Open
advertisement

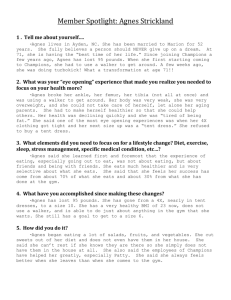
ASP level 3 case studies Adults Support and Protection (Scotland) Act 2007 Implementation Programme Group Exercises -- Questions and Case Studies Two Day Training Course Day One Programme Morning -- Session One Principles and Definitions Group Exercise 1 Group members should introduce themselves and say what agency they come from and what their post title is. The group should identify a chair, and a person to write the flipchart list and to report back in the plenary feedback session. The group task is to consider: What are the implications, challenges and dilemmas in professional practice from the definitions of 'adult at risk' and 'harm'? Use post-its on an individual basis to note words and phrases about the definition of ' an adult at risk' and the definition of 'harm' and then share these within the group to create a group list on the flipchart. Identify cases on an anonymous basis, which illustrate the dilemmas and challenges. Please flipchart your examples and comments. Inquiries - Co-operation - Advocacy and Other Services Group Exercise 2 Case Examples Agnes Agnes lives with her husband Ian in a ground floor flat. She has multiple sclerosis and anxiety states. A couple of years ago her health deteriorated and now she cannot walk very far. The only time Agnes goes out is when she attends a luncheon club twice a week. Both an OT and a home care worker have been involved for some time. There have been concerns in the past when Agnes has said he has not got any money left. She has never said where the money has gone. Service staff see very little of Ian, who seems to spend a lot of his time out of the house. There are often empty bottles of spirits in the house -- Agnes does not drink alcohol -- and old betting slips left lying around. During an assessment visit, Ian did say he did what he could for Agnes, but he had worked all his life and paid his taxes and it was up to services to provide what support she needed. Agnes has never been critical of him, and always seems highly anxious to keep things in order in case he gets angry with her. Agnes's doctor has been called out by a neighbour, who had heard Agnes shouting for help through the wall. When the neighbour went in she found Agnes crying and saying she was starving. She had not eaten for three days. She seemed to be extremely dehydrated and cried out when the neighbour touched her arm. Her neighbour helped her to the toilet, and Agnes said it was painful to pass urine. The neighbour phoned the health centre, but by the time the doctor visited Ian had returned home, said his wife was fine and they did not need any help. The doctor was only able to see Agnes very briefly, when she said she was fine and did not need any help or want anyone else involved. In this case is there a duty to inquire? Is there a duty of cooperation, and what might be the issues concerning cooperation in this case? What other factors and services may need to be considered, and in what circumstances might advocacy be appropriate? How should staff and agencies deal with the dilemmas concerning self-determination and reporting concerns raised in operational practice? Please flipchart your examples and comments. Investigations - Visits - Interviews Group Exercise 3 David David, who has learning disabilities, mobility problems and a severe hearing impairment, was admitted to hospital having sustained a head injury. The meals on wheels person found him unconscious and called an ambulance. Over the past 6 months, David has had numerous admissions with falls, fractures and unexplained major bruising. David says he has become clumsy lately, but no physical evidence has yet been established as a cause. A range of social care, health and housing services have been involved with David over a number of years. At present, David's support includes domestic help, housing support, meals on wheels and a treatment involving a district nurse. After being discharged, as the nurse was changing a dressing, David disclosed to her that his son had actually caused the injury as well as the previous injuries. David went on to say his son had a drugs problem and became physically violent towards him on pension days, when he refused to give him more money. He insisted the nurse keep this information confidential as he did not wish his son to get into trouble. How do the legislative principles, definitions, and the legal powers and duties in relation to visits, interview and warrants for entry relate to the case study? What issues are raised about confidentiality and consent, and how should they be dealt with, both in this case and more broadly in operational practice? What other dilemmas and challenges are posed in this case, and what next steps should be taken? Discuss in your groups and flipchart your examples. Adults in Managed Service Settings Group Exercise 4 Ermina Ermina is a Scottish-Asian woman, who has lived in Scotland for many years. She has a number of physical and mental health issues and her behaviour can be quite difficult at times. She has lived in a registered care setting for about a year. Staff are struggling to manage her behaviour and a social worker is involved in reviewing her care needs. The social worker is unhappy with the staff's attitude to her client. Another registered service has assessed Ermina, with a view to her moving to their specialist service. However, in their assessment, Ermina does not need such a specialist unit. The Care Commission also has a number of concerns about her present service. Ermina's cousin visits regularly, and has now reported to the social worker that as she arrived for her last visit she saw one of the staff angrily pushing Ermina along the corridor and saying to her, " I told you -- you can't come along here - you people never learn". The Senior officer later told the cousin about an accident that had happened to Ermina a few days before leaving bruising down one arm - it was not a very convincing explanation, but Ermina was not able to tell her cousin what had happened. The cousin also expressed concern that Ermina never seemed to have much left from her weekly income. Identify the implications of the Adult Support and Protection Act in this case in relation to medical examinations and the examination of records, and any other relevant considerations. Then, identify more broadly issues concerning implementing the legislation when this concerns managed social care, health or housing settings. Discuss in your groups and flipchart your examples. Serious Harm, Consent and Undue Pressure Group Exercise 5 Serious Harm How would you distinguish 'harm' from 'serious harm' within the context of the Adult Support and Protection Act? Use post-its individually for five minutes to note personal words and phrases identifying what would constitute serious harm, and then in 10 minutes create a group list after sharing and discussing these ideas. Undue Pressure The ASP Act allows consent to be dispensed with in certain circumstances and with evidence of 'undue pressure'. Use post-its individually for five minutes to note personal words and phrases identifying what you believe would constitute an evidence 'undue pressure' and any issues concerning this concept, and then in 10 minutes create a group list after sharing these ideas.Assessment Orders and Removal Orders Group Exercise 6 Identify cases in which the use of an Assessment order or a Removal order would have been of benefit to an adult at risk. Then create a group list with two columns noting the circumstances in which an Assessment order or a Removal order would have had such benefits. You may also wish to note the potential difficulties and drawbacks of using orders in these circumstances.Banning Orders