ra drugs & toxicities
advertisement

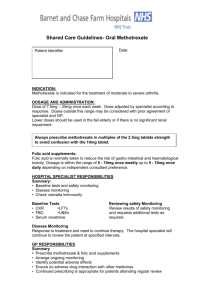
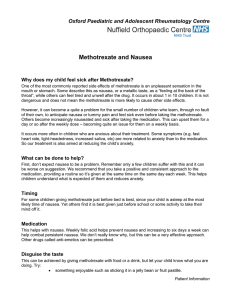
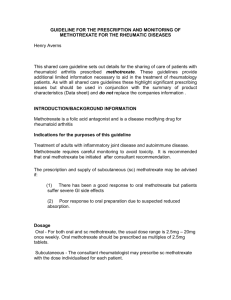
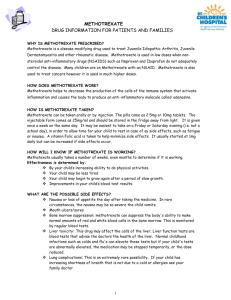
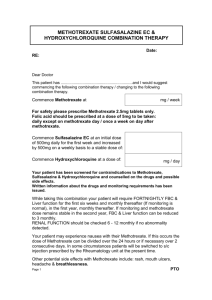
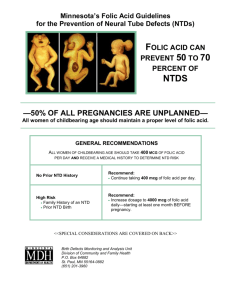
RA DRUGS & TOXICITIES: MILD RA 1) SULFASALAZINE Anti-inflammatory and Antibiotic (acetylsalicylic acid and sulfapyridine) Cleaved in the colon by bacterial enzymes to release acetylsalicylic acid and sulfapyridine ADVERSE Inhibits absorption of folate folate deficiency mild gastrointestinal disturbances (nausea, vomiting, loss of appetite, diarrhoea) skin rash and pruritus Headache, dizziness or depression oligospermia with impaired motility leucopenia, bone marrow depression haemolytic anaemia (G6PD) abnormal liver function tests, hepatitis and abdominal pain 2) HYDROXYCHLOROQUINE Nausea, dizziness, rash (must cease) MAIN RISK: RETINAL TOXICITY Haemolysis in G6PD Routine bloods not required (can do FBE after 1 week to check for haemolysis) Baseline then yearly Ophthalmology r/v MILD-MOD RA: 1) METHOTREXATE MUST CO-ADMINISTER FOLIC ACID – different day of week Folic acid analogue, binds to DHF-reductase and antagonises folic acid. Folic acid = essential for DNA synthesis Methotrexate impairs cell division. It is cytotoxic at high doses. Very long half-life, for noncancer indications, is given on one day per week. ADVERSE: Nausea and mouth ulcers Hepatotoxicity: fibrosis of increasing severity, culminating in cirrhosis Leucopenia, thrombocytopenia and anaemia Rash, menorrhagia, pneumonitis, fatigue, alopecia and depression TERATOGENIC (cease 3 months before conception) Dose in CRF, CI in severe RF Interactions Other drugs that inhibit folic acid synthesis BM depression trimethoprim+sulfamethoxazole (cotrimoxazole), OR Trimethoprim alone Levels with renal-affecting drugs (eg NSAIDS, Probenecid, Penicillin) BUT: At the doses used in rheumatology there is no clinically significant interaction with NSAIDs, and many patients are successfully managed on this combination MONITORING: FBE, U&E, LFT’s Monthly for 1st 6 months, then 1-2 monthly Abnormal LFT’s biopsy OTHER USES: PSORIASIS CROHN’S SEVERE RA: ALL 3 TOGETHER! More effective, and not more toxic, than methotrexate alone, or combinations of any 2 drugs. OR ADD: LEFLUNOMIDE In combination with Methotrexate: increased risk of leucopenia, pneumonitis and abnormal liver function CYCLOSPORIN With methotrexate: combination is more effective than either therapy alone, with adverse effects similar to that of either drug alone Inhibits cytokine release from activated T cells Adverse: MAIN ONES: Reversible renal impairment and hypertension (Co-administration with fish oil can reduce the nephrotoxicity and hypertension) Other: hirsutism, gingival hyperplasia, gastrointestinal disturbances, pancreatitis, weight gain, oedema, hepatic dysfunction, hyperlipidaemia, anaemia and other haematological abnormalities, central nervous system disturbances (eg tremor, fatigue, headache), and a burning sensation in the hands and feet. Hyperkalaemia, hypomagnesaemia and hyperuricaemia can occur. An increased rate of malignancies and infections has been reported BIOLOGICAL DMARDS (bDMARD) = Ab’s or cytokine receptors: ETANERCEPT: soluble TNF receptor (once/twice weekly SC injection) NB: vulnerability of patients taking biological DMARDs, or other significant immunosuppressants, to infectious diseases such as atypical pneumonia, listeriosis, and tuberculosis. Patients should be asked to report unusual symptoms, including fever or persistent cough