胃腸科標準病歷範本
advertisement

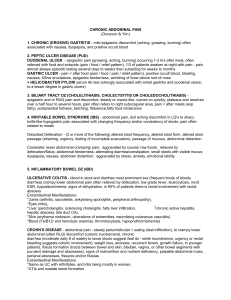
胃腸科標準病歷範本 一.【Acute cholecystitis】 Chief complaint: RUQ abdominal pain since ?(date) Present illness: This XX–year-old woman/man complained of abdominal pain for XX days. She/he had a similar experience of acute cholecystitis years ago. Her/his abdominal pain was located in the epigastrium/RUQ, dull and constant in nature, radiating to her back, and worsened after eating greasy foods. The pain was associated with vomiting.and mild fever. There was/wasn’t jaundice. She/he denied change in stool habit, chronic diarrhea and constipation. Besides, she/he denied chills, poor oral intake and recent weight loss. Under the impression of acute cholecystitis, she/he was admitted to GI ward for further evaluation and treatment. Past history: 1.Past medical history: # Cardiovascular disease - CAD, hyperlipidemia, hypertension, DM, stroke # Hepatitis B or C carrier # Current medications – NSAIDs, aspirin, steroids 2.Past surgical history: # no gastrectomy/colectomy/splenectomy Personal history # Smoking: ? PPD for years # Alcohol: type, amount, duration # Herbs used: denied # Occupation: ? # Travel history: denied # Animal exposure history: denied Family history: # No family history of hepatitis, diabetes mellitus, hypertension or malignancy Review of system: Constitutional: weakness(-), fatigue(-), fever(-), chills (-), cold sweating (-) body weight loss (-) Skin: pigmentation(-), jaundice(-), cyanosis(-), rashes(-), bruises(-), bulla (-) HEENT: a. b. c. d. e. Head--headache(-), dizziness(-), vertigo(-), syncope(-) Eyes--red eye(-), loss of vision(-), photophobia(-), pain(-) Nose--rhinorrhea(-), nasal congestion(-), postnasal drip(-) Ears--pain(-), discharge(-), hearing impairment(-), tinnitus(-) Mouth and throat--sore throat(-), hoarseness(-), oral ulcer(-) dysphagia(-), odynophagia(-) Respiratory system: cough(-), wheezing(-), dyspnea(-), chest tightness(-), hemoptysis(-), sputum (-) Cardiovascular system: dyspnea on exertion(-), paroxysmal nocturnal dyspnea(-),orthopnea (-), chest discomfort(-), palpitation(-) Gastrointestinal system: nausea(-), vomiting(-), heartburn(-), constipation(-), change of stool caliber(-), diarrhea(-) hematemesis(-), tarry stool/melena(-), bloody stool(-) abdominal pain(-), abdominal distension(-) Genitourinary system: dysuria(-), frequency(-), hematuria(-), nocturia(-), Foley catheter indwelling(-) Metabolic and endocrine system: moon face(-), central obesity(-), lower legs edema(-), heat/cold intolerance(-), polydipsia(-), polyuria(-), polyphagia(-) Neurological system: syncope(-), seizure(-), speech disturbance(-) numbness(-), weakness(-), ataxia(-), incontinence(-) Musculoskeletal system: low back pain(-), cramping(-), muscle atrophy(-), pain(-), swelling(-), intermittent claudication(-) Psychiatric: hallucination(-), delusions(-), anxiety (-), depression(-), agitation(-), suicide intention(-) Physical examination: Body weight: kg Body height: cm BMI: kg/m2 General appearance: well/fair/acute/chronic ill-looking Catherization: s/p endotracheal tube intubation/CVP insertion/ NG insertion, Foley catheterization Conscious level: alert, arousable, drowsy, coma GCS: EVM Skin: no icterus, no bruises/petechiae/ecchymosis, no spider angioma HEENT: pale/pink conjunctiva, no icteric sclera, pupil sizes(3.0mm, 3.0mm), light reflex(+/-, +/-) no injected throat, no oral ulcer Neck: supple, no enlarged thyroid gland, no jugular vein engorgement no lymphadenopathy Chest and lungs: symmetric and free expansion, no use of accessory muscles breath sounds – no rales/stridor/rhonchi/wheezing Heart: Regular/irregular heart beats, no murmurs, no S3 & S4 Abdomen: Inspection – flat/bulging/distended, no operation scar, no striae, no scratch marks, no bruises, no engorged veins Auscultation – normo/hypo/hyper-active bowel sounds, no bruits Palpation – no tenderness, no peritoneal signs (diffuse tenderness, muscle guarding, rebound pain), no Murphy’s sign, spleen: impalpable, Percussion – liver span: ( )cm over right middle clavicular line, tympanic, no shifting dullness Genitalia & digital rectal examination: no hemorrhoids, no palpable mass, normal anal tone, no blood stained on glove Extremities: warm/ cold, no pitting edema, no deformity no flapping tremor no loss of pulsation Muscle power: RUE-grade RLE-grade Neurological: no focal neurological deficits. Laboratory and image data: ; LUE-grade ; LLE-grade Impression: r/o Acute cholecystitis Plan: <Educational plan> - Consult dietitian - Educate patient about causes, complications, and management of acute cholecystitis <Diagnostic plan> Arrange abdominal echo Check bilirubin and lipase level. Follow up WBC/DC. <Therapeutic plan> - Hemodynamic plan: maintain adequate fluid intake intravenously. - Infection control: start empiric antibiotics after blood cultures. - Nutritional plan: NPO except water until symptoms improve - Others: arrange ERCP or MRCP if gallstones pancreatitis strongly suspected. Pain control and antiemetics Consult general surgeons. 二.【Acute pancreatitis】 Chief complaint: Epigastric pain for ? hours/days Present illness: This XX–year-old woman complained of abdominal pain occurred since XXXXX. She had a similar experience of acute pancreatitis XXX years ago. She has drunk alcohol over the last few days. Her abdominal pain was located in the epigastrium, dull and constant in nature, radiating to her back, relieved by sitting forward, but worsened lying down. It was/wasn’t related to food intake. The pain was associated with vomiting. She denied change in stool habit, chronic diarrhea and constipation. She also denied fever/chills, poor oral intake and recent weight loss. Under the impression of epigastric pain r/o acute pancreatitis, she was admitted to GI ward for further evaluation and treatment. Past history: 1.Past medical history: # Cardiovascular disease - CAD, hyperlipidemia, hypertension, DM, stroke # Hepatitis B or C carrier # Current medications – NSAIDs, aspirin, steroids 2.Past surgical history: # no gastrectomy/colectomy/splenectomy Personal history # Smoking: ? PPD for years # Alcohol: type, amount, duration # Herbs used: denied # Occupation: ? # Travel history: denied # Animal exposure history: denied Family history: # No family history of hepatitis, diabetes mellitus, hypertension or malignancy Review of system: Constitutional: weakness(-), fatigue(-), fever(-), chills (-), cold sweating (-) body weight loss (-) Skin: pigmentation(-), jaundice(-), cyanosis(-), rashes(-), bruises(-), bulla (-) HEENT: a. Head--headache(-), dizziness(-), vertigo(-), syncope(-) b. c. d. e. Eyes--red eye(-), loss of vision(-), photophobia(-), pain(-) Nose--rhinorrhea(-), nasal congestion(-), postnasal drip(-) Ears--pain(-), discharge(-), hearing impairment(-), tinnitus(-) Mouth and throat--sore throat(-), hoarseness(-), oral ulcer(-) dysphagia(-), odynophagia(-) Respiratory system: cough(-), wheezing(-), dyspnea(-), chest tightness(-), hemoptysis(-), sputum (-) Cardiovascular system: dyspnea on exertion(-), paroxysmal nocturnal dyspnea(-),orthopnea (-), chest discomfort(-), palpitation(-) Gastrointestinal system: nausea(-), vomiting(-), heartburn(-), constipation(-), change of stool caliber(-), diarrhea(-) hematemesis(-), tarry stool/melena(-), bloody stool(-) abdominal pain(-), abdominal distension(-) Genitourinary system: dysuria(-), frequency(-), hematuria(-), nocturia(-), Foley catheter indwelling(-) Metabolic and endocrine system: moon face(-), central obesity(-), lower legs edema(-), heat/cold intolerance(-), polydipsia(-), polyuria(-), polyphagia(-) Neurological system: syncope(-), seizure(-), speech disturbance(-) numbness(-), weakness(-), ataxia(-), incontinence(-) Musculoskeletal system: low back pain(-), cramping(-), muscle atrophy(-), pain(-), swelling(-), intermittent claudication(-) Psychiatric: hallucination(-), delusions(-), anxiety (-), depression(-), agitation(-), suicide intention(-) Physical examination: Body weight: kg Body height: cm BMI: kg/m2 General appearance: well/fair/acute/chronic ill-looking Catherization: s/p endotracheal tube intubation/CVP insertion/ NG insertion, Foley catheterization Conscious level: alert, arousable, drowsy, coma GCS: EVM Skin: no icterus, no bruises/petechiae/ecchymosis, no spider angioma HEENT: pale/pink conjunctiva, no icteric sclera, pupil sizes(3.0mm, 3.0mm), light reflex(+/-, +/-) no injected throat, no oral ulcer Neck: supple, no enlarged thyroid gland, no jugular vein engorgement no lymphadenopathy Chest and lungs: symmetric and free expansion, no use of accessory muscles breath sounds – no rales/stridor/rhonchi/wheezing Heart: Regular/irregular heart beats, no murmurs, no S3 & S4 Abdomen: Inspection – flat/bulging/distended, no operation scar, no striae, no scratch marks, no bruises, no engorged veins Auscultation – normo/hypo/hyper-active bowel sounds, no bruits Palpation – no tenderness, no peritoneal signs (diffuse tenderness, muscle guarding, rebound pain), no Murphy’s sign, spleen: impalpable, Percussion – liver span: ( )cm over right middle clavicular line, tympanic, no shifting dullness Genitalia & digital rectal examination: no hemorrhoids, no palpable mass, normal anal tone, no blood stained on glove Extremities: warm/ cold, no pitting edema, no deformity no flapping tremor no loss of pulsation Muscle power: RUE-grade RLE-grade Neurological: no focal neurological deficits. Laboratory and image data: Impression: r/o Acute pancreatitis ; LUE-grade ; LLE-grade Plan: <Educational plan> - Consult dietitian. - Educate patient about causes, complications, and management of acute pancreatitis. <Diagnostic plan> If symptoms worsened, or fever develops, need to arrange abdominal CT with contrast. - Follow ABGs if patient became dyspnea. - Check Triglycerides level. - Check Ranson’s score. <Therapeutic plan> - Hemodynamic plan: maintain adequate fluid intake intravenously and measure body weight. - Infection control: if fever occurred and abdominal pain worsened, start empiric antibiotics after blood cultures. - Nutritional plan: NPO except water and water only. - Others: arrange ERCP(or MRCP) if gallstones pancreatitis strongly suspected. Pain control. 三.【Cirrhosis】 Chief complaint: abdominal fullness for ( ) days Present illness: This XXX years old man has the history of 1._______; 2._______ ; and 3.__________. He complained of abdominal fullness for XXX days/months/years with [associated symptoms: fever/chills/ anemia/ jaundice/ conscious status/ nutrient status/ urine output/ stool pattern/ skin lesions/ bleeding tendency/ dizziness/ SOB/ abdominal pain/ appetite/ bowel habit change]. His abdominal examination showed shifting dullness. Under the impression of cirrhosis with (complications), he was admitted for further evaluation and treatment. Past history: 1.Past medical history: # Cardiovascular disease - CAD, hyperlipidemia, hypertension, DM, stroke # Hepatitis B or C carrier # Current medications – NSAIDs, aspirin, steroids 2.Past surgical history: # no gastrectomy/colectomy/splenectomy Personal history # Smoking: ? PPD for years # Alcohol: type, amount, duration # Herbal medication used: denied # Occupation: ? # Travel history: denied # Animal exposure history: denied Family history: # No family history of hepatitis, diabetes mellitus, hypertension or malignancy Review of system: Constitutional: weakness(-), fatigue(-), fever(-), chills (-), cold sweating (-) body weight loss (-) Skin: pigmentation(-), jaundice(-), cyanosis(-), rashes(-), bruises(-), bulla (-) HEENT: a. Head--headache(-), dizziness(-), vertigo(-), syncope(-) b. Eyes--red eye(-), loss of vision(-), photophobia(-), pain(-) c. Nose--rhinorrhea(-), nasal congestion(-), postnasal drip(-) d. Ears--pain(-), discharge(-), hearing impairment(-), tinnitus(-) e. Mouth and throat--sore throat(-), hoarseness(-), oral ulcer(-) dysphagia(-), odynophagia(-) Respiratory system: cough(-), wheezing(-), dyspnea(-), chest tightness(-), hemoptysis(-), sputum (-) Cardiovascular system: dyspnea on exertion(-), paroxysmal nocturnal dyspnea(-),orthopnea (-), chest discomfort(-), palpitation(-) Gastrointestinal system: nausea(-), vomiting(-), heartburn(-), constipation(-), change of stool caliber(-), diarrhea(-) hematemesis(-), tarry stool/melena(-), bloody stool(-) abdominal pain(-), abdominal distension(-) Genitourinary system: dysuria(-), frequency(-), hematuria(-), nocturia(-), Foley catheter indwelling(-) Metabolic and endocrine system: moon face(-), central obesity(-), lower legs edema(-), heat/cold intolerance(-), polydipsia(-), polyuria(-), polyphagia(-) Neurological system: syncope(-), seizure(-), speech disturbance(-) numbness(-), weakness(-), ataxia(-), incontinence(-) Musculoskeletal system: low back pain(-), cramping(-), muscle atrophy(-), pain(-), swelling(-), intermittent claudication(-) Psychiatric: hallucination(-), delusions(-), anxiety (-), depression(-), agitation(-), suicide intention(-) Physical examination: Body weight: kg Body height: cm BMI: kg/m2 General appearance: well/fair/acute/chronic ill-looking Catherization: s/p endotracheal tube intubation/CVP insertion/ NG insertion, Foley catheterization Conscious level: alert, arousable, drowsy, coma GCS: EVM Skin: no icterus, no bruises/petechiae/ecchymosis, no spider angioma HEENT: pale/pink conjunctiva, no icteric sclera, pupil sizes(3.0mm, 3.0mm), light reflex(+/-, +/-) no injected throat, no oral ulcer Neck: supple, no enlarged thyroid gland, no jugular vein engorgement no lymphadenopathy Chest and lungs: symmetric and free expansion, no use of accessory muscles breath sounds – no rales/stridor/rhonchi/wheezing Heart: Regular/irregular heart beats, no murmurs, no S3 & S4 Abdomen: Inspection – flat/bulging/distended, no operation scar, no striae, no scratch marks, no bruises, no engorged veins Auscultation – normo/hypo/hyper-active bowel sounds, no bruits Palpation – no tenderness, no peritoneal signs (diffuse tenderness, muscle guarding, rebound pain), no Murphy’s sign, spleen: impalpable, Percussion – liver span: ( ) cm over right middle clavicle line, tympanic, no shifting dullness Genitalia & digital rectal examination: no hemorrhoids, no palpable mass, normal anal tone, no blood stained on glove Extremities: warm/ cold, no pitting edema, no deformity no flapping tremor no loss of pulsation Muscle power: RUE-grade ; LUE-grade RLE-grade ; LLE-grade Neurological: no focal neurological deficits. Laboratory and image data: Impression: Cirrhosis Child-Pugh ( A B C ) score ( ) with ( complications) Plan: <Diagnostic plan> - Check Child Pugh score - Abdominal sonography for r/o hepatoma, portal hypertension or ascites. - Follow PES for varices and UGI bleeding. - If ascites present, do cultures and analysis. <Therapeutic plan> -Inderal for portal hypertension control - If fever is suspected, do blood and ascites cultures, consult infection doctor and empiric antibiotics use - EVL prevent further UGI bleeding - Duphalac prevent hepatic encephalopathy - Consider liver transplantation. <Educational plan> - Consult dietitian., low protein diet or low salt diet - Educate patient about causes, complications, and management of cirrhosis 四.【Colon cancer】 Chief complaint: Body weight loss for ( ) kg in ( duration) Present illness: This XXX-year-old woman has a history of 1._________ ; 2._______ ; 3._______ . She complained of weight loss of XXX kg for XXX days/weeks/months with [associated symptoms: fever/chills/ anemia/ nutrient status/ stool pattern/ bloody stool/ dizziness/ SOB/ abdominal pain/ appetite/ bowel habit change/ constipation/ diarrhea]. Her abdominal examination showed [palpable mass/ DRE: ?/ abdominal fullness/ tenderness). Under the impression of colon cancer, she was admitted for further evaluation and treatment. Past history: 1.Past medical history: # Cardiovascular disease - CAD, hyperlipidemia, hypertension, DM, stroke # Hepatitis B or C carrier # Current medications – NSAIDs, aspirin, steroids 2.Past surgical history: # no gastrectomy/colectomy/splenectomy Personal history # Smoking: ? PPD for years # Alcohol: type, amount, duration # Herbal medication used: denied # Occupation: ? # Travel history: denied # Animal exposure history: denied Family history: # No family history of hepatitis, diabetes mellitus, hypertension or (malignancy) Review of system: Constitutional: weakness(-), fatigue(-), fever(-), chills (-), cold sweating (-) body weight loss (-) Skin: pigmentation(-), jaundice(-), cyanosis(-), rashes(-), bruises(-), bulla (-) HEENT: a. Head--headache(-), dizziness(-), vertigo(-), syncope(-) b. Eyes--red eye(-), loss of vision(-), photophobia(-), pain(-) c. Nose--rhinorrhea(-), nasal congestion(-), postnasal drip(-) d. Ears--pain(-), discharge(-), hearing impairment(-), tinnitus(-) e. Mouth and throat--sore throat(-), hoarseness(-), oral ulcer(-) dysphagia(-), odynophagia(-) Respiratory system: cough(-), wheezing(-), dyspnea(-), chest tightness(-), hemoptysis(-), sputum (-) Cardiovascular system: dyspnea on exertion(-), paroxysmal nocturnal dyspnea(-),orthopnea (-), chest discomfort(-), palpitation(-) Gastrointestinal system: nausea(-), vomiting(-), heartburn(-), constipation(-), change of stool caliber(-), diarrhea(-) hematemesis(-), tarry stool/melena(-), bloody stool(-) abdominal pain(-), abdominal distension(-) Genitourinary system: dysuria(-), frequency(-), hematuria(-), nocturia(-), Foley catheter indwelling(-) Metabolic and endocrine system: moon face(-), central obesity(-), lower legs edema(-), heat/cold intolerance(-), polydipsia(-), polyuria(-), polyphagia(-) Neurological system: syncope(-), seizure(-), speech disturbance(-) numbness(-), weakness(-), ataxia(-), incontinence(-) Musculoskeletal system: low back pain(-), cramping(-), muscle atrophy(-), pain(-), swelling(-), intermittent claudication(-) Psychiatric: hallucination(-), delusions(-), anxiety (-), depression(-), agitation(-), suicide intention(-) Physical examination: Body weight: kg Body height: cm BMI: kg/m2 General appearance: well/fair/acute/chronic ill-looking Catherization: s/p endotracheal tube intubation/CVP insertion/ NG insertion, Foley catheterization Conscious level: alert, arousable, drowsy, coma GCS: EVM Skin: no icterus, no bruises/petechiae/ecchymosis, no spider angioma HEENT: pale/pink conjunctiva, no icteric sclera, pupil sizes(3.0mm, 3.0mm), light reflex(+/-, +/-) no injected throat, no oral ulcer Neck: supple, no enlarged thyroid gland, no jugular vein engorgement no lymphadenopathy Chest and lungs: symmetric and free expansion, no use of accessory muscles breath sounds – no rales/stridor/rhonchi/wheezing Heart: Regular/irregular heart beats, no murmurs, no S3 & S4 Abdomen: Inspection – flat/bulging/distended, no operation scar, no striae, no scratch marks, no bruises, no engorged veins Auscultation – normo/hypo/hyper-active bowel sounds, no bruits Palpation – no tenderness, no peritoneal signs (diffuse tenderness, muscle guarding, rebound pain), no Murphy’s sign, spleen: impalpable, Percussion – liver span: ( )cm over right middle clavical line, tympanic, no shifting dullness Genitalia & digital rectal examination: no hemorrhoids, no palpable mass, normal anal tone, no blood stained on glove Extremities: warm/ cold, no pitting edema, no deformity no flapping tremor no loss of pulsation Muscle power: RUE-grade ; LUE-grade RLE-grade ; LLE-grade Neurological: no focal neurological deficits. Laboratory and image data: Impression: conlon cancer Plan: <Diagnostic plan> - Colonosopy examination for tissue proof or lower GI series - Abdominal CT for tumor staging - Check CEA, albumin <Therapeutic plan> -consult GS if resection is indicated, or consult oncologist for CCRT - If not resection, consider chemotherapy - If advanced stage, discuss hospice care to patient and family. - Nutrient support - NPO if complete obstruction. <Educational plan> - Consult dietitian. - Educate patient about causes, complications, and management of bleeding/ obstruction 五.【Hepatoma】 Chief complaint: General weakness for XXXX days/weeks/months Present illness: This XXX-year-old woman has a history of 1._______, 2.______ ; 3.______. She complained of general weakness for XXX days/weeks/months with [associated symptoms: fever/chills/ anemia/ jaundice/ conscious status/ nutrient status/ urine output/ stool pattern/ skin lesions/ bleeding tendency/ dizziness/ SOB/ abdominal pain/ appetite/ bowel habit change/ body weight loss or not]. His abdominal examination showed [shifting dullness/ hepatomegaly/ splenomegaly/ jaundic/ lymphadenopathy]. Abdominal echo revealed a liver tumor, 5 mm in diameter in the [location]. Under the impression of hepatoma, she was admitted for further evaluation and treatment. Past history: 1.Past medical history: # Cardiovascular disease - CAD, hyperlipidemia, hypertension, DM, stroke # Hepatitis B or C carrier # Current medications – NSAIDs, aspirin, steroids 2.Past surgical history: # no gastrectomy/colectomy/splenectomy Personal history # Smoking: ? PPD for years # Alcohol: type, amount, duration # Herbal medication used: denied # Occupation: ? # Travel history: denied # Animal exposure history: denied Family history: # No family history of hepatitis, diabetes mellitus, hypertension or malignancy Review of system: Constitutional: weakness(-), fatigue(-), fever(-), chills (-), cold sweating (-) body weight loss (-) Skin: pigmentation(-), jaundice(-), cyanosis(-), rashes(-), bruises(-), bulla (-) HEENT: a. Head--headache(-), dizziness(-), vertigo(-), syncope(-) b. Eyes--red eye(-), loss of vision(-), photophobia(-), pain(-) c. Nose--rhinorrhea(-), nasal congestion(-), postnasal drip(-) d. Ears--pain(-), discharge(-), hearing impairment(-), tinnitus(-) e. Mouth and throat--sore throat(-), hoarseness(-), oral ulcer(-) dysphagia(-), odynophagia(-) Respiratory system: cough(-), wheezing(-), dyspnea(-), chest tightness(-), hemoptysis(-), sputum (-) Cardiovascular system: dyspnea on exertion(-), paroxysmal nocturnal dyspnea(-),orthopnea (-), chest discomfort(-), palpitation(-) Gastrointestinal system: nausea(-), vomiting(-), heartburn(-), constipation(-), change of stool caliber(-), diarrhea(-) hematemesis(-), tarry stool/melena(-), bloody stool(-) abdominal pain(-), abdominal distension(-) Genitourinary system: dysuria(-), frequency(-), hematuria(-), nocturia(-), Foley catheter indwelling(-) Metabolic and endocrine system: moon face(-), central obesity(-), lower legs edema(-), heat/cold intolerance(-), polydipsia(-), polyuria(-), polyphagia(-) Neurological system: syncope(-), seizure(-), speech disturbance(-) numbness(-), weakness(-), ataxia(-), incontinence(-) Musculoskeletal system: low back pain(-), cramping(-), muscle atrophy(-), pain(-), swelling(-), intermittent claudication(-) Psychiatric: hallucination(-), delusions(-), anxiety (-), depression(-), agitation(-), suicide intention(-) Physical examination: Body weight: kg Body height: cm BMI: kg/m2 General appearance: well/fair/acute/chronic ill-looking Catherization: s/p endotracheal tube intubation/CVP insertion/ NG insertion, Foley catheterization Conscious level: alert, arousable, drowsy, coma GCS: EVM Skin: no icterus, no bruises/petechiae/ecchymosis, no spider angioma HEENT: pale/pink conjunctiva, no icteric sclera, pupil sizes(3.0mm, 3.0mm), light reflex(+/-, +/-) no injected throat, no oral ulcer Neck: supple, no enlarged thyroid gland, no jugular vein engorgement no lymphadenopathy Chest and lungs: symmetric and free expansion, no use of accessory muscles breath sounds – no rales/stridor/rhonchi/wheezing Heart: Regular/irregular heart beats, no murmurs, no S3 & S4 Abdomen: Inspection – flat/bulging/distended, no operation scar, no striae, no scratch marks, no bruises, no engorged veins Auscultation – normo/hypo/hyper-active bowel sounds, no bruits Palpation – no tenderness, no peritoneal signs (diffuse tenderness, muscle guarding, rebound pain), no Murphy’s sign, spleen: impalpable, Percussion – liver span: () cm over right middle clavicle line, tympanic, no shifting dullness Genitalia & digital rectal examination: no hemorrhoids, no palpable mass, normal anal tone, no blood stained on glove Extremities: warm/ cold, no pitting edema, no deformity no flapping tremor no loss of pulsation Muscle power: RUE-grade ; LUE-grade RLE-grade ; LLE-grade Neurological: no focal neurological deficits. Laboratory and image data: Impression: Plan: Liver nodule, favor hepatoma <Diagnostic plan> - Check Child Pugh score - Abdominal CT for liver nodule D.D, and check BCLC stage. - Follow PES for varices and UGI bleeding. - If ascites with abdominal pain present, do cultures and analysis. - Check tumor markers, AFP, CEA, CA199 <Therapeutic plan> -consult GS if resection is indicated, or RFA/PEI if BCLC (A) - If not resection, consider TACE if BCLC (B) - If advanced stage, discuss hospice care to patient and family. - PES if UGI bleeding - Duphalac for hepatic encephalopathy <Educational plan> - Consult dietitian. - Educate patient about causes, complications, and management of hepatoma 六.【Jaundice】 Chief complaint: yellow skin and dark urine since? (date) Present illness: This is a 67-year-old man with no significant past medical history. He was admitted this time due to yellow skin and dark urine for xx days. Prior to the symptoms, he had experienced mild intermittent RUQ abdominal pain. He also noticed that his sclera became yellow. He denied abdominal pain, fever/chills, poor appetite, recent body weight loss, constipation or diarrhea. Under the impression of obstructive jaundice, he was admitted to GI ward for further evaluation and treatment. Past history: 1.Past medical history: # Cardiovascular disease - CAD, hyperlipidemia, hypertension, DM, stroke # Hepatitis B or C carrier # Current medications – NSAIDs, aspirin, steroids 2.Past surgical history: # no cholecystectomy/gastrectomy/colectomy/splenectomy Personal history # Smoking: ? PPD for years # Alcohol: type, amount, duration # Herbs used: denied # Occupation: ? # Travel history: denied # Animal exposure history: denied Family history: # No family history of hepatitis, diabetes mellitus, hypertension or malignancy Review of system: Constitutional: weakness(-), fatigue(-), fever(-), chills (-), cold sweating (-) body weight loss (-) Skin: pigmentation(-), jaundice(-), cyanosis(-), rashes(-), bruises(-), bulla (-) HEENT: a. Head--headache(-), dizziness(-), vertigo(-), syncope(-) b. c. d. e. Eyes--red eye(-), loss of vision(-), photophobia(-), pain(-) Nose--rhinorrhea(-), nasal congestion(-), postnasal drip(-) Ears--pain(-), discharge(-), hearing impairment(-), tinnitus(-) Mouth and throat--sore throat(-), hoarseness(-), oral ulcer(-) dysphagia(-), odynophagia(-) Respiratory system: cough(-), wheezing(-), dyspnea(-), chest tightness(-), hemoptysis(-), sputum (-) Cardiovascular system: dyspnea on exertion(-), paroxysmal nocturnal dyspnea(-),orthopnea (-), chest discomfort(-), palpitation(-) Gastrointestinal system: nausea(-), vomiting(-), heartburn(-), constipation(-), change of stool caliber(-), diarrhea(-) hematemesis(-), tarry stool/melena(-), bloody stool(-) abdominal pain(-), abdominal distension(-) Genitourinary system: dysuria(-), frequency(-), hematuria(-), nocturia(-), Foley catheter indwelling(-) Metabolic and endocrine system: moon face(-), central obesity(-), lower legs edema(-), heat/cold intolerance(-), polydipsia(-), polyuria(-), polyphagia(-) Neurological system: syncope(-), seizure(-), speech disturbance(-) numbness(-), weakness(-), ataxia(-), incontinence(-) Musculoskeletal system: low back pain(-), cramping(-), muscle atrophy(-), pain(-), swelling(-), intermittent claudication(-) Psychiatric: hallucination(-), delusions(-), anxiety (-), depression(-), agitation(-), suicide intention(-) Physical examination: Body weight: kg Body height: cm BMI: kg/m2 General appearance: well/fair/acute/chronic ill-looking Catherization: s/p endotracheal tube intubation/CVP insertion/ NG insertion, Foley catheterization Conscious level: alert, arousable, drowsy, coma GCS: EVM Skin: no icterus, no bruises/petechiae/ecchymosis, no spider angioma HEENT: pale/pink conjunctiva, no icteric sclera, pupil sizes(3.0mm, 3.0mm), light reflex(+/-, +/-) no injected throat, no oral ulcer Neck: supple, no enlarged thyroid gland, no jugular vein engorgement no lymphadenopathy Chest and lungs: symmetric and free expansion, no use of accessory muscles breath sounds – no rales/stridor/rhonchi/wheezing Heart: Regular/irregular heart beats, no murmurs, no S3 & S4 Abdomen: Inspection – flat/bulging/distended, no operation scar, no striae, no scratch marks, no bruises, no engorged veins Auscultation – normo/hypo/hyper-active bowel sounds, no bruits Palpation – no tenderness, no peritoneal signs (diffuse tenderness, muscle guarding, rebound pain), no Murphy’s sign, spleen: impalpable, Percussion – liver span: ( )cm over right middle clavicular line, tympanic, no shifting dullness Genitalia & digital rectal examination: no hemorrhoids, no palpable mass, normal anal tone, no blood stained on glove Extremities: warm/ cold, no pitting edema, no deformity no flapping tremor no loss of pulsation Muscle power: RUE-grade RLE-grade Neurological: no focal neurological deficits. Laboratory and image data: Impression; ; LUE-grade ; LLE-grade Plan: <Educational plan> - Consult dietitian <Diagnostic plan> Arrange abdominal echo Check serial bilirubin total and direct, GOT/GPT level. Check ALP, GGT level. Check hepatitis A/B/C serology. Follow up CEA, CA 199, and AFP if needed. <Therapeutic plan> - Hemodynamic plan: maintain adequate fluid intake intravenously. - Infection control: watch for Charcot’s triad (FEVER, ABDOMINAL PAIN, JAUNDICE). If present need to start empiric antibiotics after blood cultures - Nutritional plan: - Others: Arrange ERCP or MRCP if CBD obstruction is suspected. Arrange PTCD or PTGBD or ENBD if necessary. 七. LGI bleeding Chief complaint: Bloody stool/Brick stool passage for ( ) times for (duration). Present illness: This ( )–year-old man complained of blood–tinged/bloody stool passage since [date]. The volume of bloody stool was about ( ) ml per bowel movement and the frequency was XX times a day. He denied lower abdominal pain, change in stool habit or chronic diarrhea and constipation. He also denied fever/chills, poor oral intake and recent weight loss. Under the impression of lower gastrointestinal bleeding, he was admitted to GI ward for further evaluation and treatment. Past history: 1.Past medical history: # Cardiovascular disease - CAD, (hypertension, DM, stroke) # Hepatitis B or C carrier - denied # Malignancy and radiation history - denied # Current medications – NSAIDs, aspirin, corticosteroids 2.Past surgical history: # no gastrectomy/colectomy/splenectomy Personal history # Smoking: ? PPD for years # Alcohol: denied # Herbs used: denied # Occupation: ? # Travel history: denied # Animal exposure history: denied Family history: # No family history of malignancy Review of system: Constitutional: weakness(-), fatigue(-), fever(-), chills (-), cold sweating (-) body weight loss (-) Skin: pigmentation(-), jaundice(-), cyanosis(-), rashes(-), bruises(-), bulla (-) HEENT: a. Head--headache(-), dizziness(-), vertigo(-), syncope(-) b. c. d. e. Eyes--red eye(-), loss of vision(-), photophobia(-), pain(-) Nose--rhinorrhea(-), nasal congestion(-), postnasal drip(-) Ears--pain(-), discharge(-), hearing impairment(-), tinnitus(-) Mouth and throat--sore throat(-), hoarseness(-), oral ulcer(-) dysphagia(-), odynophagia(-) Respiratory system: cough(-), wheezing(-), dyspnea(-), chest tightness(-), hemoptysis(-), sputum (-) Cardiovascular system: dyspnea on exertion(-), paroxysmal nocturnal dyspnea(-),orthopnea (-), chest discomfort(-), palpitation(-) Gastrointestinal system: nausea(-), vomiting(-), heartburn(-), constipation(-), change of stool caliber(-), diarrhea(-) hematemesis(-), tarry stool/melena(-), bloody stool(-) abdominal pain(-), abdominal distension(-) Genitourinary system: dysuria(-), frequency(-), hematuria(-), nocturia(-), Foley catheter indwelling(-) Metabolic and endocrine system: moon face(-), central obesity(-), lower legs edema(-), heat/cold intolerance(-), polydipsia(-), polyuria(-), polyphagia(-) Neurological system: syncope(-), seizure(-), speech disturbance(-) numbness(-), weakness(-), ataxia(-), incontinence(-) Musculoskeletal system: low back pain(-), cramping(-), muscle atrophy(-), pain(-), swelling(-), intermittent claudication(-) Psychiatric: hallucination(-), delusions(-), anxiety (-), depression(-), agitation(-), suicide intention(-) Physical examination: Body weight: kg Body height: cm BMI: kg/m2 General appearance: well/fair/acute/chronic ill-looking Catherization: s/p endotracheal tube intubation/CVP insertion/ NG insertion, Foley catheterization Conscious level: alert, arousable, drowsy, coma GCS: EVM Skin: no icterus, no bruises/petechiae/ecchymosis, no spider angioma HEENT: pale/pink conjunctiva, no icteric sclera, pupil sizes(3.0mm, 3.0mm), light reflex(+/-, +/-) no injected throat, no oral ulcer Neck: supple, no enlarged thyroid gland, no jugular vein engorgement no lymphadenopathy Chest and lungs: symmetric and free expansion, no use of accessory muscles breath sounds – no rales/stridor/rhonchi/wheezing Heart: Regular/irregular heart beats, no murmurs, no S3 & S4 Abdomen: Inspection – flat/bulging/distended, no operation scar, no striae, no scratch marks Auscultation – normo/hypo/hyper-active bowel sounds, no bruits Palpation – no tenderness, no peritoneal signs (diffuse tenderness, muscle guarding, rebound pain), no Murphy’s sign, spleen: impalpable, Percussion – liver span: ( )cm over right middle clavicular line, tympanic, shifting dullness Genitalia & digital rectal examination: no hemorrhoids, no palpable mass, normal anal tone, no blood stained on glove Extremities: warm/ cold, no pitting edema, no deformity no flapping tremor no loss of pulsation Muscle power: RUE-grade RLE-grade Neurological: no focal neurological deficits. ; LUE-grade ; LLE-grade Laboratory and image data: Impression: (Lower gastrointestional bleeding related to colon tumor bleeding/hemorrhoidal bleeding/coagulopathy) Plan: <Diagnostic plan> - check Child’s score items if cirrhosis (albumin, bilirubin, ammonia, prothrombin time, consciousness level) - arrange abdominal echography and UGI endoscopy and colonoscopy - check CBC and coagulation profile <Therapeutic plan> - Hemodynamic support: on large bore intravenous catheter with adequate - crystalloids infusion if dehydration or low perfusion pressure Correct coagulopathy, thrombocytopenia and anemia Avoid ulcerogenic medicationss such as NSAIDs, aspirin, clopigodrel and - corticosteroids during active bleeding or preparation for LGI endoscopy. Nutritional plan: oral intake restriction with parenteral nutrition <Educational plan> - ? 八. UGI bleeding Chief complaint: Tarry stool for xx times since _________. Present illness: This XX- year-old woman has a major history of 1. cirrhosis with varices; 2. peptic ulcer disease; 3. CAD (or previous stroke with antiplatelet therapy/ chronic pain with NSAIDs treatment). She complained of tarry stools for XX days. She vomited XX times a day with bloody/coffee ground vomitus in volume about the size of a rice bowl. She also suffered from dizziness after vomiting/ passing tarry stools. She denied fever, chills, poor oral intake, and body weight loss. Under the impression of upper gastrointestinal bleeding, suspecting in relation to peptic ulcer disease or variceal bleeding, she was admitted to GI ward for further evaluation and treatment. Past history: 1.Past medical history: # Cardiovascular disease - CAD, (hypertension, DM, stroke) # Hepatitis B or C carrier - denied # Current medications – NSAIDs, aspirin, corticosteroids 2.Past surgical history: # no gastrectomy/colectomy/splenectomy Personal history # Smoking: ? PPD for years # Alcohol: denied # Herbs used: denied # Occupation: ? # Travel history: denied # Animal exposure history: denied Family history: # No family history of diabetes mellitus, hypertension or malignancy Review of system: Constitutional: weakness(-), fatigue(-), fever(-), chills (-), cold sweating (-) body weight loss (-) Skin: pigmentation(-), jaundice(-), cyanosis(-), rashes(-), bruises(-), bulla (-) HEENT: a. Head--headache(-), dizziness(-), vertigo(-), syncope(-) b. Eyes--red eye(-), loss of vision(-), photophobia(-), pain(-) c. Nose--rhinorrhea(-), nasal congestion(-), postnasal drip(-) d. Ears--pain(-), discharge(-), hearing impairment(-), tinnitus(-) e. Mouth and throat--sore throat(-), hoarseness(-), oral ulcer(-) dysphagia(-), odynophagia(-) Respiratory system: cough(-), wheezing(-), dyspnea(-), chest tightness(-), hemoptysis(-), sputum (-) Cardiovascular system: dyspnea on exertion(-), paroxysmal nocturnal dyspnea(-),orthopnea (-), chest discomfort(-), palpitation(-) Gastrointestinal system: nausea(-), vomiting(-), heartburn(-), constipation(-), change of stool caliber(-), diarrhea(-) hematemesis(-), tarry stool/melena(-), bloody stool(-) abdominal pain(-), abdominal distension(-) Genitourinary system: dysuria(-), frequency(-), hematuria(-), nocturia(-), Foley catheter indwelling(-) Metabolic and endocrine system: moon face(-), central obesity(-), lower legs edema(-), heat/cold intolerance(-), polydipsia(-), polyuria(-), polyphagia(-) Neurological system: syncope(-), seizure(-), speech disturbance(-) numbness(-), weakness(-), ataxia(-), incontinence(-) Musculoskeletal system: low back pain(-), cramping(-), muscle atrophy(-), pain(-), swelling(-), intermittent claudication(-) Psychiatric: hallucination(-), delusions(-), anxiety (-), depression(-), agitation(-), suicide intention(-) Physical examination: Body weight: kg Body height: cm BMI: kg/m2 General appearance: well/fair/acute/chronic ill-looking Catherization: s/p endotracheal tube intubation/CVP insertion/ NG insertion, Foley catheterization Conscious level: alert, arousable, drowsy, coma GCS: EVM Skin: no icterus, no bruises/petechiae/ecchymosis, no spider angioma HEENT: pale/pink conjunctiva, no icteric sclera, pupil sizes(3.0mm, 3.0mm), light reflex(+/-, +/-) no injected throat, no oral ulcer Neck: supple, no enlarged thyroid gland, no jugular vein engorgement no lymphadenopathy Chest and lungs: symmetric and free expansion, no use of accessory muscles breath sounds – no rales/stridor/rhonchi/wheezing Heart: Regular/irregular heart beats, no murmurs, no S3 & S4 Abdomen: Inspection – flat/bulging/distended, no operation scar, no striae, no scratch marks Auscultation – normo/hypo/hyper-active bowel sounds, no bruits Palpation – no tenderness, no peritoneal signs (diffuse tenderness, muscle guarding, rebound pain), no Murphy’s sign, spleen: impalpable, Percussion – liver span: ( )cm over tight middle clavicular line, tympanic, shifting dullness Genitalia & digital rectal examination: no hemorrhoids, no palpable mass, normal anal tone, no blood stained on glove Extremities: warm/ cold, no pitting edema, no deformity no flapping tremor no loss of pulsation Muscle power: RUE-grade ; LUE-grade RLE-grade Neurological: no focal neurological deficits. Laboratory and image data: Impression ; LLE-grade Plan: <Diagnostic plan> - check Child’s score items if cirrhosis (albumin, bilirubin, ammonia, prothrombin time, consciousness) - arrange abdominal echography and UGI endoscopy - check CBC and coagulation profile <Therapeutic plan> - Hemodynamic support: on large bore intravenous catheter with adequate crystalloids infusion if dehydration or low perfusion pressure - Correct coagulopathy, thrombocytopenia and anemia - Avoid ulcerogenic medications such as NSAIDS, aspirin, clopidogrel and corticosteroids during active bleeding. Intravenous proton pump inhibitors infusion if indicated - Nutritional plan: oral intake restriction with parenteral nutrition - <Educational plan> - Avoid ulcerogenic over-the-counter medications 九. Variceal bleeding Chief complaint: Bloody vomitus/tarry stool passage for ( ) times (duration) Present illness: This XX–year-old man has a major history of cirrhosis with varices or peptic ulcer disease, CAD or stroke with antriplatelet therapy or chronic pain with NSAIDs treatment. He complained of tarry stools for XX days. She vomited XX times a day with bloody/coffee ground vomitus in volume about the size of a rice bowl. She also suffered from dizziness after vomiting/ passing tarry stools. She denied fever, chills, poor oral intake, abdominal pain and fullness, body weight loss. Under the impression of upper gastrointestinal bleeding, suspecting in relation to peptic ulcer disease or variceal bleeding, he was admitted to GI ward for further evaluation and treatment. Past history: 1.Past medical history: # Cardiovascular disease - CAD, (hypertension, DM, stroke) # Hepatitis B or C carrier - denied # Current medications – NSAIDs, aspirin, corticosteroids 2.Past surgical history: # no gastrectomy/colectomy/splenectomy Personal history # Smoking: ? PPD for years # Alcohol: denied # Herbs used: denied # Occupation: ? # Travel history: denied # Animal exposure history: denied Family history: # No family history of diabetes mellitus, hypertension or malignancy Review of system: Constitutional: weakness(-), fatigue(-), fever(-), chills (-), cold sweating (-) body weight loss (-) Skin: pigmentation(-), jaundice(-), cyanosis(-), rashes(-), bruises(-), bulla (-) HEENT: a. Head--headache(-), dizziness(-), vertigo(-), syncope(-) b. Eyes--red eye(-), loss of vision(-), photophobia(-), pain(-) c. Nose--rhinorrhea(-), nasal congestion(-), postnasal drip(-) d. Ears--pain(-), discharge(-), hearing impairment(-), tinnitus(-) e. Mouth and throat--sore throat(-), hoarseness(-), oral ulcer(-) dysphagia(-), odynophagia(-) Respiratory system: cough(-), wheezing(-), dyspnea(-), chest tightness(-), hemoptysis(-), sputum (-) Cardiovascular system: dyspnea on exertion(-), paroxysmal nocturnal dyspnea(-),orthopnea (-), chest discomfort(-), palpitation(-) Gastrointestinal system: nausea(-), vomiting(-), heartburn(-), constipation(-), change of stool caliber(-), diarrhea(-) hematemesis(-), tarry stool/melena(-), bloody stool(-) abdominal pain(-), abdominal distension(-) Genitourinary system: dysuria(-), frequency(-), hematuria(-), nocturia(-), Foley catheter indwelling(-) Metabolic and endocrine system: moon face(-), central obesity(-), lower legs edema(-), heat/cold intolerance(-), polydipsia(-), polyuria(-), polyphagia(-) Neurological system: syncope(-), seizure(-), speech disturbance(-) numbness(-), weakness(-), ataxia(-), incontinence(-) Musculoskeletal system: low back pain(-), cramping(-), muscle atrophy(-), pain(-), swelling(-), intermittent claudication(-) Psychiatric: hallucination(-), delusions(-), anxiety (-), depression(-), agitation(-), suicide intention(-) Physical examination: Body weight: kg Body height: cm BMI: kg/m2 General appearance: well/fair/acute/chronic ill-looking Catherization: s/p endotracheal tube intubation/CVP insertion/ NG insertion, Foley catheterization Conscious level: alert, arousable, drowsy, coma GCS: EVM Skin: no icterus, no bruises/petechiae/ecchymosis, no spider angioma HEENT: pale/pink conjunctiva, no icteric sclera, pupil sizes(3.0mm, 3.0mm), light reflex(+/-, +/-) no injected throat, no oral ulcer Neck: supple, no enlarged thyroid gland, no jugular vein engorgement no lymphadenopathy Chest and lungs: symmetric and free expansion, no use of accessory muscles breath sounds – no rales/stridor/rhonchi/wheezing Heart: Regular/irregular heart beats, no murmurs, no S3 & S4 Abdomen: Inspection – flat/bulging/distended, no operation scar, no striae, no scratch marks Auscultation – normo/hypo/hyper-active bowel sounds, no bruits Palpation – no tenderness, no peritoneal signs (diffuse tenderness, muscle guarding, rebound pain), no Murphy’s sign, spleen: impalpable, Percussion – liver span: ( ) cm over right middle clavicular line, tympanic, shifting dullness Genitalia & digital rectal examination: no hemorrhoids, no palpable mass, normal anal tone, no blood stained on glove Extremities: warm/ cold, no pitting edema, no deformity no flapping tremor no loss of pulsation Muscle power: RUE-grade RLE-grade Neurological: no focal neurological deficits. Laboratory and image data: ; LUE-grade ; LLE-grade Impression: (Esophageal/Gastric variceal bleeding) Plan: <Diagnostic plan> - check Child’s score items if cirrhosis (albumin, bilirubin, ammonia, prothrombin time, consciousnesss level) - arrange abdominal echography and UGI endoscopy - check CBC and coagulation profile <Therapeutic plan> - Hemodynamic support: on large-bore intravenous catheter with adequate crystalloids infusion if dehydration or low perfusion pressure - Correct coagulopathy, thrombocytopenia and anemia Avoid ulcerogenic medicationss such as NSAIDs, aspirin, clopidogrel and corticosteroids during active bleeding. Intravenous Somatosan or Glypressin if indicated Nutritional plan: oral intake restriction with parenteral nutrition Transfer to ICU if hemodynamic instability and compromised airway <Educational plan> - maintain regular stool habits with laxatives. - Limited intake of excess protein to avoid hepatic encephalopathy 十、Diarrhea Chief complaint: Frequent watery/mucoid/oily diarrhea for ( ) days Present illness: This ( )–year-old woman has the history of 1)________, 2)__________, 3)________; she had been admitted to receive antibiotic treatment with ( ) for ( ) days then discharged ( ) days ago. She complained of watery/mucoid/oily/rice-water diarrhea with frequent small/large amount of stool with blood tinged/ mucin content for ____ days. She also suffered from abdominal discomfort/pain in the right/left upper/lower abdomen occasionally. Her diarrhea improved/didn’t improve with fasting. Besides, fever/chills was/were noted yesterday/xx days ago, accompanied with spinning sensation/weakness/poor appetite. The patient denied cough/sputum, nausea/vomiting, hunger pain, post-prandial fullness, melena, dysuria or any family members or office coworkers with the same symptom. Under the impression of diarrhea and suspected infective colitis r/o inflammatory bowel disease, the patient was admitted to GI ward for further evaluation and treatment. Past history: 1.Past medical history: # Cardiovascular disease - (hypertension,CAD,DM,stroke) under medical control # Hepatitis B or C carrier - denied # Immune compromised disease - (Cancer, DM, HIV infection) # Liver cirrhosis # Gouty arthritis # Current medications – 2.Past surgical history: # no gastrectomy/colectomy/cholecystectomy Personal history # Smoking: ? PPD for ? years # Alcohol: Beer/whisky/rice wine/wine ? cups/bottles for ? years # Herbs used: denied # Raw food intake: denied # Occupation: ? # Travel history: denied # Animal exposure history: denied # Sexual history: denied homosexual tendency Family history: # No family history of diabetes mellitus, hypertension or malignancy Review of system: Constitutional: weakness( ), fatigue( ), fever( ), chills ( ), cold sweating ( ), night sweating ( ), body weight loss () Skin: pigmentation(-), jaundice(-), cyanosis(-), rashes(-), bruises(-), bulla (-) HEENT: a. Head—headache(-), dizziness( ), vertigo(-), syncope( ) b. Eyes--red eye(-), loss of vision(-), photophobia(-), pain(-) c. Nose--rhinorrhea(-), nasal congestion(-), postnasal drip(-) d. Ears--pain(-), discharge(-), hearing impairment(-), tinnitus(-) e. Mouth and throat—sore throat(-), hoarseness(-), oral ulcer(-), dysphagia(-), odynophagia(-) Respiratory system: cough(-), wheezing(-), dyspnea(-), chest tightness(-), hemoptysis(-), sputum (-) Cardiovascular system: dyspnea on exertion(-), paroxysmal nocturnal dyspnea(-),orthopnea (-), chest discomfort(-), palpitation(-) Gastrointestinal system: nausea( ), vomiting( ), heartburn( ), constipation( ), change of stool caliber( ), diarrhea(+), hematemesis(-), tarry stool/melena(-), bloody stool(-) abdominal pain( ), abdominal distension( ) Genitourinary system: dysuria(-), frequency(-), hematuria(-), nocturia(-), Foley catheter indwelling(-) Metabolic and endocrine system: moon face(-), central obesity(-), lower legs edema(-), heat/cold intolerance(-), polydipsia(-), polyuria(-), polyphagia(-) Neurological system: syncope(-), seizure(-), speech disturbance(-), numbness(-), weakness(-), ataxia(-), incontinence(-) Musculoskeletal system: low back pain(-), cramping(-), muscle atrophy(-), pain(-), swelling(-), intermittent claudication(-) Psychiatric: hallucination(-), delusions(-), anxiety (-), depression(-), agitation(-), suicide intention(-) Physical examination: Body weight: kg Body height: cm BMI: kg/m 2 General appearance: well/fair/acute/chronic ill-looking Conscious level: alert, arousable, drowsy, coma GCS: EVM Skin: no icterus, no bruises/petechiae/ecchymosis, no spider angioma HEENT: pale/pink conjunctiva, no icteric sclera, pupil sizes(3.0mm, 3.0mm), light reflex(+/-, +/-) no injected throat, no oral ulcer Neck: supple, no enlarged thyroid gland, no jugular vein engorgement no lymphadenopathy Chest and lungs: symmetric and free expansion, no use of accessory muscles breath sounds – no rales/stridor/rhonchi/wheezing Heart: Regular/irregular heart beats, no murmurs, no S3 & S4 gallops Abdomen: Inspection – flat/bulging/distended, no operation scar, no striae, no scratch marks Auscultation – normo/hypo/hyper-active bowel sounds, no bruits Palpation – tenderness ( ) at ----, muscle guarding ( ), rebound pain( ), no Murphy’s sign, Spleen: impalpable Percussion – liver span: about ( ) cm over right mid-clavicular line, tympanic, shifting dullness ( ) Genitalia & digital rectal examination: no hemorrhoids, no palpable mass, normal anal tone, no blood stained on glove Extremities: warm/ cold, no pitting edema, no deformity no flapping tremor no loss of pulsation Muscle power: RUE-grade ; LUE-grade RLE-grade ; LLE-grade Neurological: no focal neurological deficits. Laboratory and image data: Plan: <Diagnostic plan> - check stool routine, collect specimens for stool culture if infective colitis is likely - check CBC and electrolytes , as well as lipid profile - Check stool Na and K to estimate fecal osmotic gap [290 - 2(Na+K)stool] - arrange abdominal sonography; and/or colonoscopy if IBD is suspected - Check serum amebiasis antibody if amebiasis can not be ruled out <Therapeutic plan> - Hemodynamic support: adequate hydration for volume repletion - Correct electrolyte imbalance - Prescribe antidiarrheal agents such like Kaopectin for symptomatic treatment or Questran (Cholestyramine) for bile related diarrhea Avoid excessive laxative, antacid, digitalis or colchicine medication. Nutritional plan: Light diet for enteral nutrition if tolerated, unless consider NPO and prescribe parenteral nutrition <Educational plan> - Hand-washing habit can prevent most infection - Suggest enteral nutrition with smaller amount meals, avoid too oily food and may try low fiber, soft and light diet Early medical treatment if acute diarrhea persisted, particularly when fever/chills occurred 十一、Dysphagia Chief complaint: Difficulty in swallowing for ( ) days Present illness: This ( )–year-old woman/man has the history of 1) __________, 2)___________ , 3) ________. The patient had received radiotherapy for nasopharyngeal cancer for ( ) months. She/He has suffered from difficulty in swallowing for ( ) days. She/He stated that she/he had no problem eating solid foods at all before, but recently difficulty in swallowing and sensation of something stuck in throat were noted. She/He could slowly swallow with liquid, but frequent choking and cough occurred. There was no painful sensation following swallowing, but body weight loss of ( ) kgs in last ( ) months was mentioned. The patient denied headache, dizziness, muscle weakness, palpitation, dyspnea, nausea/vomiting, tarry stool, abdominal pain, night sweating or any recent trauma. Under the impression of suspected esophageal stricture, probably malignancy related, the patient was admitted to GI ward for further evaluation and treatment. Past history: 1.Past medical history: # Cardiovascular disease - (hypertension,CAD,DM,stroke) under medical control # Hepatitis B or C carrier - denied # Current medications – 2.Past surgical history: # Personal history # Smoking: ? PPD for ? years # Alcohol: Beer/whisky/rice wine/wine ? cups/bottles for ? years # Betel nuts: denied # Herbs used: denied # Occupation: ? # Travel history: denied # Animal exposure history: denied Family history: # No family history of diabetes mellitus, hypertension or malignancy Review of system: Constitutional: weakness( ), fatigue( ), fever( ), chills ( ), cold sweating ( ), night sweating ( ), body weight loss () Skin: pigmentation(-), jaundice(-), cyanosis(-), rashes(-), bruises(-), bulla (-) HEENT: a. Head—headache(-), dizziness(-), vertigo(-), syncope(-) b. Eyes--red eye(-), loss of vision(-), photophobia(-), pain(-) c. Nose--rhinorrhea(-), nasal congestion(-), postnasal drip(-) d. Ears--pain(-), discharge(-), hearing impairment(-), tinnitus(-) e. Mouth and throat—sore throat( ), hoarseness( ), oral ulcer( ), dysphagia(+), odynophagia( ) Respiratory system: cough( ), wheezing(-), dyspnea( ), chest tightness(-), hemoptysis(-), sputum (-) Cardiovascular system: dyspnea on exertion(-), paroxysmal nocturnal dyspnea(-),orthopnea (-), chest discomfort(-), palpitation(-) Gastrointestinal system: nausea( ), vomiting( ), heartburn(-), constipation( ), change of stool caliber( ), diarrhea( ), hematemesis(-), tarry stool/melena(-), bloody stool(-) abdominal pain( ), abdominal distension( ) Genitourinary system: dysuria(-), frequency(-), hematuria(-), nocturia(-), Foley catheter indwelling(-) Metabolic and endocrine system: moon face(-), central obesity(-), lower legs edema(-), heat/cold intolerance( ), polydipsia(-), polyuria(-), polyphagia(-) Neurological system: syncope(-), seizure(-), speech disturbance(-), numbness(-), weakness(-), ataxia(-), incontinence(-) Musculoskeletal system: low back pain(-), cramping(-), muscle atrophy(-), pain(-), swelling(-), intermittent claudication(-) Psychiatric: hallucination(-), delusions(-), anxiety (-), depression(-), agitation(-), suicide intention(-) Physical examination: Body weight: kg Body height: cm BMI: kg/m 2 General appearance: well/fair/acute/chronic ill-looking Conscious level: alert, arousable, drowsy, coma GCS: EVM Skin: no icterus, no bruises/petechiae/ecchymosis, no spider angioma HEENT: pale/pink conjunctiva, no icteric sclera, no ptosis pupil sizes(3.0mm, 3.0mm), light reflex(+/-, +/-) no injected throat, no oral ulcer Neck: supple, no enlarged thyroid gland, no jugular vein engorgement Lymphadenopathy ( ) Chest and lungs: symmetric and free expansion, no use of accessory muscles breath sounds – clear/rales/stridor/rhonchi/wheezing , bilateral Heart: Regular/irregular heart beats, no murmurs, no S3 & S4 gallops Abdomen: Inspection – flat/bulging/distended, no operation scar, no striae, no scratch marks Auscultation – normo/hypo/hyper-active bowel sounds, no bruits Palpation – no tenderness, no muscle guarding, no rebound pain, no Murphy’s sign, Spleen: impalpable Percussion – liver span: ( ) cm over right mid-clavicular line, tympanic, no shifting dullness Genitalia & digital rectal examination: no hemorrhoids, no palpable mass, normal anal tone, no blood stained on glove Extremities: warm/ cold, no pitting edema, no deformity no flapping tremor no loss of pulsation Muscle power: RUE-grade ; LUE-grade RLE-grade ; LLE-grade Neurological: no focal neurological deficits. Laboratory and image data: Plan: <Diagnostic plan> - Arrange CXR to evaluate if any existence of bronchial carcinoma, consider neck sonography if throid tumor is suspected - Arrange Neck to Chest computed tomography and UGI endoscopy to evaluate if any obstructive lesions - Check CBC and electrolytes - Check serum glucose, lipid profile included HbA1C - Consider arrangement of brain computed tomography if acute stroke is likely - Consider arrangement of NCV+EMG if myathenia gravis is suspected <Therapeutic plan> - NG feeding if easy choking, to prevent aspiration pneumonia - Correct electrolyte imbalance and adequate hydration, as well as prokinetic agent and in case of GERD prescribe PPI medication - Treat underlying disease and consider esophageal dilatation if favored esophageal stricture - Arrange gastrostomy / jejunostomy if (nearing) total obstruction of esophagus Arrange rehabilitation programm Nutritional plan: High protein, low fat and high fiber soft diet if tolerated, unless NPO with parenteral nutritional support <Educational plan> - Encourage enteral nutrition, education about feeding at upright position and keep 30 minutes after meal to prevent aspiration pneumonia - No talking with food/liquid in mouth, slow swallowing and place food on dominant side of mouth by patients with CVA Heimlich maneuver if choking and emergent medical/surgical treatment is needed 十二、Ileus Chief complaint: Persistent abdominal fullness for ( ) days Present illness: This ( )–year-old woman/man has the history of 1) ________, 2) ______,3) _______. She/he complained of persistent abdominal fullness for ( ) days. The sensation of abdominal fullness is diffuse but occurred more often postprandially; sometimes it was accompanied with nausea/vomiting and frequent belching/hiccup. Besides, the patient mentioned history of chronic constipation and lack of flatulence. The patient denied body weight loss, night sweating, tenesmus, abdominal pain, back pain, tea color urine, gray color stool or melena. Under the impression of ileus, r/o ( ) obstruction, the patient was admitted to GI ward for further evaluation and treatment. Past history: 1.Past medical history: # Cardiovascular disease - (hypertension,CAD,DM,stroke) under medical control # Hepatitis B or C carrier - denied # Current medications – 2.Past surgical history: # Prior abdominal or spinal surgery: Personal history # Smoking: ? PPD for ? years # Alcohol: Beer/whisky/rice wine/wine ? cups/bottles for ? years # Herbs used: denied # Occupation: ? # Travel history: denied # Animal exposure history: denied Family history: # No family history of diabetes mellitus, hypertension or malignancy Review of system: Constitutional: weakness(-), fatigue(-), fever(-), chills (-), cold sweating (-), night sweating (-), body weight loss (-) Skin: pigmentation(-), jaundice(-), cyanosis(-), rashes(-), bruises(-), bulla (-) HEENT: a. Head—headache(-), dizziness(-), vertigo(-), syncope(-) b. Eyes--red eye(-), loss of vision(-), photophobia(-), pain(-) c. Nose--rhinorrhea(-), nasal congestion(-), postnasal drip(-) d. Ears--pain(-), discharge(-), hearing impairment(-), tinnitus(-) e. Mouth and throat—sore throat(-), hoarseness(-), oral ulcer(-), dysphagia(-), odynophagia(-) Respiratory system: cough(-), wheezing(-), dyspnea(-), chest tightness(-), hemoptysis(-), sputum (-) Cardiovascular system: dyspnea on exertion(-), paroxysmal nocturnal dyspnea(-),orthopnea (-), chest discomfort(-), palpitation(-) Gastrointestinal system: nausea( ), vomiting( ), heartburn(-), constipation( ), change of stool caliber( ), diarrhea( ), hematemesis(-), tarry stool/melena(-), bloody stool(-) abdominal pain( ), abdominal distension( ) Genitourinary system: dysuria(-), frequency(-), hematuria(-), nocturia(-), Foley catheter indwelling(-) Metabolic and endocrine system: moon face(-), central obesity(-), lower legs edema(-), heat/cold intolerance(-), polydipsia(-), polyuria(-), polyphagia(-) Neurological system: syncope(-), seizure(-), speech disturbance(-), numbness(-), weakness(-), ataxia(-), incontinence(-) Musculoskeletal system: low back pain(-), cramping(-), muscle atrophy(-), pain(-), swelling(-), intermittent claudication(-) Psychiatric: hallucination(-), delusions(-), anxiety (-), depression(-), agitation(-), suicide intention(-) Physical examination: Body weight: kg Body height: cm BMI: kg/m2 General appearance: well/fair/acute/chronic ill-looking Conscious level: alert, arousable, drowsy, coma GCS: EVM Skin: no icterus, no bruises/petechiae/ecchymosis, no spider angioma HEENT: pale/pink conjunctiva, no icteric sclera, pupil sizes(3.0mm, 3.0mm), light reflex(+/-, +/-) no injected throat, no oral ulcer Neck: supple, no enlarged thyroid gland, no jugular vein engorgement no lymphadenopathy Chest and lungs: symmetric and free expansion, no use of accessory muscles breath sounds – no rales/stridor/rhonchi/wheezing Heart: Regular/irregular heart beats, no murmurs, no S3 & S4 gallops Abdomen: Inspection – flat/bulging/distended, no operation scar, no striae, no scratch marks Auscultation – normo/hypo/hyper-active bowel sounds, no bruits Palpation – tenderness ( ) at ----, muscle guarding ( ), rebound pain( ), no Murphy’s sign, Spleen: impalpable Percussion – liver span: ( ) cm over right mid-clavicular line, tympanic, shifting dullness ( ) Genitalia & digital rectal examination: no hemorrhoids, no palpable mass, normal anal tone, no blood stained on glove Extremities: warm/ cold, no pitting edema, no deformity no flapping tremor no loss of pulsation Muscle power: RUE-grade ; LUE-grade RLE-grade ; LLE-grade Neurological: no focal neurological deficits. Laboratory and image data: Plan: <Diagnostic plan> - Arrange KUB, abdominal sonography and consider further computed tomography, GI serie to rule out any obstructive lesions - Check CBC and electrolytes , and hormonal studies included thyroid hormon - Check serum glucose, lipid profile included HbA1C - Arrange UGI/LGI endoscopy if no peritoneal sign and after informed consent patient about risks of perforation - Follow EKG to evaluate if any arrythmia - Sepsis workup <Therapeutic plan> - NG decompression and/or free drainage if obstruction is likely - Hemodynamic support: adequate hydration to improve the perfusion - Correct electrolyte imbalance - Prescribe prokinetic agents and stool softner or enema - Avoid excessive opioid agents; and treat underlying disease such liked hypothyroidism. - Nutritional plan: High protein, low fat and high fiber diet if tolerated, unless NPO with parenteral nutritional support <Educational plan> - DM and diet control with low fat, high fiber nutrition - Regular exercise and defecation habit and avoid mis-used laxative or enema Early medical/surgical treatment if acute abdominal pain occurred