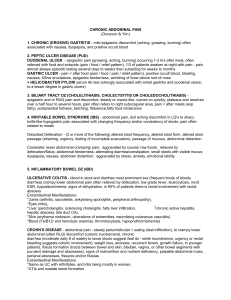
Abdominal Assessment
advertisement

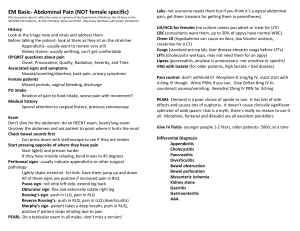
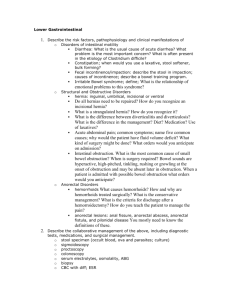
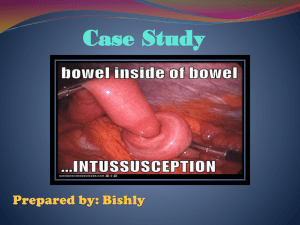
Created by: Nicole Anderson MN, NP Presented by: Jennifer Burgess RN, GNC(C) 1. 2. 3. 4. Overview of anatomy Abdominal assessment technique Interpretation of findings Constipation, fecal impaction, and bowel obstruction 5. When to report findings 1. Abdominal quadrants 2. Landmarks/surface anatomy 3. Abdominal muscles 4. Abdominal vasculature 5. Internal organs •Dividing the abdomen into 4 quadrants will aid during assessment and will allow for appropriate documentation of findings. •Understanding which organs are relevant to each quadrant will help you to determine etiology of signs/symptoms found during assessment. Understanding landmarks and surface anatomy will enhance your documentation skills and will allow for more efficient reporting of symptoms. •Function to support abdominal cavity and protect organs •Weakness in these muscles may lead to hernias, inability to cough effectively, increased risk of falls, abdominal distension, postural problems, and back pain. Liver: bile production, controls levels of fats/amino acids/proteins in the blood, immune function, detoxification, metabolizes drugs, blood clotting, store sugars, etc. Gallbladder: aids in fat digestion and concentrates/stores bile produced by the liver. Pancreas: produces digestive enzymes, secretes insulin/glucagon/somatostatin to control blood sugar levels Spleen: stores and produces lymphocytes Small intestine: digestion and absorption of nutrients, approximately 21 feet long. Large intestine: absorption of water, lubrication of contents, neutralization of acids, decomposition by live bacteria, approximately 4.5-5 feet long and 2.5 inches in diameter. RUQ: liver, gallbladder, duodenum, hepatic flexure of colon, head of pancreas, right kidney/ureter, part of ascending and transverse colon RLQ: cecum, appendix, small intestine, right ureter, right ovary/fallopian tube, right spermatic cord LUQ: stomach, spleen, splenic flexure of colon, tail of pancreas, left kidney/ureter, part of transverse and descending colon LLQ: sigmoid colon, small intestine, part of descending colon, left ovary/fallopian tube, left spermatic cord 1. Resident should be calm and supine 2. Bring a stethoscope 3. An understanding of health history or reported symptoms is useful 4. Obtain relevant history from resident 1. 2. 3. 4. Inspection Auscultation Percussion Palpation 1. Observe resident’s abdomen from foot of bed for peristalsis, asymmetry, and abdominal distension 2. Observe umbilicus for deviation 3. Assess skin of abdomen 4. Measure abdominal girth if relevant 1. Start in RLQ and listen to each quadrant for 2-5 minutes for bowel sounds 2. Normal sounds are high-pitched and gurgling in small intestine and lowpitched and rumbling in the colon 3. Normally occur at a rate of 5-35/min 1. 2. 3. 4. Percuss all quadrants for dullness Percuss for tympany Percuss for hyperresonance Percuss for bladder volume 1. With warm hands lightly palpate all 4 quadrants- palpate any area of pain last 2. Use pads of fingers depressing abdomen 1cm 3. Moderate palpation may be done to assess musculature and deeper structure Asymmetry: enlarge spleen or liver Distension: fat, flatus, stool, fluid, tumor Bruising at umbilicus: acute necrotizing pancreatitis Flank bruising: intra-abdominal or retroperitoneal hemorrhage, or injury to pancreas Periumbilical and flank ecchymosis Very loud bowel sounds: hyperperistalsis caused by diarrhea or early intestinal obstruction. High-pitched tinkles and rushes: bowel obstruction Absence or decreased: paralytic ileus, peritonitis, or acute abdomen Dullness: normal over liver and spleen, but abnormal in mid abdomen and may be due to organ distension or mass Pain: inflammation Tympany: high-pitched tympany suggests distension Hyperresonance: normal at umbilicus, but anywhere else suggests distended vasculature or aneurysms Crepitus: subcutaneous emphysema suggests abscess, diverticulitis, or organ perforation. Pain: many causes such as peritonitis, inflammation, abscess Mass/Ridge: depending on the area, could mean tumor, aneurysm, abscess. Infrequent or difficult passage of stool, hard stool, or a feeling of incomplete evacuation •Difficulty passing stool •Hardened stool •Complaints of rectal fullness •Self disimpaction •hemorrhoids •Symptoms are often un-noticed in the older adult and frequency of stools may not change •Distended tympanic abdomen •Vomiting •Blood in stool •Weight loss •Severe constipation of recent onset/worsening in older adults A large lump of hard dry stool that remains stuck in the rectum, often due to chronic constipation •Abdominal cramping and bloating •Leakage of liquid from rectum or diarrhea in a resident with chronic constipation •Rectal bleeding •Small, semi-formed stools •Difficulty passing stool and/or straining •Nausea and vomiting •Tachypnea •Tachycardia •Abdominal distension with tympanic, absent and/or high-pitched bowel sounds Significant mechanical impairment for complete blockage of contents through the intestine. Mechanical obstruction can effect either the small or large intestine. Small bowel obstruction: •Cramping around umbilicus or epigastrium •Vomiting •Obstipation •Hyperactive, high-pitched bowel sounds with rushes •Diarrhea in partial obstruction Large bowel obstruction: •More gradual onset of symptoms •Increasing constipation leading to obstipation and abdominal distension •Lower abdominal cramping unproductive of feces •Loud, hyperactive bowel sounds •Symptoms are mild •Severe steady pain •Tender with light palpation •Absent bowel sounds •Shock (tachycardia, low BP) •Oliguria •Fever/chills, or abnormal vital signs •Rectal bleeding •Older adults •Presence of red flags •Any abnormal finding on abdominal exam •Suspected intestinal obstruction •Change in bowel patterns, stool consistency, stool colour •Change in nutritional status •Suspected constipation or fecal impaction •Acute abdominal pain