Despite continuing improvements in infant health
advertisement

Folate, Folic Acid, and Health
Table of contents
Executive summary
Purpose
1
Introduction
2
Neural tube defects
2
Neural tube defects and folate/folic acid
3
Response by agencies in the USA
5
Response in other countries
6
Other health outcomes affected by folic acid
birth defects
cancers
cardiovascular disease
other health outcomes
9
9
10
12
Epidemiology of NTDs in NZ
burden of NTDs in NZ
cost of NTDs in NZ
13
14
16
The NZ response to folic acid research
19
Folate intake of New Zealanders
sources of folate
22
24
Methods for enhancing folate levels in the population
diet
supplementation
use of supplements
sales and availability of folic acid tablets
knowledge about folate/folic acid and neural tube defects
fortification
cost effectiveness of folic acid fortification
fortification of foods in NZ
health claims
knowledge about fortification in NZ
26
27
27
30
37
40
40
41
44
44
-
level of fortification
upper target level for folate
Dietary modelling
46
48
48
53
Risks from increasing folic acid intake
Potential toxic effects from folic acid
multiple births and other reproductive outcomes
vitamin B12 deficiency
zinc
other potential risks
53
54
55
56
Monitoring health outcomes and folate levels in NZ
monitoring NTDs and other birth defects
monitoring folate levels
57
57
58
Impact of folic acid supplementation and fortification policies
59
Conclusion
60
References
64
Appendices
1.
Folate intake and B12 masking (reprint)
72
2.
Vitamin B12 deficiency and the fortification of food with folic
acid (reprint)
76
Authors and Acknowledgements
The report was originally produced in late 1999 by Dr Barry Borman,
Epidemiologist, Health Funding Authority, with assistance from Sheldon Brown,
to examine the relationship between folate, folic acid and health outcomes.
The report was peer-reviewed by Professor Godfrey Oakley (Emory University,
Atlanta, USA), who was a constant source of encouragement and enthusiasm
during the writing of the report, and Associate Professor Boyd Swinburn (The
National Heart Foundation, Auckland).
Other major contributors to the report were: Professor Nicholas Wald (Wolfson
Institute of Preventive Medicine, London, England), Dr Christopher Howson and
Dr Donald Mattison (March of Dimes, White Plains, USA), Dr David Erickson
(Centers for Disease Control and Prevention, Atlanta, USA), Dr Carol Bower
(Western Australian Birth Defects Register, Perth, Australia), Jenny Reid
(Australia and New Zealand Food Authority (ANZFA), Wellington), Kay Winegar
(IMS Health, Auckland), Dr Pat Tuohy, (Child Health Adviser, Ministry of Health,
Wellington), and Geoff Tempest, Professor Bob Elliott, Lyall Thurston, and Rex
Jensen, of the Folate Replenishment-Plus Committee
Executive Summary
Conclusions
Current scientific evidence fully supports the health benefits of fortifying
breads with folic acid
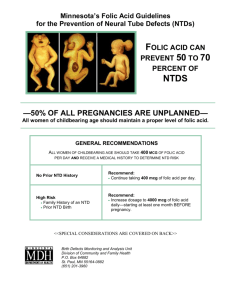
There is clear evidence that periconceptional consumption of adequate
amounts of folate/folic acid prevents NTDs. There is accumulating research
that the risk of other birth defects and health outcomes is also reduced by
folic acid
The Food Regulations permit the voluntarily fortification of bread with folic
acid up to the level of 285mg/100g
There is no current scientific evidence of toxic effects from consuming too
much folic acid – via any diet, supplementation, or fortification
NZ women in the reproductive age group have low levels of folate
It is extremely unlikely that individuals in NZ will consume an excess of folic
acid either through diet, supplementation or fortification
the neural tube defects (NTDs), anencephaly and spina bifida, are the second
leading contributors to the health burden from birth defects
in the early 1980s two studies in England and Wales indicated that the risk of
NTDs could be reduced by periconceptional supplementation with vitamins,
including the B-vitamin, folic acid. Subsequent research in a number of
countries generally supported the finding
in 1992 two randomised control trials showed that folic acid supplementation
reduced the risk of NTD recurrence and occurrence. The Centres for Disease
Control and Prevention in the USA recommended that all potentially pregnant
women should consume 0.4mg of folic acid every day. Women at higher risk
(e.g., those who previously had an infant with a NTD) were advised to
consume 4mg per day
similar recommendations have made in a number of other jurisdictions (e.g.,
Australia, Canada, England and Wales)
Other health outcomes
recent research has indicated that folic acid may also reduce the risk of other
birth defects, including facial clefts and congenital heart disease
there is also increasing evidence that folic acid may reduce the risk from
cardiovascular disease and some forms of cancer
Methods to increase folate levels
three mechanisms are available to increase folate to levels which prevent
NTDs: fortification, supplementation, and diet
fortification is the primary mechanism for improving the folate status of
women in the population. Accordingly, the FDA in the US mandated that from
January 1998 all grain products had to be fortified with synthetic folic acid.
Canada has adopted a similar approach and other countries are also
proposing to regulate for the mandatory fortification of staple products, such
as bread, with folic acid
supplements are an effective method to get 400mcg of folic acid, but advising
women to take tablets during pregnancy is contrary to ‘normal’ practice, many
pregnancies are unplanned, and NTDs are formed (i.e., the first 28 days of
gestation) before many women are aware they are pregnant
it is extremely difficult for women to raise their level of folate sufficiently
through eating folate rich foods alone. Natural folate that occurs in food is less
stable than synthetic folic acid, and has a lower bioavailability
NTDs in New Zealand
the epidemiology of NTDs shows that like a number of other countries (e.g.,
England and Wales, USA), the rate of these defects has been declining since
the mid-1970s
There is no evidence of marked differences in the risk for Maori and nonMaori, or associations with socioeconomic status, maternal age, and parity
NZ generally has a low -moderate rate of NTDs with the rate similar to
Australia, Western Australia and parts of the USA
Folate recommendation in NZ
The Public Health Commission advised NZ women in 1994 to consume 5mg
of folic acid to reduce the risk of NTDs as well as improve their diet by
consuming folate rich vegetables. The level of supplementation was the
highest recommended by any country.
In 1996, the Ministry of Health revised their recommendation to 0.8mg of folic
acid because of the advent of a low dose tablet.
Folate status of NZ women
The 1997 NZ Nutrition Survey found that the usual daily median intake of
folate from food was 278mcg for males and 212 mcg for females. People
living in the most deprived areas (NZDep96) and young females are likely to
have inadequate intakes of folate. Half of the NZ population used vitamin and
/or mineral supplements during the previous year, with the highest use among
NZ European and Others and females 19-24 years.
Another recent study found that at month 4 of their pregnancy, 49% of the
women had folate intakes less than two thirds of the Australian RDI for
pregnant women at month 4 of their pregnancy. It is not known if these levels
are similar to the levels during the periconceptional period and early stages of
pregnancy. Almost half of the European women had taken folic acid
supplements in the year before their pregnancy, compared to 10% for Maori
and Pacific Island women.
Dietary modelling of folic acid
NZ data from the Australian New Zealand Food Authority (ANZFA) indicates
that it is highly unlikely that the intake of folic acid would exceed 1000mcg on
a regular basis for any age-sex group.
Toxic levels of folic acid consumption
Current research shows there are no known toxic effects from the ingestion of
folic acid either by diet, supplementation or fortification.
Another concern expressed against fortification is the potential of folic acid to
mask B12 vitamin deficiency. However, a recent publication from the
American Institute of Medicine states that ‘clear evidence of folic acid-induced
neurotoxicity in humans is lacking’. Nonetheless, it is advocated that the
relationship between folic acid and B12-deficiency is considered in developing
a tolerable upper intake level for folic acid intake.
there is no relationship between increasing levels of folic acid intake and
multiple births, and adverse effects with zinc, anticonvulsants, oral
contraceptives
Monitoring of health outcomes and folate levels
The NZ Birth Defects Monitoring Programme continues to monitor the
prevalence of birth defects, including NTDs, among live and stillbirths and is
participating to two international studies to monitor the effect of folic acid
recommendations and fortification
The Department of Nutrition, University of Otago, has completed a
programme to collect data on folate intake and blood folate levels among
women aged 20-44 years and men aged 14-19 years.
‘One of the most exciting medical findings of the last part of the 20th
century is that folic acid, a simple, widely available, water-soluble
vitamin, can prevent spina bifida and anencephaly (SBA). Not since
the rubella vaccine became available 30 years ago have we had a
comparable opportunity for primary prevent of such common and
serious birth defects.’1
Introduction
Although many aspects of infant health continue to show improvement in a
number of developed and developing countries, birth defects remain major
causes of infant mortality and morbidity. For example, in New Zealand the infant
mortality rate between 1987 and 1996 declined from 10.1 per 1,000 livebirths to
7.3 per 1,000 livebirths. However, the proportion of infant deaths due to birth
defects remained at 24%.
In 1995, birth defects were the cause of 8% of infant hospitalisations, and in
1996, 19% of all fetal deaths. Results from the NZ Burden of Disease study
(NZBDS)2 show that 15% of the total disability (DALYS) i in the 0-14 year age
group were attributable to birth defects. Various perinatal conditions, respiratory
conditions, and injury respectively accounted for 23%, 21%, and 13% of the
disease burden in this age group. More than 80% of the burden from birth
defects in the 0-14 year age group is borne by 0-4 year olds.
The neural tube defects (NTDs) are a major group of birth defects. In 1996, 18%
of perinatal deaths (stillbirths and livebirths dying in the first 7 days of life) were
due to NTDs, compared to 15% attributable to congenital heart defects.
Anencephaly and spina bifida comprise 90% of all NTD cases.
Anencephaly is characterised by the total or partial absence of the cranial vault,
the covering skin, and the brain missing or reduced to small mass. Most infants
with anencephaly are stillborn and those that are liveborn usually die within hours
of birth. Anencephaly often occurs in association with spina bifida.
Spina bifida is a family of defects in the closure of the spinal column
characterised by herniation or exposure of the spinal cord and/or meninges
through an incompletely closed spine. Most infants with spina bifida are liveborn
and many have associated birth defects (e.g., hydrocephalus, facial clefts).
i
A DALY (the ‘disability-adjusted life year’) represents the loss of one year of healthy life and is the sum
of years lost to premature mortality and years lost to (severity-adjusted) disability - see reference 2 for a full
description
Folate, Folic Acid, and Health
1
Encephalocele, often also included under the term ‘neural tube defects’, is
characterized by herniation of the brain and /or meninges through a defect in the
skull. In this paper, ‘neural tube defects’ only includes anencephaly and spina
bifida.
NTDs occur in the first 28 days of pregnancy, often before a mother knows she is
pregnant.
Neural Tube Defects
NTDs have been the subject of a plethora of research because they are gross
malformations, usually have a high level of ascertainment, and have major
impacts on infant health.
The increasing use of antenatal diagnosis and screening over the last decade
has resulted in considerable progress in the secondary control of NTDs. Progress
in the primary prevention of the defects has been hampered by the lack of
aetiological clues emerging from the research. Many studies of NTDs suffer from
methodological problems (e.g., the lack of multiple case ascertainment and
adjustment for the effect of possible confounding factors, using prevalence rather
than incidence data).3 4
A major handicap of much of the research is that it is based on prevalence at
birth rates rather than incidence data. To establish incidence rates it would be
necessary to know the fate of all conceptuses5 Therefore, the effect of
spontaneous abortions and terminations of pregnancy (TOPs) is generally not
known, although increasingly attempts are being made to include these data in
studies and monitoring programmes.
The general epidemiological pattern of NTDs shows (see Elwood et al, 1992
for a complete review of the literature):
6
distinct international and intranational geographic patterns of prevalence. The
UK has traditionally reported the highest international rates, but recent data
indicates areas in India, China 7, and the Middle East also have high rates.
There are low to medium rates in most areas of Europe, USA, Australia, and
NZ. In England and Wales, rates are higher in the north and west, and in
North America on the east coast
in many developed countries the decline in the rates of NTDs since the mid1970s has not always accounted for by the impact of terminations of
pregnancy
there are weak and inconsistent seasonal patterns in prevalence at birth rates
Folate, Folic Acid, and Health
2
high rates have traditionally been reported for Caucasian populations while
black populations have low rates
no causative factor has been identified in reported clusters of NTDs
an inverse relationship between the male proportion of anencephaly cases
and the prevalence rate, but only a small female predominance for spina
bifida
in areas with high prevalence rates, the rates are highest in the lowest socioeconomic categories (irrespective of how socio-economic status is measured)
when maternal age and parity effects exist they are usually U-shaped
A number of aetiological factors have been investigated in relation to NTDs, but
many of the studies have methodological problems (e.g., recall and
ascertainment bias, difficulty in establishing levels of exposure). However:
no, or inconsistent, associations have been reported with tea drinking,
caffeine, potato consumption, recreational drugs, smoking, alcohol, maternal
infections, hyperthermia, occupational exposures (e.g., visual display
terminals, pesticides, solvents, plastics), various chemical elements in
drinking water
pregnancies exposed to the anti-convulsant drugs, valproic acid and
carbamazepine have a higher risk of NTDs
Following an initial review of the literature, Elwood et al 8 concluded that many of
the epidemiological patterns of NTDs (e.g., social class gradient, secular and
seasonal trends, and some geographic variation) may have dietary determinants.
The authors concluded that ‘one of the more viable specific hypotheses is that of
folic acid deficiency although certain epidemiological features of neural-tube
defects clearly are not explained by this mechanism.’
NTDs and Folate/Folic Acid
In 1965 Hibbard and Smithells9 found that 69% of mothers who delivered a NTD
affected infant had folate deficiency compared to 17% of mothers with normal
children (mothers were matched by age, parity, time of conception and
gestation). A later study reported that mothers who gave birth to infants with
NTDs had lower mean first trimester levels of serum folate and red cell folate
than controls.10
In the UK in the early 1980s, a non-randomised trial by Smithells 11 12 and a small
randomised trial by Laurence 13 14 found the recurrence risk of NTDs was
Folate, Folic Acid, and Health
3
reduced with supplementation by multivitamins, which included folic acid (table 1).
However, the impact of these results was overshadowed by criticisms of the
methodologies used in the studies.6 15 16
Subsequently, in the mid to late 1980s a number of case-control, cohort, and
non-randomised intervention studies also reported a reduced risk of NTDs after
periconceptional supplementation with multivitamins and/or folic acid.17 18 19 20 21
22 The one notable exception was the case-control study by Mills et al 23 in
California and Illinois which showed no effect of supplementation on the risk of
NTDs (tables 1 & 2).
In July 1991 the results from a British Medical Research Council funded
multicentre randomised control trial were published showing that high-dose folic
acid supplements (4.0 mg per day) used by women who had a previously NTDaffected pregnancy reduced the risk of having a subsequent NTD-affected
pregnancy by 70% 24 (table 1).
In December 1992, Czeizel and Dudas 25 reported that in a randomised trial in
Hungary the occurrence risk of NTDs was reduced with the use of 0.8mg per day
of folic acid with other vitamins (table 1).
Table 1: Randomised and non-randomised intervention trials of the use of vitamin supplements
and NTD risk
Trial/study
Place
Recurrence (R)
Occurrence (O)
Folic acid (FA) Daily dose of
Multivitamin
FA
(MV)
supplement
(mg)
Relative
95%
risk confidence
interval
Randomised controlled trials
Laurence et al (1981)
South Wales
R
FA
4
0.42
0.04-2.97
MRC Vitamin Study
Research Group (1991)
International
R
FA
4
0.29
0.10-0.74
Czeizel & Dudas (1992)
Hungary
O
M
0.8
0.00
0.00-0.85
Kirke et al (1992)
Ireland
R
FA
0.36
0.00
0.00-10.0
0.24
0.11-0.52
0.36
0.14
0.03-0.47
5
0.00
0.00-2.13
0.12
0.04-0.41
Combined
Non-randomised trials
Smithells et al (1980, 1983) UK, several
centres
R
M
Vergel et al (1990)
R
FA
Cuba
Combined
source: Adapted from:
Wald,35
CDC,38
Folate, Folic Acid, and Health
Elwood,26
NHMRC,27
4
and respective studies
Table 2: Observational studies of vitamin supplementation and NTD risk
Study
Folic acid (FA)
multivitamin (MV)
supplement
Relative
risk
95%
confidence
interval
Winship et al (1984)
FA
0.14
0.003-1.11
Mulinare et al (1988)
FA/MV
0.41
0.26-0.66
Milunsky et al (1989)
FA/MV supplement
0.29
0.15-0.55
diet: folate >100mg/day
0.42
0.16-1.15
Mills et al (1989)
MV/FA
0.87
0.80-1.10
Bower & Stanley (1992)
FA/MV
0.11
0.01-1.33
Werler et al (1993)
dietary FA
0.60
0.40-1.10
source: Adapted from:
Wald,35
CDC,38
Elwood,26
, NHMRC,
27
and respective studies
A variety of later studies have corroborated the finding that the periconceptual
use of folic acid reduces the recurrence and occurrence risk of NTDs. 28 29 30 31 32
33 During 1993-1995, the Centre for Disease Control and Prevention in the USA
and the People’s Republic of China conducted a population-based intervention
study of almost 250,000 women in the northern (high rates of NTD - 5-6/1,000)
and southern (low NTD rates - similar to US) area of China. The results showed a
85% reduction in the risk of a NTD among women in the north who took 400mcg
of folic acid daily at least 80% of the time periconceptionally, compared to 41% in
the south.34
The scientific evidence emphatically shows that folic acid supplementation in the
effective range of 360mcg - 4mg and increases in dietary folate prevents up to
70% of NTD 35 36 even though the mechanism of the action is still not completely
known.
Response by Agencies in the USA
In August 1991, the Centers for Disease Control and Prevention in Atlanta, USA,
recommended that women who had a previous NTD affected pregnancy and who
were planning to start a new pregnancy should consume a 4mg daily dose of folic
acid from at least one month before conception through the first trimester of
pregnancy.37
Folate, Folic Acid, and Health
5
On 11 September 1992, the US Public Health Service issued an enhanced
recommendation: 38
‘All women of childbearing age in the United States who are
capable of becoming pregnant should consume 0.4mg of folic
acid per day for the purpose of reducing their risk of having a
pregnancy affected with spina bifida or other NTDs. Because
the effects of high intakes are not well known but include
complicating the diagnosis of vitamin B12 deficiency, care should
be taken to keep total folate consumption at <1mg per day,
except under the supervision of a physician. Women who have
had a previous NTD-affected pregnancy are at high risk of
having a subsequent affected pregnancy. When these women
are planning to become pregnant, they should consult their
physicians for advice.’
In March 1996, the US Food and Drug Administration regulated that from 1
January 1998, enriched cereal grain products (e.g., flour, bread, pasta, rice etc)
would be fortified with 140mcg of folic acid per 100g flour.
The Response in Other Countries
Australia, Canada, China, Hungary, Ireland, New Zealand (see below), Norway,
South Africa, Spain, the Netherlands, and the United Kingdom are among the
countries which have also made recommendations to prevent NTDs by
increasing the consumption of folic acid or naturally occurring food folatesii (see
table 3). There are marked variations between the countries in the focus (e.g., all
women, women planning a pregnancy), level of daily consumption (e.g., 0.4mg,
0.8mg, greater than 0.5mg), and the methods advised to increase consumption
(e.g., daily supplement, folate-rich foods, a combination of both).39
Norway is one of the few countries with folic acid recommendations to advise
against fortification of foods with folic acid. Supplementation and diet are thought
to be sufficient to increase the folate levels of the population. The average intake
for adult women is ‘remarkably lower than the 400 micrograms per day
recommended’.40
‘Folic acid’ refers to pteroylmonoglutamic acid, a synthetic compound used in dietary
supplements and fortified foods and is more readily absorbed than most naturally occurring food
folates. ‘Folate’ refers to all compounds that have the vitamin properties of folic acid; folates
include folic acid and naturally occurring compounds in food
ii
Folate, Folic Acid, and Health
6
Table 3: NTD occurrence recommendations
Country
Directed at all fertile women or Recommended daily
at women planning a
consumption of folates
pregnancy
(mg)
How to achieve daily
consumption
Australia
planning or likely to become
pregnancy
>0.5
folate-rich foods + fortified
foods + 0.5mg supplement
daily
Canada
all
not specified
folate-rich foods
planning
>0.4/0.8iii
supplement daily
current status
China
planning
Chile
all
fortification of flour permitted
but not required - much of
Canadian flour is fortified
because millers export flour to
USA
>0.4
current status
supplement daily
fortification of flour used for
bread at 220mcg of folic acid
per 100g flour starting January
2000
Denmark
planning
0.4
folate-rich foods; supplement if
needed
Hungary
planning
0.4-1.0
supplement daily
current status
Ireland
some voluntary fortification of
bread
women who are likely to
become pregnant
>0.4
iii
folate-rich foods + fortified
foods + 0.4mg supplement
daily
The Canadian recommendations state that women planning a pregnancy should consult their
physician about folic acid supplements. In the information to physicians, it is stated that ‘a dose of
0.4mg daily is likely to be beneficial’, but ‘Individuals may choose to use doses up to 0.8mg, as
the evidence for a preventive effect on occurrence is strongest at that dose’.
Folate, Folic Acid, and Health
7
New Zealand
planning
0.8
current status
0.8mg tablet per day. A diet
containing extra folates around
the time of conception is
recommended to add to but
replace daily folic acid by tablet
some voluntary fortification of
46 foods (including breads,
breakfast cereals, food drinks)
- see table 4
Norway
all
0.4
folate-rich foods
South Africa
all
0.4
supplement daily
The Netherlands
planning
>0.5
0.5mg supplement daily
United Kingdom
planning
>0.4
folate-rich foods + fortified food
+ 0.4mg supplement daily
current status
United States
voluntary fortification of some
cereal grain products
all
0.4
current status
All enriched cereal grain
products (eg, flour, bread,
pasta, rice etc) have been
fortified with 140mcg of folic
acid per 100g flour
source: Cornel and Erickson 1997,39 Erickson 41
Folate, Folic Acid, and Health
food and/or fortified food and/or
supplements
8
Other Health Outcomes Affected by Folic Acid
Birth defects
There is overwhelming scientific evidence that periconceptional folate/folic acid
intakes of at least 0.4mg prevents up to 70% of NTDs. Research also indicates
periconceptional supplementation by folic acid or a multivitamin preparation
containing folic acid, may also reduce the risk of NTD cases that have associated
major defects (‘multiples’),42 as well as a number of other specific birth defects
such as orofacial clefts,43 44 congenital heart defects,45 46 47 limb defects,48 49 and
urinary tract anomalies.46 49 50 In a population-based study, Li et al 51 showed that
a periconceptional folic acid supplementation of 0.4mg/day can reduce the risk of
congenital heart defect occurrence by about 36%. It estimated that 28% (36,000)
of all cases of congenital heart defects (CHDs) in China could be prevented if
80% of women took 0.4mg of folic acid before their last menstrual period. A
recent initial study by James et al,52 reported that folate metabolism was
abnormal in mothers of children with Down syndrome.
On the contrary, studies 25 49 53 54 have reported the absence of a protective
relationship between the use of folic acid supplements and the risk of oral clefts
and limb defects.
Shaw et al 43 have cautioned that with multivitamin preparations the association
may not be attributable to folic acid specifically, but may be a consequence of
other multivitamin supplement components, or behaviours, that are highly
correlated with the use of multivitamins containing folic acid.
It is important to acknowledge that folic acid will prevent ‘folic acid-preventable
NTDs’55 by up to 70%, but will not completely eliminate the risk of NTDs
occurring. A considerably smaller number of babies will continue to be born with
NTDs because both genetic and environmental factors are important contributors
to the aetiology of the defects. For example, Werler et al 56 and Shaw et al 57
found that the risk of NTD was increased among obese women, independent of
the effects of folate intake and folic acid supplementation.
Cancers
Daily folate supplementation may provide some protection against the
development of neoplasis in ulcerative colitis.58 Women in the Nurses’ Health
study had a 75% lower incidence of colon cancer after consuming multivitamins,
containing 0.4g of folic acid, over a 15-year period.59 Glynn et al 60 and Kato et al
61 also suggest a possible association between low folate intake and the
increased risk of colon cancer (but not rectal cancer) and Ferraroni et al only with
rectal cancer.62 Baron et al 63 found ‘modest’ support for the beneficial effects of
Folate, Folic Acid, and Health
9
folate on colorectal adenoma risk, while the World Cancer Research Fund 64
cautioned that the epidemiological evidence is insufficient to suggest that higher
intakes of folate may decrease the risk of colorectal cancer.
While no association has been found with folate intake and the overall risk of
breast cancer 65 66 or the risk of early-stage breast cancer 67 there is a suggestion
that the excess risk of breast cancer associated with alcohol consumption may
be reduced by adequate folate intake.65
Research in South Africa 68 has suggested that an additional 0.4mg of folic acid
per day could substantially reduce the incidence of oesophageal, cervical, colon,
and primary liver cancers. In contrast, other reviews have concluded that high
dietary folate intake ‘possibly has no relationship with the risk of cervical cancer’
64 69 and the ‘data are insufficient to make conclusions regarding the possible role
of folate in reducing the risk of cancer of the lung, esophagus, or stomach.’ 70
A Canadian study among the elderly, found that people with low folate levels are
more likely to be demented, institutionalised, depressed and have a history of
weight loss.71 Poor folate status has also been associated with impairment in
word and object recall,72 and age-related hearing loss in elderly women.73 Clarke
et al 74 found low blood levels of folate and vitamin B12 and elevated plasma total
homocysteine levels were associated with Alzheimers disease.
Cardiovascular disease
There is an increasing body of research showing folic acid deficiency is
associated with elevated levels of homocysteine, an independent risk factor for
cardiovascular disease. Such a relationship has potentially major implications for
New Zealand’s health status. Despite the death rate from cardiovascular disease
declining since the 1950s, cardiovascular disease still accounts for more than
30% of all deaths and is a major component of hospital admissions.
Boushey et al 75 estimated that 10% (30,000 men and 19,000 women) of
mortality from coronary artery disease in the USA could be prevented by
increasing, through fortification, the daily intake of folic acid by 350mcg/100g for
men and 280mcg/100g for women. A subsequent meta-analysis 76 of published
and unpublished randomised trials that had assessed the effects on blood
homocysteine concentrations of folic acid supplements, with or without the
addition of vitamins B12 or B6, found that dietary folic acid reduced blood
homocysteine concentrations by 25%. There were similar effects in the range of
0.5-5mg folic acid daily.
In a large prospective study of 80,082 women from Nurses’ Health Study with no
previous history of cardiovascular disease, it was found that the 20% who had
the highest consumption of folate (94% had consumed multivitamins) had less
Folate, Folic Acid, and Health
10
cardiovascular disease than the lowest 20%
(7% had consumed
77
78
multivitamins). Oakley
observed that inadequate blood folate, the major
cause of homocysteine blood concentrations above the low, normal baseline, is
unusual among those who do consume, but common among those who do not
consume, multivitamin supplements. Ninety percent of those consuming
multivitamins in the Framingham Heart Study original cohort had homocysteine
levels above the low, normal baseline associated with adequate blood folate. 79
A case-control study by Verhoef et al 80 found that folate was the most important
determinant of plasma homocysteine, even in subjects with apparently adequate
nutritional status of the vitamin.
A recent population-based case-control study by Kittner et al 81 found a strong,
statistically significant, inverse association between multivitamin (included 0.4mg
of folic acid) use and stroke among women aged 15-44 years. Participants who
developed coronary heart disease in a prospective study 82 had lower, but not
statistically significant, mean plasma concentrations of folate. A retrospective
cohort study in Canada 83 reported low serum levels were associated with an
increased risk of fatal congenital heart disease.
The Australian Diet & Heart Advisory Committee for the National Heart
Foundation concluded:
‘there is strong circumstantial evidence that patients with
homocysteinaemia and vascular disease will benefit from treatment
with folic acid, 0.5-1.0mg per day. Such treatment is safe and should
be considered pending the outcome of controlled trials.’84
The Nutrition Committee of the American Heart Association has offered similar
advice in a statement for healthcare professionals.85
Riddell et al 86 concluded from a recent NZ study that:
‘The most appropriate means of reducing tHcy [total homocysteine]
levels in individuals and population is by increasing total dietary
folate from the present average intake of around 200ug/day to about
600ug/day, by the use of either folate supplements or fortified
breakfast cereals.’
Despite these highly promising and accumulating results there remain a number
of skeptics. To Havranek 87 ‘lowering homocysteine levels, through increased
folate intake is a promising but unproven primary prevention strategy.’ Kuller and
Evans88 are more emphatically negative and dismissive of results from the
current research:
‘It would be pleasant to be able to put folic acid in a hamburger bun and
enjoy half a pound of a juicy high-fat hamburger without worrying about
Folate, Folic Acid, and Health
11
high LDL cholesterol, coronary atherosclerosis, and thrombosis. Carrots
were not the panacea. Some hope that putting folic acid in bread will be
the next great public health advance for cardiovascular disease.’
Other health outcomes
There is an increasing volume of literature on the protective effects of folic acid in
reducing the risk of a number of other health outcomes. Scholl et al 89 suggested
that in low income, urban women, use of prenatal multivitamin/mineral
supplements (which included 1mg of folic acid) may have the potential to
diminish infant morbidity and mortality through reducing the risks of preterm
delivery and low birthweight. Czeizel et al 90 found no similar association using a
multivitamin containing 0.8mg of folic acid, and Stefanidis et al 91 reported no
relationship between folate levels of maternal serum and gestational age at
delivery or birth weight.
Data from the Hungarian folic acid-NTD trial showed that the female menstrual
cycle became more regular during multivitamin supplementation (including folic
acid),92 but there was no increased in sexual activity. 93
In addition to the unequivocal evidence that folic acid prevents NTDs, there is
sufficient and accumulating scientific research to indicate that folic acid reduces
the risk of a number of other adverse health outcomes.
Folate, Folic Acid, and Health
12
Epidemiology of Neural Tube Defects in NZ
In the 1995-96 period iv, the NZ Birth Defects Monitoring Programme (NZBDMS)
reported there were
31 cases of anencephaly (26 stillborn, 5 liveborn), a rate of 0.27 per 1,000
total births
59 cases of spina bifida (43 liveborn, 16 stillborn), a rate of 0.51 per 1,000
total births
90 NTD cases (48 liveborn, 42 stillborn), a rate of 0.78 per 1,000 total births
In 1997-98 there were: iv
7 liveborn cases of anencephaly
33 liveborn cases of spina bifida
The NZ rates of anencephaly and spina bifida are almost twice as high as the
rates reported from the Australian national programme and considerably higher
than the rates in England/Wales and Finland (table 4). However, with the
exception of the Japanese and Canadian programmes, terminations of
pregnancy (TOP) account for a considerable proportion of NTD cases. For
example, 83% and 68% respectively of all anencephaly and spina bifida cases in
England/Wales are notified from TOP.
Table 4: Rates of NTDs in selected birth defect monitoring programmes
Anencephaly
Spina Bifida
Total
Total births
Monitoring Programme
no
rate*
no
rate*
no
rate*
Australia ('96)
40
0.16
75
0.29
115
0.45
254,978
Canada (''96)
33
0.12
156
0.55
189
0.67
283,356
England/Wales ('97)
28
0.04
48
0.07
76
0.12
645,146
Finland ('97)
5
0.08
24
0.40
29
0.49
59,565
Japan ('97)
20
0.20
35
0.35
55
0.54
100,930
New Zealand ('95-'96)
31
0.27
59
0.51
90
0.78
115,854
Norway ('96)
7
0.12
16
0.27
23
0.38
60,085
USA:Atlanta ('97)
4
0.09
13
0.30
17
0.39
43,271
iv
1996 is the latest fetal death data available. The definition of a fetal death changed in late 1995
from 28 or more completed weeks of gestation to 20 weeks and/or 400g birthweight
Folate, Folic Acid, and Health
13
shtriblatoT latoT adifBanipS ylahpecn A
*etar on *etar on *etar on em argoPgnirotnM
879,452 54.0 51 92.0 57 61.0 04 )69'(ailrtsuA
653,82 76.0 981 5.0 651 21.0 3 )69'(adnC
641,56 21.0 67 70. 84 40. 82 )79'(selaW/dnalgE
56,95 94.0 92 04. 42 80. 5 )79'(dnaliF
039,01 45.0 5 53.0 53 02. 02 )79'(napJ
458,1 97.0 19 15.0 95 82.0 23 )69'-5 (dnaleZweN
580,6 83.0 32 72.0 61 21.0 7 )69'(yawroN
172,34 93.0 71 03. 31 90. 4 )79'(atnlA: SU
*rate per 1000 total births
source: NZ Birth Defects Monitoring Programme, ICBDMS Annual Report 1999
94
There is currently no facility to collect data on the numbers of terminations of
pregnancy carried out for NTDs. If TOPs constituted the same proportion of all
cases in NZ as in Australia and Finland, the annual number of NTDs would be
approximately:
47 cases of anencephaly (3 livebirths, 12 stillbirths, 32 TOPs)
53 cases of spina bifida (8 stillbirths, 20 livebirths, 25 TOPs)
100 cases of NTDs of which 20 are stillborn, 23 liveborn, and 57 TOPs
Data from the NZ Birth Defects Register, shows that the prevalence at birth rate
of NTDs: 4 95
is lower for Maori than nonMaori parents
is higher for females than males
is higher in the North than South Island for anencephaly, but not for spina
bifida
Folate, Folic Acid, and Health
14
is lower among births to women born in countries other than the British Isles
and NZ
is not related to maternal or paternal age, parity, urban-rural place of
residence, nuptiality, social class or season of birth
has been declining since the mid-1970s 96
is lower for NZ-born mothers than for mothers born in England/Scotland 97
Burden of NTDs in NZ
NTDs are the second major category of birth defects (after congenital heart
defects) and are a major component of fetal and infant death and morbidity. An
alternative method of understanding the population impact of spina bifida is
through the contribution to the overall ‘burden of disease’. This takes account of
both the years of life lost to premature mortality and the years of life lost
(severity-adjusted) to disability. Among 0-14 year olds, 35.5% of the total burden
from birth defects is due to congenital heart defects and spina bifida (table 5).
Current scientific evidence shows that the disease burden from these birth
defects can be reduced by increasing the daily intake of folic acid.
Table 5: Burden of disease - birth defects, 0-14 years, 1996
Birth defect
% of total
burden from
birth defects
Nonchromosomal defects
Congenital heart defects
Spina bifida
Down syndrome
Urogenital defects
Defects of the digestive system
Facial clefts
Defects of the abdominal wall
Other defects
Total
Folate, Folic Acid, and Health
41.0
20.5
15.0
10.2
3.0
1.8
0.4
0.7
7.4
100.0
15
source: NZ Burden of Disease Study 2
Cost of NTDs
Singh and Elliott 98 estimated that the 20-year cost of treating, managing and
caring for one spina bifida case in NZ is about $355,060. On average there are
about 20 liveborn cases of spina bifida per year resulting in a total cost over 20
years of $7,101,200. This does not include other potential costs such as the loss
of parental income, special schooling needs, family stress, wheelchair, crutches,
occupational therapy, GP visits etc.
Waitzman et al 99 100 employed a cost-of-illness methodology to estimate the
direct (includes medical, special education, and development services) and
indirect (includes mortality and morbidity) costs of spina bifida and 17 other birth
defects in the USA (table 6a). While health system costs in the USA are high by
international standards, these data, adjusted to NZD equivalents (table 6b), show
that spina bifida has the fourth highest lifetime cost from birth defects.
Folate, Folic Acid, and Health
16
Table 6a: Lifetime cost of selected birth defects, USA, discounted at 5% (US$1,000s,
1992)
Direct Costs
Birth defect
Spina bifida
Transposition/DORV
Tetralogy of fallot
Cleft lip or palate
Colorectal atresia
Renal agenesis
Lower limb reduction
Diagraphmatic hernia
Down syndrome
Cerebral palsy
Medical
204,512
166,334
185,122
97,126
57,213
24,713
16,560
62,772
278,696
851,809
Special
education
41,672
4,402
3,974
17,551
11,851
293,960
226,718
Developmental
services Indirect costs
1,781
241,324
343,794
171,390
2,937
578,888
162,049
399,466
138,656
301,576
95,029
1,180,068
217,899
1,129,355
Total costs
489,289
514,530
360,486
696,502
219,262
424,179
167,067
364,348
1,847,753
2,425,781
* double-outlet right ventricle
source: Waitzman et al 99
Table 6b: NZD equivalents* of lifetime cost of selected birth defects, NZD1,000s
New Zealand equivalent (1NZD=0.52USD)
Direct Costs
Special Developmental
Birth defect
Medical education
services Indirect costs
Spina bifida
393,292
80,138
3,425
464,085
Transposition/DORV
319,873
8,465
661,142
Tetralogy of fallot
356,004
7,642
329,596
Cleft lip or palate
186,781
33,752
5,648
1,113,246
Colorectal atresia
110,025
311,633
Renal agenesis
47,525
768,204
Lower limb reduction
31,846
22,790
266,646
Diagraphmatic hernia
120,715
579,954
Down syndrome
535,954
565,308
182,748
2,269,362
Cerebral palsy
1,638,094
435,996
419,037
2,171,837
* 1NZD = 0.52USD ** double-outlet right ventricle
source: Waitzman et al 99
Folate, Folic Acid, and Health
17
Total costs
940,940
989,481
693,242
1,339,427
421,658
815,729
321,283
700,669
3,553,371
4,664,963
Based on the data from Waitzman et al 99 the lifetime cost of each case of spina
bifida is estimated to be NZD565,000 (table 7), more than for the major
congenital heart defects such as tetralogy of fallot and transposition of the great
vessels, abdominal wall defects, and cleft lip or palate.
Table 7: Lifetime cost per case of birth defects, United States (1992) and NZD equivalent
Cost per case ($,000s)
Birth defect
USD (1992)
NZD*
Truncus arteriosus
505
971
Cerebral palsy
503
967
Down syndrome
451
867
Single ventricle
344
662
Spina bifida
294
565
Transposition/DORV**
267
513
Tetralogy of fallot
262
504
Renal agenesis
250
481
Diagraphmatic hernia
250
481
Lower limb reduction
199
383
Omphalocele
176
338
Tracheoesophageal fistula
145
279
Colorectal atresia
123
237
Gastroschisis
108
208
Cleft lip or palate
101
194
Upper limb reduction
99
190
Urinary obstruction
84
162
Atresia, small intestine
75
144
* 1NZD = 0.52USD ** double-outlet right ventricle
source: Waitzman et al 99
Folate, Folic Acid, and Health
18
The NZ Response to Folic Acid Research
On page 2 of the 10 January 1993 issue of the NZ ‘Sunday Times’
under the heading ‘Green vegie diet to avoid birth defects’ noted:
101
an article
‘pregnant women are being advised to eat plenty of green, leafy vegetables to
reduce the risk of their baby being born handicapped’.
‘The Health Department plans to send a circular to general practitioners
advising them to encourage pregnant patients to boost their intake of folic
acid’
the Department’s principal medical officer of health said that ‘the abundance
of vegetables in New Zealand meant there was no need to recommend "pills
and potions" to pregnant women. Instead they should simply ensure they ate
plenty of green vegetables, lightly steamed rather than cooked, and salads.’
The results of the UK MRC trial 24 were promoted by Dixon and Murray, 102 in the
10 March 1993 issue of NZ Medical Journal and by Elwood 103 in the 28 July
issue of the NZ Herald. In September, the Public Health Commission (PHC) v
produced a letter to health professionals entitled ‘Reducing the chances of spina
bifida by taking folic acid.’104 A public statement was made recommending that
all women planning a pregnancy should take a daily supplement of folic acid per
day. Only 5mg tablets were available on the NZ market. Women were also
advised to improve their diet by increasing the consumption of green vegetables.
Additional features of ‘the overall prevention plan for spina bifida and neural tube
defects’ were for the PHC and the Ministry of Health to:
obtain approval of a lower dose folic acid tablet
investigate whether and to what extent the food supply should be fortified with
folic acid
In June 1995, health professionals 105 and the public 106 107 were informed of the
availability of a ‘low dose’ 0.8mg folic acid tablet ‘to help prevent spina bifida in
planned pregnancies’. Women were advised that ‘diet alone does not provide
sufficient folic acid’ and ‘to take daily folic acid by tablet’. The PHC undertook to
investigate ‘other avenues for increasing folic acid intake’ noting the ‘Addition of
folate to manufactured foods deserves serious consideration as this could
contribute to a reduction in the incidence of spina bifida and other conditions.’ 108
v
The Public Health Commission was disestablished in 1994 and its functions taken over by the
Ministry of Health (policy and monitoring) and the Regional Health Authorities (purchasing)
Folate, Folic Acid, and Health
19
In 1995, the PHC recommended that ‘spina bifida incidence among livebirths be
reduced one-third below the 1993 incidence level by 1997.’ 108 The target was
elaborated in the 1995 edition of ‘Progress on Health Outcome Targets’: 109
‘To reduce by 30 percent the prevalence of spina bifida among
livebirths from 0.42 per 1,000 livebirths in 1993 to 0.29 per 1,000
livebirths by the year 1997.’
Two important points were made in the accompanying commentary:
‘At the current rate of decline [of spina bifida] the target will be easily
achieved’
‘Fortification of food with folic acid will be considered by the Ministry of Health
in 1995 as a way to reduce the risk of spina bifida in unplanned pregnancies’
The ‘National Plan of Action for Nutrition’, published in 1995, observed: ‘Most
nutrition professionals in New Zealand have supported the view that all New
Zealanders can obtain the nutrients they need through the appropriate food
choices (apart from folic acid, iodine and fluoride).’ 110
Subsequent developments in NZ’s response to the scientific research on the
relationship between folic acid and NTDs have been:
1996
Singh and Elliott 98 recommend a ‘Folate Replenishment-Plus Programme’
to fortify all flour with folate
Kellogg launches its entire range of cereals with added folic acid onto the
New Zealand and Australian market with the ‘Folate added’ logo on the
packaging
1997
in January/February Sanitarium adds folic acid to the breakfast cereal
‘Weetbix’ at a level of 333mg/100g
the flourmilling industry through its research trust is approached to lend
support to the proposal to fortify all flour with folic acid
the Folate Replenishment-Plus Committee formed to coordinate and
promote the fortification of flour with folic acid. Membership comprises
health professionals, representatives of the milling and baking industry
and NZCCS, a nutritionist, an epidemiologist, and a public relations
Folate, Folic Acid, and Health
20
consultant. Funding was initially provided by the NZ Flourmillers’ Research
Trust and subsequently by NZCCS
1997-98
Folate Replenishment-Plus Committee undertakes a consultation and
communications campaign and begins discussions with the Ministry of
Health about the folate fortification of flour to the level of 285mcg/100g
1998
The Baking Industry Research Trust commission Bourn and Newton, from
the Department of Consumer Sciences, University of Otago to produce a
report on ‘Consumer Attitudes on the Fortification of New Zealand Bakery
Products’ 111
based on feedback from consultation, the Folate Replenishment-Plus
Committee modifies its proposal to only fortify bread, rather than flour, at
the level of 140mcg/100g and discussions begin with the NZ Association
of Bakers
The Australia New Zealand Food Authority (ANZFA) launches the folate
health claim and continues negotiations with the corporate and business
community
Sanitarium progressively adds folic acid to other products such as ‘Hi
Bran/Soya Linseed’, ‘Marmite’ and ‘Light & Tasty’
in November, Kellogg conducts research on folate awareness
1999
in March, Kellogg launches a campaign about the benefits of folate to
health generally and specifically in reducing the risk of NTDs
the Ministry of Health and ANZFA fund University of Otago to collect
baseline data on folate intake and blood folate levels among women of
child-bearing age and teenage boys
in June, Watson and McDonald
Pregnancy’
in June, Kellogg repeats its previous research on folate awareness
in August, publication of results from the ‘1997 National Nutrition Survey’
122
113
Folate, Folic Acid, and Health
21
release a report on ‘Nutrition during
in September, Sanitarium announces at nutrition conference in Auckland
that four products in Australia and two in New Zealand will carry the
ANZFA folate health claim
late 1999 - Champion, New Zealand’s leading supplier of flour and bakery
pre-mixes, adds folic acid to all its improvers, concentrates and yeastraised bakery mixes at the recommended levels. To coincide with this
initiative, a leading supermarket retailing group applies for registration
from ANZFA to add folic acid to all bread made at its in-store bakeries
using Champion’s bakery mixes and concentrates with added folic acid.
Folate Intake of New Zealanders
The current NZ Recommended Daily Intake (RDI) of folate is 200mcg per day for
non-pregnant adults and 400mcg per day for women of childbearing age 112. As
previously noted the Ministry of Health also recommends that women planning a
pregnancy should take an additional daily supplement of folic acid to reduce the
risk of NTDs.
The 1997 the National Nutrition Survey 113 found that the usual daily median
intake of folate from food was 242mcg (males 278mcg, females 212mcg) (table
8). In comparison, the median intake in the 1991 survey 114 was less than
170mcg, but the increase could represent a change in folate intake as well as
differences in the methods used in the two surveys.
In 1997, median folate intakes for males ranged from 256mcg (65+ year age
group) to 286mcg (25-44 year age group) and for females from 194mcg (15-18
year age group) to 222mcg (45-64 year age group). Males and females living in
NZDep96 115 quartile IV areas had lower levels of intake (268mcg and 201mcg
respectively) than those living in the highest quartile I areas (287mcg and
227mcg respectively).
Comparing results from the 1991 and 1997 surveys shows the median intake for
boys aged 15-18 years increased 27%, compared to more than 45% in the other
age groups. Among women, the median intakes in the 15-18 and 19-24 year age
groups increased 28% and 14% respectively, compared to 43% for 25-44 years,
and more than 51% in the oldest age groups.
Folate, Folic Acid, and Health
22
Table 8: Usual folate intake by ethnic, gender, age group
Usual folate intake
(mcg)
50th
percentile
Ethnic group / Age group
1991
gender
(yrs)
NZ
Male
Female
Maori
Male
Female
Other
Male
Female
1997
1997 inadequate
intake (%) *
242
277
272
286
278
256
278
194
195
213
222
217
212
7.1
2.8
3.4
1.6
0.8
1.0
1.3
22.2
21.2
13.4
9.8
9.2
13.1
15-24
25-44
45+
Total
15-24
25-44
45+
Total
226
283
260
273
194
207
196
198
8.7
2.5
1.0
2.3
28.6
18.4
26.0
23.0
15-24
25-44
45+
Total
15-24
25-44
45+
Total
291
290
272
282
197
215
222
215
1.7
0.8
1.5
1.7
18.7
11.5
9.5
11.5
15+
15-18
19-24
25-44
45-64
65+
Total
15-18
19-24
25-44
45-64
65+
Total
170
218
187
192
192
176
192
151
171
149
147
140
151
*calculated by probability analysis
source: 1997 National Nutrition Survey, 113 1991 National Nutrition Survey 114
Folate, Folic Acid, and Health
23
In 1997, the prevalence of inadequate intake was reported to be higher among:
females than males (irrespective of age) (table 8)
NZ Maori females and males than NZ European and Others (table 8)
females living in areas the lowest quartile of NZDep96 compared to those
living in quartile I areas
females aged 15-24 years (21.2-22.2%) compared with females aged 45+
years (9.2-9.8%) (table 8)
However, the authors caution that ‘the prevalence of inadequate intake is likely to
be overestimated’ because of the difficulty in determining folate levels in foods
and that the requirements have been set to maintain liver stores. 113
Sources of folate
According to the 1997 National Nutrition Survey,113 vegetables are the principal
source of dietary folate in most age groups (table 9). The exceptions are
breakfast cereals (16%) for males aged 15-24 years, while vegetables and bread
contribute similar proportions (15%) of dietary folate for females aged 15-18
years.
Folate, Folic Acid, and Health
24
Table 9: Major sources of dietary folate, by gender and age group
Age
group
(yrs)
NZ
population
Male
Major sources of folate (%)
Vegetables
Bread* Breakfast
cereals
Fruits
Potatoes
and kumara
15+
18
13
11
8
8
15-18
19-24
25-44
45-64
65-74
75+
Total
13
12
18
18
24
18
17
12
11
14
14
12
14
13
16
16
10
10
12
14
12
5
6
6
6
6
8
6
11
10
8
8
8
9
9
15-18
15
19-24
20
25-44
18
45-64
22
65-74
22
75+
22
Total
20
* includes rolls and speciality breads
15
12
13
13
13
12
13
10
9
11
10
10
13
10
9
11
9
10
11
10
10
8
8
7
6
6
6
6
Female
source: 1997 National Nutrition Survey 113
Methods of Enhancing Folate Levels in The Population
Three strategies are available to increase the folate levels sufficiently to prevent
NTDs: diet, supplementation, and fortification. The first two approaches are
selective by focusing primarily on women who are planning a pregnancy, while
fortification is a population based strategy.
Diet
A NZ study 122 of the diet of pregnant women at four and seven months found
less than half of the women had changed their eating habits since they became
pregnant. Maori and Pacific Island women ate less fruit and vegetables, the
major source of dietary folate, and bread and cereals than European women.
Women in the lower occupational categories ate bread and cereals less often
Folate, Folic Acid, and Health
25
than the other groups. However, the report provides no indication of the
relevance of these data to the mothers’ diet at the time when NTDs are formed.
It is not feasible to expect a woman to increase her folate level through diet
alone. As highlighted by Skeaff and Mann,116 the folate-NTD relationship is:
‘the first well documented public health situation where the amount of
nutrient required to prevent the nutrient-related condition is more than
can be practically eaten in the diet by choosing foods wisely.’
Wald and Bower 117 noted that for a woman to receive an extra 0.4mg of folic
acid each day she would have to ‘consume over eight glasses of orange juice, 10
servings of broccoli, three servings of brussel sprouts, or appropriate
combinations of such foods.’
Elwood 118 estimated that 100g of fresh green cabbage, a good source of folate,
contains only about 90mcg of active folic acid.
The bioavailability of food folate is about 50%. 70 Therefore, Cuskelly et al 119
found that dietary advice and consumption of extra folate as natural food folates
were ‘ineffective in optimising folate status.’ In contrast, serum folate doubled
with supplements and fortified foods. The authors concluded: ‘that advice to
women to consume folate-rich foods as a means to optimise folate status is
misleading.’
Improving all aspects of maternal diet, especially among adolescent mothers,120
should be regarded as a fundamental part of public health practice. While it is
commendable to encourage women to consume more folate-rich foods, such a
strategy alone will have little impact on preventing NTDs.
Supplementation
The second strategy for the prevention of NTDs is through the use of dietary
supplements,vi either specifically folic acid or a multivitamin containing folic acid.
The bioavailability of synthetic folic acid ranges from about 100% for
supplements taken on an empty stomach to 85% when consumed with a meal. 70
An economic analysis in the USA,121 estimated that folic acid supplementation
would reduce annual hospital charges for NTDs and congenital heart defects
respectively by USD73-89m and USD1047-1135m.
A dietary supplement is ‘an edible substance in a controlled dose which is intended to
supplement the intake of those substances normally derived from food’ (Nutrition Taskforce. Food
for Health. The Report of the Nutrition Taskforce to the Department of Health. Wellington:
Department of Health, 1991)
vi
Folate, Folic Acid, and Health
26
use of supplements
The 1997 National Nutrition Survey 113 found that 51% of the NZ population (59%
of females, 42% of males) were regular or occasional users of vitamin and/or
mineral supplements during the last year (table 9). Only 23% of Pacific Island
women used these supplements, compared to 46% of Maori women and 63% of
‘Other’ women (table 10) Three percent of the women aged 25-44 years in the
‘Other’ ethnic group consumed folic acid supplements in the last year.
Table 9: Vitamin and mineral supplement use in the last year, by gender and age
group
Gender
NZ
Male
Female
Consumption frequency % of population consuming
Age group Regular* Occasional** Multivitamins
Folic acid
(yrs)
&/or mineral
15+
28
23
19
1
15-18
19
36
17
0
19-24
18
33
15
0
25-44
21
26
16
0
45-64
22
13
10
0
65-74
21
4
8
0
75+
19
5
13
0
Total
21
21
14
0
15-18
29
37
16
0
19-24
33
36
32
0
25-44
37
27
27
2
45-64
36
20
24
0
65-74
35
15
16
1
75+
26
8
11
0
Total
34
25
24
1
* used any supplement at least once per week, during the last year
** used any supplement no more than three times per month, during the last year
*** the use of any supplement, regular or ocassional
source: source: 1997 National Nutrition Survey 113
Folate, Folic Acid, and Health
27
Table 10: Vitamin and mineral supplement use in the last year, by ethnic group, females
Ethnic group Age
group
(yrs)
Maori
15-24
25-44
45+
Total
Pacific Island 15-24
25-44
45+
Total
Other
15-24
25-44
45+
Total
Consumption
%
of
population
frequency
consuming
Regular* Occasional** Multivitamins Folic acid
&/or mineral
22
29
22
25
10*
11
12*
11
35
39
35
37
20
25
14
21
12*
14
8*
12
43
29
17
26
9
20
18
16
6+
9
11+
9
31
29
20
26
0
1
0
0
0+
0
0+
0
0
3
0
1
* used any supplement at least once per week, during the last year
**used any supplement no more than three times per month, during the last year
*** the use of any supplement, regular or occasional
+ limited sample size
source: source: 1997 National Nutrition Survey 113
There are caveats with these data. ‘Regular’ and ‘occasional’ users take a
supplement ‘at least once a week’ and ‘three times per month’ respectively, but
folic acid must be taken daily to prevent NTDs. There is no indication of the
amount of folic acid included in either the multivitamin or folic acid specific
supplements.
Watson and McDonald 122 found that 37% of 504 pregnant female volunteers in
the northern half of the North Island had taken folic acid supplement in the year
before their pregnancy (table 11). Almost half of ‘European’ women used a
supplement compared to 10% of Maori and 9% of Pacific Island women. Among
European and Pacific Island women consumption of multivitamin supplements
were considerably lower than the consumption of folic acid supplements. The
authors noted: ‘there was some anecdotal evidence Pacific Island women were
being warned off all pills during pregnancy, which includes folic acid.’
The use of folic acid also increased with higher occupation category and
increasing education level and income. It is not clear from the study report what
effect recall bias may have on the results, and the relevance of diet and nutrition
data at months 4 and 7 of pregnancy compared to the time of conception and the
first 28 days of gestation (when NTDs occur). There is also no indication about
Folate, Folic Acid, and Health
28
the frequency of supplement use in the year before the pregnancy or the amount
of folic acid in the various supplements.
Table 11: Women taking multivitamin and folic acid supplements in the year before pregnancy
Ethnic group
European
Maori
Pacific
Total
Supplement use in the year
pregnancy
Multivitamin
Folic acid
no
%
no
43
12.1
173
10
10.0
10
1
2.6
4
54
10.8
187
source: adapted from Watson and McDonald
before
%
48.6
10.0
8.7
37.1
122
A nationwide mail survey in 1998 111 found 69% of females and 49% of males
had taken some form of dietary supplement (there was no indication of type of
supplement) during the previous year. The highest proportions of weekly
supplement takers were in the youngest age groups. The proportion of older
respondents taking supplements at least once a week was less than in the
younger age groups.
Despite the methodological limitations of these NZ studies, there are indications
that NZ women are not taking sufficient folic acid by supplementation to prevent
NTDs.
sales and availability of folic acid tablets
In the period 1991 to 1996, annual unit sales of folic acid in NZ, 123 which will be
an underestimate of the true level of supplementation, declined by 24% from
172,300 to 130,013 (figure 1). The peaks of sales each year generally occurred
in March-April and there is some evidence that the major announcements on folic
acid stimulated a small sales reaction.
Annual sales increased 4% in 1997, and 7% in 1998, with peak sales occurring in
November-December. There is some evidence of more consistent purchasing of
folic acid tablets since July 1995, when the second recommendation was issued
by the Ministry of Health and the so-called ‘low dose’ 0.8mg folic acid tablet
became available.
Folic acid is available on the NZ market from folic acid specific tablets of 300mcg,
800mcg, and 5mg, and multivitamin tablets with levels of folic acid ranging from
30mcg to 350mcg (table 12). Most multivitamin tablets will not provide sufficient
daily folic acid to prevent NTDs. In contrast, multivitamin tablets in the USA
usually include 400mcg of folic acid. The annual cost of folic acid specific
supplements in NZ is about NZD30-40.
Folate, Folic Acid, and Health
29
Table 12: Sample of folic acid supplements available in NZ, November 1999
Manufacturer
Brand
Healtheries
Healtheries
Healtheries
Healtheries
Healtheries
Healtheries
Multivitamin & minerals
Teenage multi
Senior multi
Womens multi
Womens multi
Folic acid
MV
MV
MV
MV
MV
FA
nil
130mcg
100mcg
300mcg
300mcg
300mcg
30
60
60
10.30
17.05
5.35
Red Seal
Red Seal
Red Seal
Womens multi
One-a-day multi
Total multi
MV
MV
MV
300mcg
100mcg
30mcg
30
30
30
9.25
5.25
7.75
Kordels
Kordels
Kordels
Womens multi
Megatime
Teentime
MV
MV
MV
300mcg
300mcg
125mcg
30
60
60
12.95
21.95
16.95
Natural nutrition
Natural nutrition
Womens mega vita-min
Nutritent care for women
on the pill
MV
MV
200mcg
200mcg
50
30
22.95
14.95
Folate, Folic Acid, and Health
Multivitamin
(MV) or folic
acid (FA)
Amount of Number
folic acid
of
tablets
30
Cost
Comment or any health
statement on accompanying
packing
"Recommended prior to and
during pregnancy for health
cell development"
Nature's Own
Folic acid
FA
300mcg
100
Blackmores
Folic acid
FA
300mcg
90
Blackmores
Womens multi
MV
300mcg
50
9.95 "May reduce the risk of having
a child withg spina
bifida/neural tube dfefects if
taken prior to and during
pregnancy"
17.95
Thompsons
Thompsons
Thompsons
Folic acid
Femmefit
Multifort
FA
MV
MV
300mcg
300mcg
300mcg
80
60
60
9.95
19.95
18.80
Abbott
Bio-organics
Iron-folic acid
Ultra
Iron+FA
MV
350mcg
25mcg
30
30
5.95
17.80
Folic Acid
obtained from
pharmachist
Folic acid
FA
800mcg
120
9.95
no questions were asked or
advice given
Folic Acid
obtained from
pharmachist
Folic acid
FA
5mg
120
8.50
no questions were asked or
advice given
Folate, Folic Acid, and Health
31
8.75
"Useful for normal health
pregnancies"
Figure 1: Unit sales of folic acid in New Zealand, 1991 to June 1999
unit sales
45000
40000
35000
MRC study
published
30000
0.8mg tablet
advertised
1st PHC
recommendation
25000
20000
15000
10000
5000
0
J
1991
J= January
J
1992
J
1993
J
1994
J
months and years
source: IMS HEALTH, New Zealand Phamaceutical Index, June 1999
Folate, Folic Acid, and Health
1995
33
J
1996
J
1997
J
1998
J
1999
Knowledge about folate and NTDs
Integral to increasing the intake of dietary folate and the use of supplements is
the level of knowledge that health professionals and the public have about the
benefits of improving folate levels.
A number of studies have investigated the awareness of folic acid among
populations, changes in diet or supplement use, the impact of mass media
campaigns and the usefulness of other information sources.
For example:
in Toronto in 1994 124 only 13% of mothers of spina bifida infants were aware
of relation between folic acid and NTDs and they did not take folic acid
supplements. A sample of ‘well educated, English speaking women’, in
Ontario during 1997-98 showed 63% were aware of the need for
preconceptional folic acid, but only one third took vitamin supplements before
conception 125
in Ireland, traditionally an area with high international rates of NTDs, only 16%
of women were taking folic acid despite a mass media campaign. 126
Marriage and planned pregnancy were predictors of folic acid knowledge,
compared to planned pregnancy advice given before pregnancy and relative
affluence as predictors of periconceptional use127
specifically in Dublin, 63% of women were aware of folic acid, but this
knowledge was associated with higher social class and education and only
3% of women were actually taking supplements 128
41% of female undergraduate students were aware of the need to increase
folate intake 129
a South American study 130 found that 40% of women claimed to have taken
vitamins during pregnancy, but only half were actually found to have taken
vitamins. Minerals and other products had often been mistaken for vitamins.
None of the mothers who took vitamins did so preconceptionally, 14% knew
the benefits of taking folate, but only 2% correctly identified folate rich foods
in Glasgow, 57% of women took supplements during their pregnancy, but only
21% did so before conception. 131 The most important reason for not taking
supplements was the lack of awareness of the benefits, with unplanned
pregnancy, younger age, and previous pregnancies being other reasons
in Israel, 6% of 920 women interviewed had heard of folic acid and 38% had
taken it132
Folate, Folic Acid, and Health
35
in a study in Atlanta, 133 the location of the Center for Disease Control and
Prevention, found than 80% of low income, predominantly minority women did
not take supplements preconceptionally, 57% had heard about folate, and
30% could list folate rich food sources.
among Latinos and African Americans in inner city Hartford, 11% of
respondents identified folic acid as capable of preventing NTDs, and more
than 80% did not know which foods were folate rich, and the intake of fruit
and vegetables was low 134
in Western Australia, most women were not taking folic acid supplements
before they became pregnant (the critical time), but there was an increase in
the number taking supplements in the first trimester 135
Brandenburg et al 136 found that 60% of women were taking folic acid
supplements, but only 25% were using it periconceptionally
in the south of England, 32% of pregnant women used supplements
containing folic acid before conception, but young age, smoking and low
education attainment were predictors of failure to use folic acid before
conception.168 Previous reports 137 138 139 140 from elsewhere in England also
found that women had poor knowledge of folic acid and a low level of
supplementation
pregnant women attending an inner city practice were no more aware of the
relationship between folic acid and NTDs than non-pregnant women in
contrast to women attending a suburban practice 141
surveys before the 1996 Victorian Folate Campaign in Australia found that
78% of women knew the term ‘folate’ or ‘folic acid’, 42% did not know what it
was, 12% knew folate prevents NTDs, 40% knew folate should be taken
periconceptionally, and 4% were taking a folate supplement 142
a 1998 national sample survey of women 143 in the US reported:
-
68% had heard or read about folic acid (52% in 1995)
awareness was lowest among 18-24 year olds and those with less
than high school education
13% knew that folic acid prevents birth defects
7% knew that folic acid should be taken before pregnancy
32% were taking a daily vitamin supplement containing folic acid
only about 2% of women in a sample from teaching practices in Northeastern
Ontario knew that folic acid supplementation before conception prevents
NTDs 144
Folate, Folic Acid, and Health
36
Results from studies reporting on the sources of information about folic acid and
NTDs show:
in Ontario, the media were the principal source of information before
conception and doctors after 125
in Glasgow, the major sources of information on folic acid supplement use for
pregnant women were GPs, magazines, and books 131
a random sample of Canadian physicians
correct timing of folic acid supplements
less affluent women in Ireland used their GP more as a source of information
and advice than more affluent women 127
in Dublin, the majority of women found out about folic acid from lay sources
(eg, friends and media) 146
doctors were the major source of information in Western Australia
a small survey in England in 1995 139 found that only 43% of GPs correctly
knew the correct dose and duration of folic acid needed to prevent NTDs
in 1998 in the USA,143 31% of women of childbearing age obtained
information about folic acid from books and magazines, 23% from radio or
television, and 19% from health care providers
in Southwestern Virginia, television and healthcare providers were the two
leading sources of information about folic acid 147
Bonin et al 144 found variability about knowledge of folic acid supplementation
between 22 teaching practices in Northeastern Ontario
among women attending two GP practices in the UK, magazines and
newspapers were the major source of information. 141 Only a third of patients
mentioned health professions as a source of information
in Leiden, 148 18% of GPs thought they were insufficiently informed about folic
acid recommendations, 58% sometimes forgot to inform the women about
folic acid, and 66% thought it contributed to the medicalisation of the
pregnancy
145
showed that only 14% knew the
150
Mass media campaigns are often used to increase public awareness and use of
folic acid. Evaluations of some of the campaigns show:
Folate, Folic Acid, and Health
37
following mass media campaigns in the Netherlands in 1995 149 and Ireland in
1996-97,126 the awareness of women about folic acid increased more than
76% and usage of folic acid more than doubled. However, in the Netherlands
the socioeconomic differences in awareness persisted.
in Western Australia: 150
-
-
-
the promotion of folic acid supplements to prevent NTDs during 199295, resulted in 70% of GPs offering folic acid supplements to women
planning a pregnancy, 56% of GPs and 82% of pharmacists knowing
the recommended dose of 0.5mg, and an 88% increase in sale of
0.5mg of folic acid
it was estimated that 68% of women of child-bearing age in Western
Australia knew of the association between folic acid and NTDs
compared with 8% before the campaign
women who had seen the promotional pamphlet were seven times
more likely than women who had not seen the pamphlet to know
increasing folic acid intake prevents NTDs
in southwestern Virginia there were considerable increases in the awareness
and knowledge of the benefits of folic acid following a year-long community
information campaign aimed at the women of childbearing age in 1997
Therefore, most women are still not aware that folic acid prevents NTDs, the use
of folic acid is still low, and women who do take supplements are usually not
taking them periconceptionally. Mass media campaigns can increase awareness,
but these need to be sustained over a period of time.
Fortification
The preceeding evidence from NZ and overseas clearly shows that improving the
folate status of a population to a level sufficient to prevent NTDs can only be
achieved through a population approach. The effective change in dietary habits
and use of supplements is dependent on a number of factors such as patient
education, availability and cost of foods, access to care, access to medication,
compliance and acceptability of taking supplements in pregnancy, availability and
accuracy of advice given to women. In many cases, these requirements are most
problematic for those in the lower or more disadvantaged socio-economic
groups.
It has been estimated 151 that in the UK, GPs would have to give advice during
35,714 consultations about contraception or 111,428 general medical
consultations to prevent one neural tube defect. The estimate assumes that
women plan their pregnancies, attend for consultations, remember and wish to
comply with the advice given, and can afford folate supplementation.
Folate, Folic Acid, and Health
38
Another major impediment to improving folic acid intake through supplementation
is the high proportion of pregnancies which are unplanned. A number of studies
have shown that women were consuming supplements after the critical time of
NTD formation. In many countries it is estimated that about 40% of pregnancies
are unplanned, in contrast to the Netherlands where 90% of pregnancies are
planned.149 There are no data on the proportion of unplanned pregnancies in NZ.
As a surrogate measure, rate of teenage pregnancy in NZ has declined over the
last ten years, but it is still of the highest in the developed world 152
Because diet and supplementation have major deficiencies as delivery
mechanisms, food fortification vii has been proposed as the population strategy
for improving folate status and preventing NTDs. Fortification is simple, does not
require behavioural change or active intervention, and is in the public domain.
Skeaff and Mann 116 identified ‘the key principal of fortification is that the amount
of nutrient added to the food supply should be only as much as is needed to
produce the desired effect while minimising any risk of toxicity to the target and
non-target populations.’
Cost effectiveness of folic acid fortification
A number of studies have shown that fortification with folic acid is a highly
effective delivery mechanism for increasing the folate status of a population. An
extensive economic analysis in the USA 100 153 concluded that fortification of
cereal grains ‘would probably have economic benefits that significantly exceed
the costs under a wide range of assumptions.’ It was estimated that US
consumers would spend USD132,000 on supplements to avert one NTD case,
compared to USD92,500 for low-level fortification (140mcg/100g) and
USD65,500 for high-level fortification (350mcg/100g).
Singh and Elliot 98 have estimated that preventing one spina bifida birth per year
in NZ will pay for the entire costs of fortifying 236,000 tonnes of flour milled
annually at 100mcg/35g ($201,780). Supplementation using folic acid tablets was
estimated to cost about $30 per year per women capable of childbearing.
Therefore, the total annual cost of fortification equates to the cost of 6,726
women taking folic supplements. In the 1996 Census there were 833,730 women
aged 15-44 years.
The NHMRC 27 in Australia estimated that each year fortification would produce
savings of AUD$2,315,289 and acknowledged this would be an underestimate.
Fortification is the addition of nutrients to food ‘for the purpose of improving the quality of food
or as a way of helping to improve the nutritional status of a population or a sector of the
population.’ source: Ministry of Health. Food and Nutrition Guidelines for Health Children Aged 212 Years: A Background Paper. Wellington: Ministry of Health, 1997
vii
Folate, Folic Acid, and Health
39
Fortification of foods in NZ
The introduction of a fortification programme requires the availability of a
legislative regulation and the provision for health claims to be placed on food
products.
In accordance with The Food Regulations 1984, Amendment no 12 (1995/305),
the allowable folate fortification level in NZ since January1996 is 100mcg per 35g
of white flour and pasta, and 50g of breads. In 1998, 46 viii foods available in NZ
had been fortified with folic acid, 50% of which were breakfast cereals, and 21
were produced by Kelloggs (Aust) Pty Ltd (table 13). The earliest date that a
product had been fortified was 1 January 1980 (Healtheries KLB6 Slimming
Formula - 320.00mcg/100g). Three of the four breads had been fortified
(200mcg/100g) since 1 March 1996.
Table 13: Total number of foods fortified with folic acid in NZ in 1998
Food
Breads
Breakfast cereals
Extracts of meat,
vegetables
Food drinks
Supplement bar
Total
yeast,
no
fortified
4
23
or 1
15
3
46
source: NZ Therapeutic Database
The overall level of fortification varies from 40mcg/100g (‘Up & Go’) to
2000mcg/100g (‘Marmite’), but in bread and breakfast cereals the range is from
166.70mcg/100g to 333.30mcg/100g (table 14).
viii
The summary in the publication from the NZ Therapeutic Database lists 48 foods available in 1998
which had been fortified; details are only given for 46 products - no details are given for the 2 fortified fruit
juices
Folate, Folic Acid, and Health
40
Table 14: Fortified foods available in NZ, 1998
Food
Company Brand
Product
Amount
Date
fortified
Fibre White
Swiss Grain
Wholemeal
200.00mcg/100g 1/03/1996
200.00mcg/100g 1/03/1996
200.00mcg/100g 1/03/1996
Mighty White
200.00mcg/100g 1/10/1998
Breads
Allied Foods Co Ltd
Norths Extra
Tip Top
Breakfast cereals
Kelloggs (Aust) Pty Ltd
Kelloggs
All-bran
222.20mcg/100g
All Bran Soy 'N' Fibre
222.20mcg/100g
Bran Flakes
333.00mcg/100g
Coco Pops
166.70mcg/100g
Corn Flakes
333.00mcg/100g
Crispix
167.00mcg/100g
Crunchy Nut Corn Flakes 166.70mcg/100g
Froot Loops
166.70mcg/100g
Frosties
166.70mcg/100g
Golden Wheats
333.00mcg/100g
Honey Rice Bubbles
167.00mcg/100g
Just Right
222.00mcg/100g
Just Right Grains
222.00mcg/100g
Mini-wheats - Apricot
333.30mcg/100g
Mini-wheats
- 333.30mcg/100g
Blackcurrent
Mini-wheats - Strawberry 333.30mcg/100g
Nutri-grain
166.70mcg/100g
Rice Bubbles
166.70mcg/100g
Special K
333.30mcg/100g
Sultana Bran
222.00mcg/100g
Sustain
222.00mcg/100g
Sanitarium The Health
Food Co
Sanitarium
Light 'N' Tasty
Weetbix
Folate, Folic Acid, and Health
41
1/12/1996
1/08/1998
1/01/1998
1/12/1996
1/12/1996
1/06/1997
1/12/1996
1/12/1996
1/12/1996
1/06/1997
1/06/1997
1/12/1996
1/10/1998
1/12/1996
1/12/1996
1/12/1996
1/12/1996
1/12/1996
1/12/1996
1/12/1996
1/12/1996
333.30mcg/100g 1/11/1997
100.00mcg/100g 1/03/1997
Extracts of meat, yeast, or
vegetables
Sanitarium The Health
Food Co
Sanitarium
Marmite
2000.00mcg/100 1/07/1998
g
Food
drinks
Healtheries of NZ Ltd
Healtheries
KLB6 Slimming Formula 320.00mcg/100g
- Creamy Vanilla
KLB6 Slimming Formula 320.00mcg/100g
- Luscious Strawberry
KLB6 Slimming Formula 320.00mcg/100g
Rich - Chocolate
Vitaplan - Bountiful Berry 55.00mcg/100g
Vitaplan
Classic 55.00mcg/100g
Chocolate
Vitaplan - Vital Vanilla
55.00mcg/100g
Heinz
Wattie's
Australasia
Complan
Complan Banana
55.00mcg/100g
Complan Chocolate
55.00mcg/100g
Complan
Double 55.00mcg/100g
Chocolate
Complan Strawberry
55.00mcg/100g
Complan Vanilla
55.00mcg/100g
1/01/1980
1/01/1980
1/01/1980
1/02/1995
1/02/1995
1/02/1995
14/02/1996
14/02/1996
14/02/1996
14/02/1996
14/02/1996
Sanitarium The Health
Food Co
Sanitarium
Up & Go - Banana
Up & Go - Cocoa Malt
Up & Go - Original Malt
40.00mcg/100g 1/10/1998
40.00mcg/100g 1/10/1998
40.00mcg/100g 1/10/1998
Smithkline Beecham Consumer Healthcare
Horlicks
Malted Food Drink
160.00mcg/100g 1/12/1996
Supplement bar
Folate, Folic Acid, and Health
42
New Image International
K-28Plus
K-28Plus Blueberry
K-28Plus Chocolate
K-28Plus Vanilla
167.00mcg/100g 1/01/1998
167.00mcg/100g 1/01/1998
167.00mcg/100g 1/01/1998
source: NZ Therapeutic Database
Health claims
Previously in Australia and NZ, the use of health claims ix about foods on product
labels and associated advertising had been prohibited under the Australian and
New Zealand Food Regulations. However, from November 1998 to February
2000, ANZFA is piloting a health claim communicating the benefits of folate to
help reduce the prevalence of neural tube defects. The Medicines Act was
amended in December 1998 to permit the use of a folate health claim.
By July 1999, ANZFA had approved the use of the folate health claim on more
than 100 products (28 primary foods and 72 processed foods) which contained at
least 40mcg of folate. However, up to May 1999, no NZ food company or
association had sought approval to carry the claim, and ‘interviews with key
informants in NZ confirmed a low level of interest in the folate health claim’.154
Consumer knowledge about, and reaction to, fortification in NZ
In the Netherlands,149 64% of pregnant women preferred to take folic acid in
fortified food rather than by tablet irrespective of the level of education.
Despite publicity, the increase in the availability of fortified products in NZ, and
differences in study design, two surveys indicate little change in the awareness
about fortification in NZ. In a mail survey in 1998 111, 56% of the respondents
claimed they had heard about fortification, compared to 52% in a Ministry of
Health telephone survey in 1994.155
In 1998, 111 more females (49%) than males (41%) knew about bread fortification,
but there were no differences in awareness across the age groups. The major
sources of information for those that knew about fortification were breakfast
cereal packets (50%), other food packets (42%), television advertisements (39%)
and newspapers/magazines (34%)
It was also found that 62% of female and 53% of male respondents thought it
was very to extremely important to have a choice of buying bakery products with
or without added folic acid.
ix
health claims are messages which make a direct link between eating certain foods as part of
people’s diet and reducing the risk of a specific disease (ANZFA)
Folate, Folic Acid, and Health
43
From 23%-49% of respondents had no opinion about a number of statements on
fortification (table 14), including 49% who ‘neither agreed nor disagreed’ that
‘folate should be added to bread.’ Males over 55 years of age disagreed more
than 15-24 year olds with the statement that ‘folate should be added to bread’.
On the contrary, younger males disagreed more about getting ‘too much
vitamin/mineral by eating foods with added vitamins and minerals’. Both males
and females aged 55-74 years tended to disagree more than 15-24 year olds
with the statement ‘eating foods with added vitamins and minerals would help me
to have a healthy diet’.
Table 14: Level of agreement with statements about vitamins and minerals (mean and standard
deviation)*
Mean (standard deviation)
Statement
Females Males
Total
Healthy people can get all the 3.4 (1.0) 3.6 (0.9) 3.5 (1.0)
vitamins and minerals they need from
food
Where there is a choice, I prefer to 3.2 (0.9) 3.0 (1.0) 3.1 (0.9)
eat foods with vitamins and minerals
added to them
Folate should be added to bread
3.2 (0.9) 3.0 (0.9) 3.1 (0.9)
It is unnatural to add vitamins and 2.8 (1.0) 2.8 (1.0) 2.8 (1.0)
minerals to foods
I can get too much of a 2.9 (1.0) 2.9 (1.0) 2.9 (1.0)
vitamin/mineral by eating foods with
added vitamins and minerals
Eating foods with added vitamins and 3.3 (1.0) 3.2 (1.0) 3.3 (1.0)
minerals would help me to have a
healthy diet
*scale: 1=strongly disagree; 5=strongly agree
source: Bourn and Newton 111
Folate, Folic Acid, and Health
44
Level of fortification
Critical to the acceptance and success of a fortification programme is determining
the appropriate level of fortification. After much debate 55 156 157 158 159 and
reviewing several possible concentrations of fortification up to 350mcg/100g (five
times the replacement level or level of wheat before milling), the US FDA
regulated that the fortification level would be at 140mcg/100g (twice the
replacement level) of all enriched cereal grain products (eg, flour, bread, pasta,
rice etc).
The level of fortification proposed by the Folate Replenishment-Plus Committee
(140mcg/100g) is the same as regulated by the US FDA and implemented on
January 1, 1998.
Modelling by the Centers for Disease Control (Fig 2) has shown that:
fortifying flour with 350mcg/100g would increase average intake by about
0.25mg per day, leaving about 30% of women with total folate intakes below
0.4mg/day. 158 Total folate consumption of all sources (diet, supplements, and
fortification) would be more than 1mg for 15% of the population
fortifying at 140mcg/100g of flour would increase average daily intake of
women in the reproductive age group by about 1mcg and have only modest
effect on NTD rates
On the basis of recent data, Oakley180 (appendix 3) has even suggested that the
concentration of folic acid in fortified grains can be safely increased to 3.5mg or
higher up to almost 7mg/kg grain. The March of Dimes (appendix 4) and the
American College of Preventive Medicine advocate increasing the fortification
level in the USA to at least 350mcgs, but the American College of Medical
Genetics 160 supports an increase to 280mcg/100g of grain.
The American Academy of Pediatrics,161 simply ‘encourages efforts at devising a
program of food fortification to provide all women a daily intake of 400ug of folic
acid.’ while the Teratology Society 162 recommended fortification to a level that
‘will provide 0.4mg of folic acid each day to at least 95% of women in the
reproductive age group.’
After a careful examination of the literature, the Institute of Medicine (IOM) clearly
stated in 1998: 70
‘to reduce the risk of neural tube defects for women capable of
becoming pregnant, the recommendation is to take 400 g of
synthetic folic acid daily, from fortified foods and/or supplements, in
addition to consuming food folate from a varied diet.’
Folate, Folic Acid, and Health
45
The vital difference between the IOM recommendation and the FDA deliberations
is that the former stipulated 400mcg of synthetic folic acid in addition to folate
from a diet. In contrast, the FDA only considered 400mcg of folate from all
sources.
Figure 2: Percentage of women aged 19 to 50 years with mean daily intake of
total folate greater than or equal to specified amount, by grain fortification level
(mcg/100g).
source: Oakley G. In: Willett W. Nutritional Epidemiology; New York: Oxford University Press,
1998
Folate, Folic Acid, and Health
46
Upper target for folate
In 1994, the Australian NHMRC Expert Panel on Folate Fortification Committee
adopted 1000mcg a day as an upper target on intake of natural and synthetic
folate for all population groups. 27 Dietary modelling indicated that with the
proposed level of voluntary fortification, x females aged 25-34 years would be
consuming a mean folate intake of 500mcg a day, with intakes of about 290mcg
a day and 730mcg a day at the 10th and 90th percentiles respectively. Males in
the same age group would, respectively, consume 710mcg, 410mcg and
1040mcg folate a day. It was concluded: ‘Even women who take folate
supplements should have total folate intakes below the 1000mcg upper target’.
The Institute of Medicine
acid per day.
70
has set an upper limit of 1000mcg of synthetic folic
Dietary modelling
Data is available from two dietary modelling exercises in NZ. The Australian and
New Zealand Food Authority (ANZFA) has recently carried out dietary modelling
of potential folate intakes from NZ diets containing folate-fortified supplementary
foods.
Two scenarios were modelled (each with three options):
scenario 1 assumes only the current market proportions of folate-fortified
products within each permitted category (table 11)
scenario 2 assumes all breads, breakfast cereals and fruit juice (not fruit
drinks) are fortified to the maximum permitted amount of folate (table 12)
Fortified fruit juice was included in the models to allow for the product to appear
on the local market in response to the initiative to pilot the folate-neural tube
defect health claim.
Males aged 15-18 and 19-24 years in scenario 2 are the only group who could
potentially exceed the upper intake level of 1000mcg of synthetic folic acid (table
12). However, this would necessitate an extremely high intake from all breads,
breakfast cereals and fruit juice which have been fortified to the maximum
permitted level.
ANZFA concluded from their modelling that:
x
50% RDI per reference quantity of: flour, savoury biscuits, break, breakfast cereals, past, rice, yeast
extracts, and fruit and vegetable juices. ANZFA, 1999
Folate, Folic Acid, and Health
47
‘the results of both models show that at both mean and high levels of
consumption of supplementary foods, the risk of chronic excessive
synthetic folic acid intake (greater than 1mg synthetic folic/day) is
minimal from today’s folate-fortified food supply, and very low from
an even more folate-fortified food supply. The safety of the
Authority’s recommendation is further assured because of the
overestimates built into the model assumptions’.
A recent NZ study by Bourn and Newton
Research Trust, estimated that (table 13):
for the Baking Industry
of women aged 25-44 years:
-
111 163
10% would consume over 400mcg of folate per day if flour was
fortified at 140mg/100g
about half would consume 400mcg of folate per day if all bread
was directly fortified at 70mcg/35g slice
about 10% would consume over 400mcg folate/day if half of bread
consumed was fortified at 70mcg/35g slice
males would have higher folate intakes because of greater consumption
of breads and cereals
The authors concluded that it ‘seems unlikely that the majority of women in
the child-bearing age group will consume the additional 400g folate/day,
unless the appearance of health claims on labels has a significant impact on
food purchases.’
The Institute of Medicine, 70 which set an upper limit of 1000mcg of synthetic
folic acid per day, concluded from dietary modelling in the US that with
current fortification levels and ‘… assuming regular use of an over-thecounter supplement that contains folic acid (ordinarily 400g per dose), it is
unlikely that intake of folic acid would exceed 1,000g on a regular basis for
any of the gender or life-stage groups.’
Folate, Folic Acid, and Health
48
Table 11: ANZFA modelling: scenario 1 for New Zealanders who might consume fortified bread, breakfast cereals and juice
Options
Folate intake from diet containing mean intake of
some fortified breakfast cereals and fruit juice, and
high intake fortified (100mcg/200mL) beverage
supplements and high intake fortified bread
Male
Female
15-18yrs 15-18yrs
859
454
Male
Female
19-24yrs 19-24yrs
708
464
Male
Female
25-44yrs 25-44yrs
649
410
Male
Female
45-64yrs 45-64yrs
525
399
Male
Female
65+yrs 65+yrs
467
329
Maximum amount of added folic acid (from above
scenario covering high intake fortified beverage
supplements and high intake fortified bread)
587
292
502
292
400
252
308
243
276
173
Upper 'safe' intake of added folic acid (mcg/day)
800
800
1000
1000
1000
1000
1000
1000
1000
1000
assume
* 25% of breads and 100% breakfast cereals and 30% fruit juice are fortified to maximum permitted levels
* all dry beverage flavourings fortified at 1000mcg/g
source: ANZFA 1999
Folate, Folic Acid, and Health
49
Table 12: ANZFA modelling: scenario 2 for New Zealanders who regularly consume fortified bread, breakfast cereal and juice
Options
Folate intake from diet containing mean intake of
some fortified breakfast cereals and fruit juice, and
high intake fortified (100mcg/200mL) beverage
supplements and high intake fortified bread
Maximum amount of added folic acid (from above
covering high intake fortified beverage supplements
and high intake fortified bread)
Upper 'safe' intake of added folic acid (mcg/day)
Male
Female
15-18yrs 15-18yrs
1417
794
Male
Female
19-24yrs 19-24yrs
1266
804
Male
Female
25-44yrs 25-44yrs
1110
664
Male
Female
65+yrs 65+yrs
778
566
1145
632
1060
632
861
506
693
515
587
410
800
800
1000
1000
1000
1000
1000
1000
1000
1000
assume
* 100% breads and 100% breakfast cereals and 100% fruit juice are fortified to maximum permitted levels
* all dry beverage flavourings fortified at 1000mcg/100g
source: ANZFA 1999
Folate, Folic Acid, and Health
Male
Female
45-64yrs 45-64yrs
910
671
50
Table 13 :Estimated dietary folate intakes for the 25-44 year age group
Folate (mcg/day)
Percentiles
Gender
Estimated folate intake from
10
50
90
fortified breads (140mcg folate/100g flour)
plus cereals and dietary folate intake
128
252
432
fortified breads (all bread 70mcg folate/35g
slice) plus cereals and dietary folate intake
193
403
584
fortified breads (50% bread 70mcg
folate/35g slice) plus cereals and dietary
folate intake
141
281
462
fortified breads (140mcg folate/100g flour)
plus cereals and dietary folate intake
162
354
625
fortified breads (all bread 70mcg folate/35g
slice) plus cereals and dietary folate intake
227
505
920
fortified breads (50% bread 70mcg
folate/35g slice) plus cereals and dietary
folate intake
175
382
675
Female
Male
source: Bourn and Newton 111 163
Folate, Folic Acid, and Health
51
Risks from Increasing Folic Acid
A major objection to fortification of a staple food (e.g., bread) with folic acid is that
all members of society are exposed to folic acid in larger amounts than is usual.
However, there are instances in public health where fortification has been
effective to prevent rickets (vitamin D), goiter (iodine) and dental caries (fluoride).
Rubella immunisation is offered to both boys and girls although the benefit
accrues to the pregnant women.
A number of potential risks have been identified from increasing the level of
folate, both individually and on a population basis. A traditional view is that diet
should be a sufficient source of nutritients and improvement in diet should be
sufficient without recourse to other means such as supplements. As noted above,
the bioavailability of food folate is considerably less than synthetic folic acid and
women in the reproductive age would have to consume larger amounts of folate
rich foods to obtain the same bioavailability from synthetic folic acid. Moreover,
there have been a number of examples in the history of health where advice
and/or techniques promoted in one era were subsequently shown to be
deterimental to an individual’s health.
There is no current evidence to indicate that the consumption of synthetic folic
acid above 1mg per day is harmful. There are indications that the tolerable safety
level may extend to 7mg. However, it is impossible to give a 100% assurance
that folic acid is totally and completely safe. It is also inappropriate to give such
an assurance because the quest for absolute safety and certainty will negate
most public health programmes and in folic acid, not enable the prevention of up
to 70% of NTDs.
Potential toxic effects from folic acid
multiple births and other reproductive outcomes
The Hungarian randomised control trial of folic acid and the occurrence of the
NTDs 25 found a higher rate of multiple births after periconceptional multivitamin
supplementation.90 164 165 166 In contrast, a recent analysis of UK data 167 from the
MRC Vitamin Study 24 and the Prospective Study of Nutrition, Smoking and
Pregnancy Outcome 168 provided no evidence that folic acid supplementation is
associated with an increased rate of twinning.
The higher rate of conceptions after preconceptional multivitamin
supplementation compared with a placebo-like trace element supplementation
was explained by a 5% shorter time in the achievement of conception.169
Folate, Folic Acid, and Health
52
vitamin B12 deficiency
To some, 170 171 the major fear from fortification is the so-called ‘masking’ effect of
folic acid. Folic acid may correct the anaemia due to vitamin B12 deficiency,
thereby delaying the diagnosis and treatment of the deficiency, and increasing
the risk of permanent neurological damage by allowing the complications to
progress.
To ensure that fortification was safe for all people the FDA restricted the level of
fortification to 140mcg/100g primarily because:156
‘One in five people [aged] 65 to 95 lack sufficient vitamin B12, a
deficiency that can cause pernicious anemia. Extra folic acid can
mask the symptoms of the condition, which may lead to permanent
nerve damage if left untreated.’
Appendices 1 172 and 2
B12 deficiency.
173
provide an evaluation of the issue of folic acid and
There is overwhelming evidence that ‘folic acid is intrinsically safe’.
example:
174
For
Oakley et al 175 have noted there have been no controlled published studies
showing that folic acid consumption resulted in correcting the anaemia and
delaying the diagnosis of vitamin B12 deficiency
‘folic acid even in a full therapeutic dose (eg, 4 or 5mg/d) will neither cause
nor accelerate neurological deterioration in pernicious anemia’ 174
‘there may be more elderly people with biochemical folate deficiency than
vitamin B12 deficiency’ 172
‘the recommended dose [0.4-0.8mg] will not mask the hematological features
of pernicious anemia’ 176
‘a dose of 0.4 to 0.8 mg per day is considered safe for general use’ 35
‘there are no known reports of neurological illness induced by folate
fortification of staple foods in countries where this is practised’ 27
aggravation of the B12 neuropathy is rare in the US, despite 40% of adults
taking vitamin supplements 177
the cause of the neuropathy is B12 deficiency, not folic acid, even in high
dose and it is diagnosed in the absence of anaemia 35. Therefore any effect
Folate, Folic Acid, and Health
53
folate has in delaying the onset of anaemia does not mask or delay the
diagnosis of neuropathy 27
the side-effects of food fortification with folic acid are hypothetical and
avoidable 174
Wald and Bower 178 concluded that:
‘ Concern over the presence or absence of an accompanying
macrocytosis or anaemia is misplaced … The haematological effect
of folic acid in pernicious anaemia should not be used as a reason for
failure to implement adequate folic-acid fortification for prevention of
neural tube defects.’
To Bower and Wald: 173
‘Potential diagnosis problems with vitamin B12 deficiency should be
a reason to ensure that patients with B12 deficiency are being
diagnosed in a timely fashion and treated appropriately, not a reason
to delay or discourage public health strategies to prevent neural tube
defects.’
After a careful review of the literature, Dickinson174 stated ‘that the current
prejudice against universal folic acid fortification of food is based on anecdotal
and scientifically invalid evidence, and that the benefits outweigh the risks... folic
acid is not a neurological poison.’
The Teratology Society 179 believe there is only a ‘theoretical risk’ of folic acid
fortification delaying the diagnosis of pernicious anemia which is ‘clearly
outweighed by the demonstrable benefit of fortification.’
Fortification with vitamin B12 has been suggested 175 180 181 as a solution to the
lingering, and unfounded, concerns over the potential for harm from folic acid
doses greater than 1mg.
Keane et al 182 recommended the use of folic acid-fortified milk in the regular diet
of the elderly population to overcome folic acid deficiency which is common about
elderly and results in anaemia, dementia, and many neurological sequelae. The
Institute of Medicine 70 has recommended daily allowance (RDA) for adults 50
years and older of 2.4mcg of synthetic B12 which can only be obtained from
fortified foods or B12-containing supplements.
In August 1996, the US FDA 183 184 received a citizens petition requesting:
Folate, Folic Acid, and Health
54
every food that was to be fortified with folic acid also be fortified with a
specified amount of vitamin B12 (a minimum 25 micrograms per 100 grams of
the folic-fortified foods)
Herbert and Bigaouette 184 estimated that implementation of this petition would
prevent B12 deficiency, 20% of all heart attacks, 40% of all thrombotic strokes,
and 60% of all peripheral venous thrombosis, and save billions of health care
dollars. Bronstrup et al 185 also suggested B12 cofortification or supplementation
to reduce homocyseine levels.
zinc
There has been debate about supplemental folic acid intake having an adverse
affect on intestinal zinc absorption 186 187 188 189 190. After reviewing the literature,
the Institute of Medicine 70 concluded in 1998 that ‘folic acid supplementation has
either no effect on zinc nutrition or an extremely subtle one.’ For example, in the
MRC trial 24 there was minimal difference between the zinc levels for cases and
controls. Hambidge et al 191 concluded that ‘periconceptional folic acid
supplements do not compromise the zinc status of the mother or the embyro with
respect to zinc intake.’
other potential risks
In 1998 the Institute of Medicine 70 evaluated the potential for folate interactions
with nutrients, other food components, and drugs and found :
no reports demonstrate that the intake of other nutrients increases or
decreases the requirement for folate
certain forms of fibre (eg, wheat bran) may decrease the bioavailability of
certan forms of folate under some conditions, but many forms of fibre had no
adverse effects
survey data of chronic alcoholics suggest that inadequate intake is a major
cause of the folate deficiency observed in chronic alcohol users
low intake rather than an increased requirement may account for the poorer
folate status of smokers
routine use of low doses of nonsteroidal anti-inflammatory drugs has not been
reported to impair folate status
no definitive conclusions can be drawn about the adverse effects of
anticonvulsants on folate status.
Folate, Folic Acid, and Health
55
methotrexate is a folic acid antagonist frequently used successfully in the
treatment of some nonneoplastic diseases (eg, rheumatoid arthritis, psoriasis,
asthma, primary biliary cirrhosis, and inflammatory bowel disease). When
patients are also given high-folate diets or supplemental folate, there is a
significant reduction in toxic effects with no reduction in drug efficacy. It is
recommended that patients undergoing chronic methotrexate therapy for
rheumatoid arthritis increase folate consumption
oral contraceptive use has not been reported to influence folate status
A review of the Hazardous Substances Data Bank 192 shows:
oral folic acid is not toxic to man even with doses as high as 15mg per day,
and there have been no substantiated reports of side effects
allergic reactions to folic acid preparations have been rarely reported and
have included erythma, rash, itching, general malaise, and bronchospastic
respiratory difficulty
adverse gastrointestinal and central nervous system effects have been rarely
reported in patients receiving 15mg of folic acid daily for one month
Monitoring of health outcomes and folate levels in NZ
To maximise the prevention of folic acid-preventable birth defects requires a
passive population strategy that assures that all, or almost all (more than 90%) of
women of reproductive age consume 400mcg of synthetic folic acid per day. Until
such a strategy is implemented, the following monitoring and research would
assist in increasing the number of women consuming the requisite level of folic
acid daily:
monitoring changes in the relative risks of birth defects in relation to the
promotion and implementation of prevention policies
investigating the extent to which available evidence has modified and factors
which have promoted or impeded the use of folic acid or multivitamin
supplements among women of childbearing age
determining additional factors that promote or impede change in the use of
folic acid or multivitamin supplements
what recommendations and advisories have been issued or are being
developed to promote the use of folic acid or multivitamin supplements
Folate, Folic Acid, and Health
56
clarifying the factors considered by the public health authorities when deciding
if and how to promote such recommendations
Monitoring NTDs and other birth defects
NZ Birth Defects Monitoring Programme (NZBDMS) , which has been operating
since 1980, will continue to monitor the prevalence at birth of the NTDs as well as
other birth defects. The NZBDMS routinely collects data on all livebirths born in,
or admitted to, a public hospital. Quarterly and annual tables are submitted to the
International Clearinghouse for Birth Defects Monitoring Systems in Rome and
also supplied to a number of people in NZ.
These livebirth data are annually supplemented with stillbirth data.
The major deficiency in the current ascertainment is the absence of data on
terminations of pregnancy (TOP). However, a joint study with Dr Joanne Dixon,
Geneticist, Capital Coast Health, is investigating various methods in which TOP
data can be included in the NZBDMS. Currently, if the presence of a birth defect
is the reason for the TOP, the specific defect(s) does not have to be specified on
the form.
The NZBDMS is participating in two international studies monitoring the impact of
folic acid recommendations:
Biomed project (PL 963969): NTDs and Primary Prevention Strategies
(Funded by the European Union). Twenty-four birth defect registries and
monitoring programmes are participating in this study which has the
objectives:
-
-
-
to investigate the reasons why different countries, working from the
same published data, adopted different policies (or none) regarding
the primary prevention of NTDs through the use of folic acid
to determine the extent to which such policies (or lack) are being
implemented
to determine time trends in NTD prevalence in the same countries
during the period likely to be influenced by such policies (or absence
of policy)
to determine whether different strategies have been associated with
different time trends in NTD prevalence
The study will be completed in 2001
Prevention Strategies based on periconceptional folic acid supplementation
(Funded by the Centers for Disease Control and Prevention, USA). Twenty
programmes are involved in this study which has the following objectives:
Folate, Folic Acid, and Health
57
to describe and compare public health policies regarding the use of folic
acid or multivitamin supplements for the primary prevention of NTDs and
other birth defects
evaluate the extent to which current public health policies are being
implemented and explore the factors involved in the compliance and
acceptance of such policies
compare the prevalence of NTDs, oral clefts, cardiac defects, and limb
defects before and after the initiation of folate prevention strategies
The project will be completed in 2002.
Monitoring folate levels
The Ministry of Health and ANZFA are funding a project by the University of
Otago to establish baseline data among women aged 20-44 years (n=210) and
boys aged 14-19 years (n=140) on: 193
folate status, using dietary and biochemical assessment, for monitoring the
impact of the folate health claim
knowledge, attitudes and behaviours about the folic acid and the health claim
Draft results from the study are scheduled for release by the end of November
1999. The Ministry has expressed a wish to implement a folate monitoring
programme.
Impact of folic acid supplementation and fortification policies
An international study conducted over 1987-mid-1996 found that changes in the
time trend of NTDs were not due to the introduction of national policies of folate
supplementation 194
Since the 1992 folic acid recommendation in the UK,195 the number of folic acid
prescriptions dispensed and preparations sold over the counter increased
considerably.196 However, there has been no concomitant change in the
incidence of NTDs (since the early 1970s), either nationally or regionally. 197
Explanations include incorrect use of the supplement and the limited impact of a
health education campaign which reinforce the need for a fortification
programme. 198
Folate, Folic Acid, and Health
58
Since fortification in the USA, NTD rates in North Carolina have shown little
change, 199 but elsewhere folate levels have risen since fortification. 200 201
The lack of visible evidence of a decline in NTD rates since folic acid
recommendations were made and fortification commenced should not detract
from continuing efforts to increase the intake of folic acid. Oakley 202 has argued
strongly that such is likely to be the result of ‘the failure to implement effective
programs for protection against folic acid-preventable birth defects.’
Folate, Folic Acid, and Health
59
Conclusion
There is no scientific evidence that the fortification of bread with synthetic folic
acid at the level of 140mcg/100g presents any risk to any group in the NZ
population. Dietary modelling in NZ and the USA indicates that it is highly unlikely
that the intake of folic acid would exceed 1,000mcg (the upper threshold) on a
regular basis for any age-gender groups. The NZ programmes for monitoring the
effect of a fortification programme on health outcomes are of similar standard to
those elsewhere. However, there is currently no provision to monitor the folate
status of the population.
However, it is not certain that fortification at 140mcg/100g will be sufficient to
prevent NTDs occurring. Modelling data from the USA indicates that the
proposed level of fortification will still require women to take supplements as well
as generally improving their diet.
There can be no doubt that implementing the proposal to fortify some breads to
140mcg/100g should only be viewed as a first step towards:
increasing the level of fortification to at least the level permitted by the Food
Regulations (285mcg/100g - see appendices 3,4,5)
encouraging manufacturers to increase the level of folic acid fortification in
breakfast cereals
regulating folic acid fortification
A fortification programme, will not only assist in preventing NTDs but also offer
other advantages without risk: 27
the folate status of the NZ population, regardless of age, gender, ethnic
group, and socio-economic status
folate intakes will be increased without a change of dietary behaviour or
having to remember to take supplements
folic acid will be provided in a continuous and passive manner
folate deficiency in the elderly would be corrected
current evidence indicates that improving folate status could reduce the risk of
other major health outcomes such as cardiovascular disease and colorectal
cancer. Riddell et al 86 concluded that in NZ:
Folate, Folic Acid, and Health
60
‘Fortification with folic acid, recommended primarily to reduce the
risk of congenital malformation may also help to reduce
cardiovascular risk.’
Folate, Folic Acid, and Health
61
References
1
Oakley GP. Folic acid-preventable spina bifida and anencephaly. JAMA 1993;269:1292-3
Ministry of Health. The Burden of Disease and Injury. In: The Health of New Zealanders.
Chapter 10. draft. 1999
3 Borman B, Cryer C. Fallacies of international and national comparisons of disease occurrence in
the epidemiology of neural tube defects. Teratology 1990;42:405-12
4 Borman B. Risk Factors in the Prevalence of Anencephalus and Spina Bifida in New Zealand.
Unpubl. PhD thesis, University of Otago, 1987
5 Borman B, Howard JK, Chapman CJ. The epidemiological study of birth defects. NZ Med J
1984;97:602
6 Elwood JM, Little J, Elwood JH. Epidemiology and Control of Neural Tube Defects. Oxford:
Oxford University Press; 1992
7 Moore CA, Li S, Li Z et al. Elevated rates of severe neural tube defects in a high-prevalence
area in North China. Am J Med Genet 1997;73:113-8
8 Elwood JM, Elwood JH. Epidemiology of Anencephalus and Spina Bifida. Oxford: Oxford
University Press;1980
9 Hibbard ED, Smithells RW. Folic acid metabolism and human embryopathy. Lancet 1965;i:1254
10 Smithells RW, Sheppard S, Schorah CJ. Vitamin deficiencies and neural tube defects. Arch Dis
Child 1976;51:944-50
11 Smithells RW, Sheppard S, Schorah CJ et al. Possible prevention of neural-tube defects by
periconceptional vitamin supplementation. Lancet 1980;i:339-40
12 Smithells RW, Nevin NC, Seller MJ et al. Further experience of vitamin supplementation for
prevention of neural tube defect recurrences. Lancet 1983;i:1027-31
13 Laurence KM, James N, Miller MH et al. Double-blind randomised controlled trial of folate
treatment before conception to prevent recurrence of neural-tube defects. Br Med J
1981;282:1509-11
14 Laurence KM, Campbell H, James NE. The role of improvement in the maternal diet and
preconceptional folic acid supplementation in the prevention of neural tube defects. In Dobbing J
(ed): Prevention of Spina Bifida and Other Neural Tube Defects. London: Academic Press;1983:
85-106
15 Dobbing J (ed). Prevention of Spina Bifida and Other Neural Tube Defects. London: Academic
Press, 1983
16 Little J, Elwood JM. Epidemiology of neural tube defects. In: Kiely M (ed). Reproductive and
Perinatal Epidemiology. Boca Raton: CDC Press; 1991:251-336
17 Winship KA, Cahal DA, Weber JCP et al. Maternal drug histories and central nervous system
anomalies. Arch Dis Child 1984;59:1052-60
18 Mulinare J, Cordero JF, Erickson JD et al. Periconceptional use of multivitamins and the
occurrence of neural tube defects. JAMA 1988;260:3141-5
19 Milunsky A, Jick H, Jick S et al. Multivitamin/folic acid supplementation in early pregnancy
reduces the prevalence of neural tube defects. JAMA 1989;262:2847-52
20 Bower C, Stanley FJ. Dietary folate as a risk factor for neural tube defects: evidence from a
case-control study in Western Australia. Med J Aust 1989;150:613-9
21 Vergel RG, Sanchez LR, Heredero BL et al. Primary prevention of neural tube defects with folic
acid supplementation: Cuban experience. Prenat Diagn 1990;100:149-52
22 Yates JRW, Ferguson-Smith MA, Shenkin A et al. Is disordered folate mechanism the basis for
the genetic predisposition to neural tube defects? Clin Genet 1987;31:279-87
23 Mills JL, Rhoads GG, Simpson JL et al. The absence of a relation between the
periconceptional use of vitamins and neural tube defects. N Eng J Med 1989;321:430-5
24 MRC Vitamin Study Research Group. Prevention of neural tube defects: results from the
Medical Research Council Vitamin Study. Lancet 1991:338:131-7
25 Czeizel AE, Dudas I. Prevention of the first occurrence of neural tube defects by
periconceptional vitamin supplementation. N Engl J Med 1992:327:1832-5
26 Elwood JM. Prevention of neural tube defects: clinical and public health policy. NZ Med J
1993;106:517-8
2
Folate, Folic Acid, and Health
62
27
NHMRC. Folate Fortification. Canberra: National Health and Medical Research Council, 1994
Kirke PN, Daly LE, Elwood JH. A randomised trial of low dose folic acid to prevent neural tube
defects. Arch Dis Child 1992;67:1442-6
29 Bower C, Stanley FJ. Periconceptional vitamin supplementation and neural tube defects;
evidence from a case-control study in Western Australia and a review of recent publications. J
Epidemiol Community Health 1992;46;157-61
30 Werler MM, Shapiro S, Mitchell AA. Periconceptional folic acid exposure and risk of occurrent
neural tube defects. JAMA 1993;269:1257-61
31 Shaw GM, Schaffer D, Velie EM, et al. Periconceptional vitamin use, dietary folate, and the
occurrence of neural tube defects. Epidemiology;1995:219-26
32 Friel JK, Frecker M, Fraser FC. Nutritional patterns of mothers of children with neural tube
defects in Newfoundland. Am J Med Genet 1995;55:195-9
33 Wong W, Chang A. Neural-tube defects and folic acid status in Hong Kong Chinese. Br J
Obstet Gynaecology 1993;100:1065
34 Berry RJ, Li Z, Erickson JD, Li S, et al. Prevention of neural-tube defects with folic acid in
China. N Engl J Med 1999;341:1485-90
35 Wald NJ. Folic acid and neural tube defects: the current evidence and implications for
prevention. In: Bock G, Marsh J (eds): Neural Tube Defects, Ciba Foundation Symposium 181,
1994; Chichester: John Wiley & Sons: 192-211
36 Lumley J, Watson L, Watson M et al. Periconceptional supplementation with folate and/or
multivitamins for preventing neural tube defects (Cochran Review). In: The Cochrane Library,
Issue 2, 1999. Oxford: Update Software
37 Centers for Disease Control and Prevention. MMWR August 2 1991;40:513-6
38 Centres for Disease Control and Prevention. MMWR September 11 1992;41:1-7
39 Cornel MC, Erickson JD. Comparison of national policies on periconceptional use of folic acid
to prevent spina bifida and anencephaly (SBA). Teratology 1997;55:134-7
40 Tell GS, Vollset SE, Lande B et al. Folate and health - new knowledge and new
recommendation. Tidsskr Nor Laegeforen 1998;118:3155-60
41 Erickson JD. Center for Disease Control and Prevention, personal communication, 1999
42 Khoury MJ, Shaw, Moore CA et al. Does periconceptional multivitamin use reduce the risk of
neural tube defects associated with other birth defects? Data from two population-based casecontrol studies. Am J Med Genetics 1996;61:30-6
43 Shaw GM, Lammer EJ, Wassereman CR et al. Risks of orofacial clefts in children born to
women using multivitamins containing folic acid periconceptionally. Lancet 1995;346:393-6
44 Tolarova M, Harris J. Reduced recurrence of orofacial clefts after periconceptional
supplementation with high-dose folic acid and multivitamins. Teratology 1995;51:71-8
45 Czeizel AE, Toth M, Rockenbauer M. Population-based case control study of folic acid
supplementation during pregnancy. Teratology 1996;54:345-51
46 Czeizel AE. Reduction of urinary tract and cardiovascular defects by periconceptional
multivitamin supplementation. Am J Med Genet 1996;62:179-83
47 Botto LD, Mulinare J, Erickson JD. Occurrence of congenital heart defects in relation to
maternal multivitamin use. Am J Epidemiol (in press)
48 Yang Q, Khoury MJ, Olney RS et al. Does periconceptional multivitamin use reduce the risk for
limb deficiency in offspring? Epidemiology 1997;8:157-61
49 Werler MM, Hayes C, Louik C et al. Multivitamin supplementation and risk of birth defects. Am
J Epidemiol 1999;150:675-82
50 Li Dk, Daling JR, Mueller BA, et al. Periconceptional multivitamin use in relation to the risk of
congenital urinary tract anomalies. Epidemiology 1995;6:212-8
51 Li S, Ji C, Zhang Z. Maternal perinconception folic acid supplementation and reduced risk for
congenital heart defects. Presented: Scientific session, Annual Meeting, International
Clearinghouse for Birth Defects Monitoring Systems, Strasbourg, 1999
52 James SJ, Pogribna M, Pogribny IP et al. Abnormal folate metabolism and mutation in the
methylenetetrahydrofolate reductase gene may be maternal risk factors for Down syndrome. Am
J Clin Nutr 1999;70:429-30
28
Folate, Folic Acid, and Health
63
53
Hayes C, Werler MM, Willett WC, et al. Case-control study of periconceptional folic acid
supplementation and oral clefts. Am J Epidemiol 1996;143:1229-34
54 Czeizel AE. Limb-reduction defects and folic acid supplementation. Lancet 1995;345:932
55 Oakley GP, Erickson JD, James LM et al. Prevention of folic acid-preventable spina bifida and
anencephaly. In: Bock G, Marsh J (eds): Neural Tube Defects, Ciba Foundation Symposium 181,
1994; Chichester: John Wiley & Sons:223-31.
56 Werler MM, Louik C, Shapiro S et al. Prepregnant weight in relation to risk of neural tube
defects. JAMA 1996;275:1089-92
57 Shaw GM, Velie EM, Schaffer D. Risk of neural tube defect-affected pregnancies among obese
women. JAMA 1996;275:1093-6
58 Lashner BA, Provencher KS, Seidner DL et al. The effect of folic acid supplementation on the
risk for cancer or dysplasis in ulcerative colitis. Gastroenterology 1997;112:29-32
59 Giovannucci E, Stampfer MJ, Colditz GA et al. Multivitamin use, folate, and colon cancer in
women in Nurses’ Health Study. Ann Inter Med 1998;129:517-24.
60 Glynn SA, Albanes D, Pietinen P et al. Colorectal cancer and folate status: a nested casecontrol study among male smokers. Cancer Epidemiol Biomarkers Prev 1999;5:487-94
61 Kato I, Dnistrian AM, Schwartz M et al. Serum folate, homocystein and colorectal cancer risk in
women: a nested case-control study. Br J Cancer 1999;79:1917-22
62 Freudenheim JL, Graham S, Marshall JR et al. Folate intake and carcinogenesis of the colon
and rectum. Int J Epidemiol 1991;20:368-74
63 Baron JA, Sandler RS, Haile RW et al. Folate intake, alcohol consumption, cigarette smoking,
and risk of colorectal adenomas. J Natl Cancer Inst 1998;90:57-62
64 World Cancer Research Fund. Food, Nutrition and the Prevention of Cancer: a Global
Perspective. World Cancer Research Fund and the American Institute for Cancer Research.
Washington DC: American Institute for Cancer Research, 1997
65 Zhang S, Hunter DJ, Hankinson SE et al. A prospective study of folate intake and the risk of
breast cancer. JAMA 1999;281:1632-7
66 Wu K, Helzlsouer KJ, Comstock GW et al. A prospective study on folate, B12, and pyridoxal 5’phosphate (B6) and breast cancer. Cancer Epidemiol Biomarkers Prev 1999;8:209-17
67 Potischman N, Swanson CA, Coates RJ et al. Intake of food groups and associated
micronutrients in relation to risk of early-stage breast cancer. Int J Cancer 199;30:315-2
68 Albrecht C, Everett K. The Role of Folic Acid in the Prevention of Cancer. Presented: to the
Directorate: Nutrition of the Department of Health, South Africa, 1999
69 Carew M. The role of folic acid in the prevention of cervical neoplasia: a review of the
literature.Chronic Diseases in Canada 1995;16:111-6
70 Institute of Medicine. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B
6,
Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. A report of the Standing Committee on
the Scientific Evaluation of Dietary Reference Intakes and its Panel on Folate, Other B Vitamins,
and Choline and Subcommittee on Upper Reference Levels of Nutritients. Washington DC:
National Academy Press, 1998
71 Ebly EM, Schaefer JP, Campbell NR et al. Folate status, vascular disease and cognition in
elderly Canadians. Age Ageing 1998;27:485-91
72 Hassing L, Wahlin A, Winbald B et al. Further evidence on the effects of vitamin B12 and folate
levels on episodic memory functioning: a population-based study of healthy very old adults. Biol
Psychiatry 1999;45:1472-80
73 Houston DK, Johnson MA, Nozza RJ et al. Age-related hearing loss, vitamin B-12, and folate in
elderly women. Am J Clin Nutr 1999;69:564-71
74 Clarke R, Smith AD, Jobst KA et al. Folate, vitamin B12, and serum total homocysteine levels
in confirmed Alzheimer disease. Arch Neurol 1998;55:1449-55
75 Boushey CJ, Beresford SAA, Omenn GS et al. A quantitative assessment of plasma
homocysteine as a risk factor for vascular disease. JAMA 1995;274:1049-57
76 Homocysteine Lowering Trialists’ Collaboration. Lowering blood homocysteine with folic acid
based supplements: meta-analysis of randomised trials. Br Med J 1998;316:894-8
77 Rimm EB, Willet WC, Hu FB et al. Folate and vitamin B6 from diet and supplements in relation
to risk of coronary heart disease among women. JAMA 1998;279:359-64
Folate, Folic Acid, and Health
64
78
Oakley GP. Eat right and take a multivitamin. N Engl J Med 1998;338:1060-1
Tucker KL, Mahnken B, Wilson PW. Folic acid fortification of the food supply. Potential benefits
and risks for the elderly population. JAMA 1996;276:1879-85
80 Verhoef P, Stampfer MJ, Buring JE et al. Homocysteine metabolism and risk of moycardial
infarction: relation with vitamins B6, B12, and folate. Am J Epidemiol 1996;143:845-59
81 Kittner SJ, Giles WH, Macko RF et al. Homocy(e)ine and risk of cerebral infarction in a biracial
population: the stroke prevention in young women study. Stroke 1999;30:1554-60
82 Folsom AR, Nieto J, McGovern PG et al. Prospective study of coronary heart disease incidence
in relation to fasting total homocysteine, related genetic polymorphisms, and B vitamins.
Circulation 1998;98:204-10.
83 Morrison HI, Schaubel D, Desmeules M et al. Serum folate and risk of fatal coronary heart
disease. JAMA 1996;275:1893-6
84 National Heart Foundation. Web site: www.heartfoundation.com.au/docs/pp5.htm
85 Malinow MR, Bostom AG, Krauss RM. Homocyst(e)ine, diet, and cardiovascular diseases. A
statement for healthcare professionals from the Nutrition Committee, American Heart Association.
Circulation 1999;99:178-82.
86 Riddell LJ, Chisholm A, Duncan A et al. Homocysteine levels in healthy New Zealanders and
those with vascular disease. NZ Med J 1999;112:438-42.
87 Havranek EP. Primary prevention of CHD: nine ways to reduce risk. Am Fam Physician
1996;59:1455-66
88 Kuller LH, Evans RW. Homocysteine, vitamins, and cardiovascular disease. Circulation
1998;98:196-9
89 Scholl TO, Hediger ML, Bendich A et al. Use of multivitamin/mineral prenatal supplements:
influence on the outcome of pregnancy. Am J Epidemiol 1997;146:134-41
90 Czeizel AE, Dudas I, Metneki J. Pregnancy outcomes in a randomised controlled trial of
periconceptional multivitamin supplementation. Final report. Arch Gynecol Obstet 1994;255:131-9
91 Stefanidis K, Stefos T, Vekris A et al. Folate status during labour: relationship with pregnancy
outcome. J Matern Fetal Med 1999;8:61-3
92 Dudas I, Rockenbauer M, Czeizel AE. The effect of preconceptional multivitamin
supplementation on the menstrual cycle. Arch Gynecol Obstet 1995;256:115-23
93 Czeizel AE, Rockenbauer M, Susansky E. No change in sexual activity during preconceptional
multivitamin supplementation. Br J Obstet Gynaecol 1996;103:569-73
94 ICBDMS. Annual Report 1999 with data for 1997. Rome: International Clearinghouse for Birth
Defects Monitoring Systems, 1999
95 Borman B, Cryer C. The prevalence of anencephalus and spina bifida in New Zealand. J
Paediatr Child Health 1993;29:282-8
96 Borman B, Howard JK, Chapman CJ. Secular trends in the prevalence of anencephalus in New
Zealand. NZ Med J 1986;99:183-5
97 Borman B, Smith AH, Howard JK. Risk factors in the prevalence of anencephalus and spina
bifida in New Zealand. Teratology 1986;33:221-30
98 Singh S, Elliott RB. Prevention of Spina Bifida in New Zealand. Unpubl. University of Auckland,
1997
99 Waitzman NJ, Romano PS, Scheffler RM. Estimates of the economic costs of birth defects.
Inquiry 1994;31:188-205
100 Waitzman NJ, Scheffler RM, Romano PS. The Cost of Birth Defects. Estimates of the Value of
Prevention. Lanham: University Press of America, Inc. 1996
101 NZ Sunday Times. 10 January 1993
102 Dixon JW, Murray HG. Folic acid and neural tube defects. NZ Med J 1993; 106:90
103 Elwood JM. Easy path to prevention. NZ Herald, 28 July 1993
104 PHC. Reducing the chances of spina bifida by taking folic acid. Letter to Health Professionals.
Wellington: Public Health Commission, 28 September 1993
105 PHC. Low dose folic acid tablets to prevent spina bifida. Letter to Health Professionals.
Wellington: Public Health Commission, June 1995
106 PHC. Planning for Pregnancy. Folic Acid and Spina Bifida. Pamphlet code 4147. Wellington:
Public Health Commission
79
Folate, Folic Acid, and Health
65
107
CCS. Folic Acid - point eight available. Access. Wellington: New Zealand CCS, August 1995
PHC. Congenital and Inherited Conditions. The Public Health Commission’s Advice to the
Minister of Health, 1994-95. Wellington: Public Health Commission, 1995
109 PHC. Progress on Health Outcome Targets. The State of the Public Health in New Zealand,
1995. Wellington: Public Health Commission, 1995
110 PHC. National Plan of Action for Nutrition. The Public Health Commission’s Advice to the
Minister of Health, 1994-95. Wellington: Public Health Commission, 1995
111 Bourn D, Newton R, Consumer Attitudes on the Fortification of New Zealand Bakery Products.
A Report Produced for the Baking Industry Research Trust. Dunedin: Department of Consumer
Sciences, University of Otago, 1998
112 Truswell AS, Stewart A (eds). Recommended Nutrient Intakes; Australia papers. Canberra:
Australian Professional Publications, 1990
113 Russell D, Parnell W, Wilson N et al. NZ Food: NZ People. Key Results of the 1997 National
Nutrition Survey. Wellington: Ministry of Health, 1999
114 Howarth C, Parnell W, Birkbeck J, et al. Life in New Zealand Commission Report. Volume VI:
Nutrition. Dunedin: University of Otago, 1991
115 Salmond C, Crampton P, Sutton F. NZDep96: Index of Deprivation. Research Report No 8:
Wellington: Health Services Research Centre, 1998
116 Skeaff M, Mann J. Should folate be added to flour to prevent neural tube defects? NZ Med J
1998;111:417-8
117 Wald NJ, Bower C. Folic acid and the prevention of neural tube defects. Br Med J
1995;310:1019-20
118 Elwood JM. Folic acid prevents neural tube defects. Med J Aust 1991;155:579-80
119 Cuskelly GJ, McNulty H, Scott JM. Effect of increasing dietary folate on red-cell folate:
implications for prevention of neural tube defects. Lancet 1996;347:657-9
120 Ministry of Health. Food and Nutrition Guidelines for Healthy Adolescents: A background
paper. Wellington: Ministry of Health, 1998
121 Bendich A, Mallick R, Leader S. Potential health economic benefits of vitamin
supplementation. West J Med 1997;166:306-12
122 Watson P, McDonald B. Nutrition During Pregnancy. Report to the Ministry of Health. Albany:
Massey University, 1999
123 supplied by IMS Health, Auckland
124 Forman R, Singal N, Perelman V et al. Folic Acid and prevention of neural tube defects - a
study of Canadian mothers of infants with spina bifida. Clinical & Investigative Medicine
1996;19:195-201
125 Neimanis IM, Paterson JM, Bain E. Preventing neural tube defects. Survey of preconceptional
use of folic acid. Can Fam Physician 1999;45:1717-22
126 McDonnell R, Johnson Z, Doyle A. Folic acid knowledge and use among expectant mothers in
1997: a comparison with 1996. Ir Med J 1999;92:296-9
127 McDonnell R, Johnson Z, Doyle A et al. Determinants of folic acid knowledge and use among
antenatal women. J Public Health Med 1999;21:145-9
128 Sayers GM, Hughes N, Scallan E et al. A survey of knowledge and use of folic acid among
women of child-bearing age in Dublin. J Pub Health Med J 1997;19:328-32
129 Wild J, Schorah CJ, Maude K et al. Folate intake in young women and their knowledge of
preconceptional folate supplementation to prevent neural tube defects. Eur J Obstet Gynecol
Reprod Biol 1996;70:185-9
130 Castilla EE, Dutra MG. Folate awareness among South American women. Lancet
1997;349:735
131 McGovern E, Moss H, Grewal G et al. Factors affecting the use of folic acid supplements in
pregnant women in Glasgow. Br J Gen Pract 1997;47:635-7
132 Ringel S, Lahat E, Elizov T et al. Awareness of folic acid for neural tube defect prevention
among Israeli women. Teratology 1999;60:29-32
133 Kloeblen AS. Folate knowledge, intake from fortified grain products, and periconceptional
supplemention patterns of a sample of low-income pregnant women according to the Health
Belief Model. J Am Diet Assoc 1999;99:33-8
108
Folate, Folic Acid, and Health
66
134
Perez-Escamilla R, Himmelgreen D, Segura-Millan S et al. Knowledge of folic acid and neural
tube defects among inner city residents: have they heard about it. J Am Diet Assoc 1999;99:80-3
135 Bower C, Knowles S, Nicol D. Changes in folate supplementation, and in serum and red cell
folate levels in antenatal patients over the course of a health promotion project for the prevention
of neural tube defects. Aust NZ J Obstet Gynaecol 1997;37:267-71
136 Brandenburg H, Trass MA, Laudy J et al. Periconceptional use of folic acid amongst women of
advanced maternal age. Pernat Diagn 1999;19:132-5
137 Clark NAC, Fisk NM. Minimal compliance with the Department of Health recommendation for
routine folate prophlaxis to prevent fetal neural tube defects. Br J Obstet Gynaecol 1994;101:70910
138 Balen A. Minimal compliance with the Department of Health recommendation for routine folate
prophlaxis to prevent fetal neural tube defects. Br J Obstet Gynaecol 1995;102:171
139 Odibo AO, Greenwood C, Selinger M. Minimal compliance with the Department of Health
recommendation for routine folate prophlaxis to prevent fetal neural tube defects. Br J Obstet
Gynaecol 1995;102:171
140 Nelson-Piercy C, de Swiet M. Minimal compliance with the Department of Health
recommendation for routine folate prophlaxis to prevent fetal neural tube defects. Br J Obstet
Gynaecol 1995;102:171
141 Krischer J. Knowledge about folic acid and the prevention of neural tube defects in two general
practice populations. Br J General Practice 1997;47:231-2.
142 Public Health and Development Division, Department of Human Services, Victoria, Australia.
Victorian Folate Campaign 1999. Web site: www.dhs.gov.au/phb/folate/notavers.htm
143 Petrini JR, Damus K, Johnston RB et al. Knowledge and use of folic acid by women of
childbearing age - United States, 1995 and 1998. MMWR 1999;48:325-7
144 Bonin MM, Bretzlaff JA, Therrien SA et al. Knowledge of periconceptional folic acid for the
prevention of neural tube defects. The missing links. Northeastern Ontario Primary Care
Research Group. Arch Fam Med 1998;7:438-42
145 Koren G. Periconception folic acid supplementation. Knowledge and practice of Canadian
family physicians. Can Fam Phys 1997;43:851-2
146 Sayers G, Scallan E, McDonnell R et al. Knowledge and use of periconceptional folic acid
among antenatal patients. Ir Med J 1997;90:236-8
147 Broome K. Folic acid campaign and evaluation - Southwestern Virginia, 1997-1999.
MMWR1999;48:914-7
148 Brugman E van der Pal-de-Bruin KM, den Ouden Al et al. Folic acid use for women desiring
offspring: the family physician’s response. Ned Tijdschr Geneeskd 1997;141:1653-7
149 de Walle HEK, van der Pal KM, de Jong-van den Berg LTW et al. Effect of mass media
campaign to reduce socioeconomic differences in women’s awareness and behaviour concerning
use of folic acid: a cross sectional study. Br Med J 1999;319:291-2
150 Bower C, Blum L, O’Daly K et al. Promotion of folate for the prevention of neural tube defects:
knowledge and use of periconceptional folic acid supplements in Western Australia, 1992 to
1995.
Aust N Z J Public Health. 1997;21(7):716-21.
151 Boon C, Hull S. Preconceptional supplementation is impractical. Br Med J 1995:311:256-7
152 National Health Committee. The Social, Cultural and Economic Determinants of Health in New
Zealand: Action to Improve Health. Wellington: National Advisory Health Committee on Health
and Disability, 1998
153 Romano PS, Waitzman NJ, Scheffler RM. Folic acid fortification of grain: an economic
analysis. Am J Public Health 1995;85:667-76
154 ARTD Management and Research Consultants. Process Evaluation of the Management
Framework for the Folate/Neural Tube Defect Health Claim Pilot. Final Report. July 1999
155 Lungley S. Survey of Attitudes of New Zealand Population to Restoration and Fortification of
Foods. Wellington: New Zealand Health Information Service, Ministry of Health, 1994. Cited in:
Bourn D, Newton R. Consumer Attitudes on the Fortification of New Zealand Bakery Products. A
Report Produced for the Baking Industry Research Trust. Dunedin: Department of Consumer
Sciences, University of Otago, 1998
Folate, Folic Acid, and Health
67
156
Williams RD. FDA proposes folic acid fortification. FDA Consumer May 1994
Horton R. Fighting about folate. Lancet 1994;344:1696
158 Oakley GP, Erickson JD, Adams MJ. Urgent need to increase folic acid consumption. JAMA
1995;274:171-8
159 Gaull GE, Testas CA, Thomas PR et al. Fortification of the food supply with folic acid to
prevent neural tube defects is not yet warranted. J Nutr 1996;126:773S-780S
160 Crandall BF, Corson VL, Evans MI et al. American College of Medical Genetics statement of
folic acid: fortification and supplementation. Am J Med Genet 1998;78:381
161 American Academy of Pediatrics, Committee on Genetics. Folic acid for the prevention of
neural tube defects. Pediatrics 1999;104;325-7
162 Teratology Society. Teratology Society Consensus Statement on Use of Folic Acid to Reduce
the Risk of Birth Defects. Teratology 1997;55:381
163 Bourn DM, Newton R. Estimated dietary folate intakes and consumer attitudes to folate
fortification of cereal products in New Zealand. (submitted). Quoted with permission of the
authors
164 Czeizel AE. Controlled studies of multivitamin supplementation on pregnancy outcomes. Ann
NY Acad Sci 1993;678:266-75
165 Czeizel AE, Metneki J, Dudas I. Higher rate of multiple births after periconceptional
multivitamin supplementation: an analysis of causes. Acta Genet Med Gemellol (Roma)
1994;43:175-84
166 Czeizel AE, Metneki J, Dudas I. Higher rate of multiple births after periconceptional vitamin
supplementation.. N Engl J Med 1994;330:1687-8
167 Mathews F, Murphy M, Wald NJ et al. Twinning and folic acid use. Lancet 1999;353:291-2
168 Mathews F, Yudkin P, Neil A. Folates in the periconceptional period: are women getting
enough? Br J Obstet Gynaecol 1998;105:954-9
169 Czeizel AE, Metneki J, Dudas I. The effect of preconceptional multivitamin supplementation on
fertility. Int J Vitam Nutr Res 1996;66:55-8
170 Brantigan CO. Folate supplementation and the risk of masking vitamin B
12 deficiency. JAMA
1997;277:884
171 Reynolds EH. Folate has potential to cause harm. Br Med J 1995;311:257
172 Truswell AS. Appendix 4: Could a general increase in folate intake mask or accelerate the
development of neurological disease due to vitamin B12 deficiency? In: NHMRC. Folate
Fortification. Canberra: National Health and Medical Research Council, 1994
173 Bower C, Wald NJ. Vitamin B
12 deficiency and the fortification of food with folic acid. Eur J Clin
Nutr 1995:49:787-93
174 Dickinson CP. Does folic acid harm people with vitamin B
12 deficiency? Q J Med 1995;88:35764
175 Oakley GP, Adams MJ, Dickinson CM. More folic acid for everyone, now. J Nutr 1996;751S755S
176 Rieder MJ. Prevention of neural tube defects with periconceptional folic acid. Fetal Drug
Therapy 1994;21:483-503
177 Metz J. Folate, B , and neural tube defects. Med J Aust 1995;163:231-2.
12
178 Wald NJ, Bower C. Folic acid, pernicious anaemia, and prevention of neural tube defects.
Lancet 1994;343;307
179 Teratology Society. Teratology society consensus statement on use of folic acid to reduce the
risk of birth defects. Teratoogy 1997;55:381
180 Oakley GP. Let’s increase folic acid fortification and include vitamin B-12. Am J Clin Nutr
1997;65:1889-90
181 Ubbink JB. Should all elderly people receive folate supplements? Drugs Aging 1998;13:415-20
182 Keane EM, O’Broin S, Kelleher B et al. Use of folic acid-fortified milk in the elderly population.
Gerontology 1998;44:336-9
183 US Department of Agriculture, Food and Drug Administration. Notes from the Food Advisory
Committee Meeting, 25 September, 1997
157
Folate, Folic Acid, and Health
68
184
Herbert V, Bigaouette J. Call for endorsement of a petition to the Food and Drug
Administration to always add vitamin B-12 to any folate fortification or supplement. Am J Clin Nutr
1997;65:572-3
185 Bronstrup A, Hayes M, Prinz-Langenohl R, et al. Effects of folic acid and combinations of folic
acid and vitamin B-12 on plasma homocysteine concentrations in health, young women. Am J
Clin Nutr 1998;68:1104-10
186 Milne DB, Canfield WK, Mahalko JR et al. Effect of oral folic acid supplements on zinc, copper,
and iron absorption and excretion. Am J Clin Nutr 1984;39:535-9
187 Butterworth CE, Tamura T. Folic acid safety and toxicity: a brief review. Am J Clin Nutr
1989;50:353-8
188 Milunsky A, Morris JS, Jick H et al. Maternal zinc and fetal neural tube defects. Teratology
1992;46:341-8
189 Kauwell GP, Bailey LB, Gregory JF et al. Zinc status is not adversely affected by folic acid
supplementation and zinc intake does not impair folate utilization in human subjects. J Nutrition
1995;125:66-72
190 Hansen DK, Grafton TF, Dial SL et al. Effect of supplemental folic acid on valproic acidinduced embryotoxicity and tissue zinc levels in vivo. Teratology 1995;52:277-85
191 Hambidge M, Hackshaw A, Wald N. Neural tube defects and serum zinc. Br J Obstet
Gynaecol 1993;100:746-9
192 Hazardous Substances Data Bank (on CD). Micromedex, 1999
193 Skeaff M. Department of Human Nutrition, University of Otago, personal communication, 1999
194 Rosano A, Smithells D, Cacciani L et al. Time trends in neural tube defects prevalence in
relation to preventive strategies: an international study. J Epidemiol Community Health
1999;53:630-5
195 Report from an Expert Advisory Group (1992) on Folic Acid and the Prevention of Neural Tube
Defects. London: Department of Health; Scottish Office Home and Health Department; Welsh
Office: Department of Health and Social Services, Northern Ireland, 1992
196 Kadir RA, Sabin C, Whitlow B et al. Neural tube defects and periconceptional folic acid in
England and Wales: retrospective study. Br Med J 1999:319:92-3
197 Abramsky L, Botting B, Chapple J, Stone D. Has advice on periconceptional folate
supplementation reduced neural-tube defects? Lancet 1999;354:998-9
198 Alberman E, Noble JM. Commentary: food should be fortified with folic acid. Br Med J
1999;319:93
199 Meyer RE, Oakley GP. Folic acid fortification: initial effects on neural tube defect prevalence.
(submitted), 1999. Cited with the permission of the authors
200 Lawrence JM, Petitti DB, Watkins M et al. Trends in serum folate after food fortification. Lancet
1999;354:915-6
201 Jacques PF, Selhub J, Bostom AG et al. The effect of folic acid fortification on plasma folate
and total homocysteine concentrations. N Engl J Med 1999;340:1449-54
202 Oakley GP. Prevention of neural-tube defects. N Engl J Med 1999;341:1546
Folate, Folic Acid, and Health
69