobactam
Cephalosporins
Semisynthetic beta-lactams
Beta-lactam ring that is more resistant to beta-lactamase
New R-group side chain: leads to drugs with different spectrums of activity
Cover a broad spectrum of gram-positive and negative organisms
Cephalosporinases
Enterococci and MRSA are resistant to cephalosporins
As the generation increases, penetration into the CSF increases
Side effects: 5-10% cross-reactivity with penicillins
Cephalosporins
Cefazolin Ceftriaxone
Cefuroxime Cefepime
Cephalosporin Generations
1 st generation
Cefadroxil (Duricef)
Cephalexin (Keflex)
Cefazolin (Kefzol)
2 nd generation
Cefaclor (Ceclor)
Cefuroxime (Ceftin)
Cefotetan
Cefoxitin (Mefoxin)
3 rd Generation
Ceftriaxone (Rocephin)
Cefotaxime (Claforan)
Cefdinir (Omnicef)
Cefixime (Suprax)
Ceftazidime (Fortaz)
4 th Generation
Cefepime (Maxipime)
Cephalosporin Generations
1 st
Strep, Staph, E. coli, Klebsiella, Proteus
Surgical ppx
2 nd
H. influenza, Moraxella, E. coli, Enterobacter, etc
Not as effective against S. aureus as 1 st gen.
3 rd
Gram negative> gram positive
Ceftriaxone: useful against meningitis
Ceftazidime is active against Pseudomonas
4 th
Active against MSSA , Strep, aerobic gram negatives including Pseudomonas
No Enterococcus or anaerobic coverage
Monobactams
Aztreonam
Beta-lactamase resistant
Has the beta-lactam ring with side groups attached to the ring.
Narrow spectrum of activity: only binds to the transpeptidase of gram-negative bacteria
Pseudomonas, E.coli, Klebsiella, Proteus
Ineffective against gram-positives & anaerobes
Can use in penicillin allergic patients
Carbapenems
Meropenem
Imipenem
Ertapenem
Broadest spectrum beta-lactam
Activity against gram-negatives, gram-positives, anaerobes
MSSA, Strep, Pseudomonas, Proteus, Klebsiella, Bacteroides
Resistance in MRSA , some Pseudomonas ,
Mycoplasma
Imipenem lowers the seizure threshold
Side effects: some PCN allergy cross-reactivity
Vancomycin
Covers nearly all gram-positive organisms
MRSA , coagulase-negative Staph, Enterococcus, highly resistant Strep pneumo
Leuconostoc resistant
Glycopeptide ( Streptomyces orientalis )
Inhibits synthesis of cell wall phospholipids & prevents cross-linking of peptidoglycans at an earlier step than beta-lactams
Also inhibits RNA synthesis
Synergy with aminoglycosides
Vancomycin
Not absorbed orally!
Poor CSF penetration
Not the drug of choice for MSSA
Delayed sterilization of blood infections
Drug levels
Peak = Toxicity (goal 25-40)
Trough = Efficacy (5-15)
Goal is to achieve drug levels above the MIC
Side effects: “red man syndrome”, neutropenia, renal and ototoxicity, phlebitis, fever, chills
Vancomycin
Protein Synthesis Inhibitors
Chloramphenicol, clindamycin, macrolides, aminoglycosides, tetracyclines
Bacterial cells depend on the continued production of proteins for growth and survival
Targets the bacterial ribosome
Bacterial – 70S (50S/30S)
Human – 80S (60S/40S)
Bacterial Ribosome 70S Particle
50S subunit (large)
Chloramphenicol
Lincosamides
(Clindamycin)
Oxazolidindones
(Linezolid)
Macrolides
30S subunit (small)
Tetracycline
Aminoglycosides
Lincosamides
Clindamycin
Gram-positive organisms & anaerobes
Inhibits protein synthesis by irreversibly binding to the
50S subunit
Poor CSF penetration
Good PO bioavailability
Side effects: C. difficile ( pseudomembraneous colitis)
Oxazolidinones
Linezolid
Broad gram-positive coverage (MRSA & VRE)
Prevents the formation of the 70S initiation complex of bacterial protein synthesis by binding to the 50S subunit at the interface with 30S subunit.
Bacteriostatic
Treatment of gram-positives including VRE & MRSA
Good PO bioavailability
Side effects: bone marrow suppression, lactic acidosis, headache, GI upset
Macrolides
Irreversibly bind the 50S subunit
Inhibits peptide bond formation
Erythromycin
Gram positives: MSSA , Strep, Bordetella, Treponema
Atypicals: Mycoplasma, Chlamydia, Ureaplasma
Clarithromycin
Similar to Erythromycin
Increased activity against gram negatives ( H. influenza,
Moraxella)
Azithromycin
Decreased activity against gram positives
Increased activity against H. influenza & Moraxella
Macrolides
Azithromycin structure
Side Effects
Oxidized by cytochrome P450
Leads to increased serum concentrations of theophylline, coumadin, digoxin, cyclosporin, etc.
Erythromycin
GI symptoms
Tetracyclines
Tetracycline, doxycycline
Bacteriostatic; Binds the 30S subunit
Spirochetes, Mycoplasma, Chlamydia, some grampositives & gram-negatives
Can chelate with milk products, Ca, & Mg
Side effects: phototoxic dermatitis, discolored teeth, renal & hepatic toxicity
Aminoglycosides
Streptomycin, gentamicin, tobramycin, amikacin
Binds to the 30S subunit, disrupting protein synthesis
Active against aerobic gram-negative organisms
E. coli, Proteus, Serratia, Klebsiella, Pseudomonas
Synergism for gram positive organisms with cell wall inhibitors because it leads to increased permeability of the cell
Side effects: CN VIII toxicity (hearing loss, vertigo), renal toxicity, neuromuscular blockade
Patients also on vancomycin are at higher risk of ototoxicity and nephrotoxicity
Aminoglycosides
Aminoglycosides
Concentration dependent due to active transport for uptake
Significant post-antibiotic effect
Drug levels
Peak = efficacy
Trough = toxicity (<2)
Inhibitors of Metabolism
Septra/Bactrim
Bacteria must synthesize folate to form cofactors for purines, pyrimidines, and amino acid synthesis
Gram-positives (including some MRSA), enteric gram negatives, Pneumocystis jiroveci, H. influenza,
Strep pneumo, Stenotrophomonas, Nocardia
Sulfomethoxazole & TMP act synergistically
Side effects: bone marrow suppression, anemia in those with G6PD deficiency, rashes
(photodermatitis; can lead to TEN)
Trimethoprim (TMP)
Dihydrofolate reductase inhibitor
Mimics dihydrofolate reductase of bacteria & competitively inhibits the reduction of folate into its active form, tetrahydrofolate (TH4)
Inhibiting bacterial DNA formation
Sulfonamides
Sulfamethoxazole, sulfasoxazole
Bacteriostatic
Inhibit bacterial folic acid synthesis by competitively inhibiting para amino benzoic acid (PABA)
Good penetration including CSF
Inhibitors of Nucleic Acid Synthesis &
Function
Fluoroquinolones
Rifampin
Fluoroquinolones
Ciprofloxacin, ofloxacin, levofloxacin, moxifloxacin
Synthetic derivative of nalidixic acid
Effective against gram positives and negatives, atypicals, Pseudomonas (cipro)
Decreased activity against anaerobes
Inhibit DNA gyrase, resulting in permanent DNA cleavage (bacteriocidal)
Concentration dependent killing
Great PO bioavailability
Wide distribution: CSF, saliva, bone/cartilage
Side effects: headache, nausea; damage cartilage in animals, Achilles tendonitis & rupture
Fluoroquinolones
Ciprofloxacin
Pseudomonas, H. influenza, Moraxella
Resistance in MRSA, Strep pneumo & pyogenes
Ciprofloxacin can inhibit GABA and cause seizures
Levofloxacin (Respiratory)
Strep, S. aureus (MRSA), H. influenza, atypicals
Levofloxacin & moxifloxacin have increased Staph coverage, including ciprofloxacin resistant strains
Used for otitis media, sinusitis, & pneumonia
Rifampin
Interacts with the bacterial DNA-dependent
RNA polymerase, inhibiting RNA synthesis
Mycobacterium, gram positives & negatives
Treats the carrier state in H. influenza and meningococcus
Resistance develops rapidly
May induce the cytochrome P450 system
Conclusion
Target antibiotic use for the patient and the organism you are treating
Know side effect profiles
Always check your antibiotic dosing and drug interactions
Questions & Comments
Resources
Hayley Gans MD & Kathleen Gutierrez, “Antibiotics
Overview” 2006
Prober, Long, & Pickering. Principles & Practice of
Pediatric Infectious Disease, 3 rd Edition
Centers for Disease Control
UpToDate 2007
The 2006 American Academy of Pediatrics Redbook
PREP American Academy of Pediatrics Questions
1999-2006