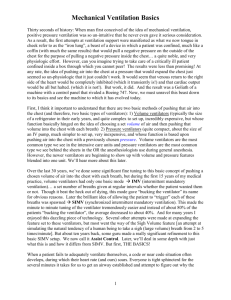
ventilator basics
advertisement
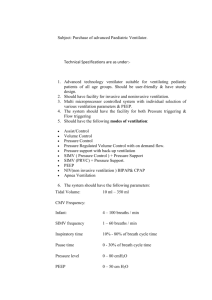
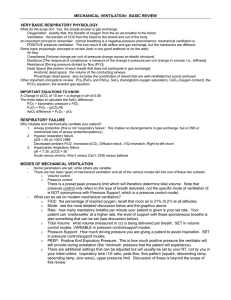
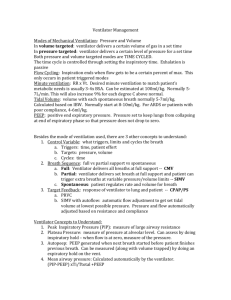
Ventilators – a basic tutorial What is the point? To provide oxygenation and ventilation. Or to reduce work of breathing. How do you ventilate someone? Put air in their lungs, either a set volume or set pressure. Vocabulary: 1. Tidal volume 2. Pressure support – pressure that augments a spontaneous breath 3. PEEP – positive end expiratory pressure. Pressure that is maintained at the end of expiration to prevent alveolar collapse. This in effect increases compliance, and thus oxygenation. 4. I:E ratio – the inspiratory time to expiratory time ratio. Normal is 3:1. 5. “10 over 5” or “10/5” – (pressure support) above (PEEP). The assigned pressure support, which is above and beyond the continuous PEEP, for spontaneous breaths. What can we control? 1. The amount of air we put into the lungs – either by volume (tidal volume) or pressure. We can also control pressure support and PEEP. 2. Oxygen – FiO2 3. Timing – Respiratory rate. I:E ratio. What can we measure? 1. Pressures a. Peak b. Plateau – a measure of how compliant the lung is c. Static = (Peak – Plateau). A measure of resistance in the circuit. 2. Minute Ventilation (total volume ventilated in 1 minute) Modes of ventilation – Each has distinct advantages and disadvantages. Volume-based ventilation: 1. Assist-Control. a. “assist” – refers to assisting a spontaneous breath b. “control” –refers to a fully controlled breath without spontaneous effort c. Result – There is a basal rate of full breaths, and each spontaneous breath gets a full volume. 2. IMV – intermittent mandatory ventilation a. “mandatory” – refers to assigned rate of full mandatory breaths b. All other breaths are spontaneous or assisted with pressure support c. “synchronized” – refers to synchronization of mandatory breaths with pt’s diaphragm Pressure-based ventilation: 1. Pressure Control a. Assigned rate of full pressure breaths b. Volumes will vary. c. Flow rate will vary. 2. Pressure Support a. Augments spontaneous breathing. Helps overcome tubing. 3. PRVC – pressure regulated volume control a. Adjusts I:E time and other factors to accomplish a rate with volume minimums and pressure maximums. Noninvasive ventilation: 1. CPAP – continuous positive airway pressure a. Tight fitting mask, only temporary, can’t eat b. Stents open alveoli with continuous pressure. No rate, no volume. 2. BiPAP – bidirectional positive airway pressure a. Tight fitting mask, only temporary, can’t eat b. IPAP – inspiratory positive airway pressure c. EPAP – expiratory positive airway pressure d. Can set rate (not that helpful) e. In BiPAP “10/5”, the IPAP is 10, the EPAP is 5. In SIMV “10/5”, the IPAP is 15, the EPAP is 5. Some troubleshooting and management issues: 1. AutoPEEP – PEEP that results because of incomplete exhalation of air. 2. The BEEPING/Angry ventilator – often due to increased peak pressures. If you see this, a. Check end expiratory pressure – to see if this is autopeep. b. Check end inspiratory pressure – this is your plateau pressure (ie compliance). c. Check static pressure – this is your resistance. If elevated, think obstruction in the circuit and check CXR, ETT placement, suction, etc. 3. Always see the effect of vent change in real time, and reevaluate pt after 30 minutes on a vent change. 4. ARDS – Acute respiratory distress syndrome a. Criteria i. Bilateral infiltrates ii. Acute onset <48’ iii. P:F ratio < 200 iv. No L atrial HTN b. Pathophysiology – injury and inflammation to lung > PMNs > alveolar wall injury > exudates > hyaline membranes and fluid > collagen > fibrosis. The result is decreased compliance and increased resistance, and decreased diffusing capacity for O2. c. Normal tidal volumes are 10-15 mL/kg of IBW d. ARDS tidal volumes should be 6 mL/kg of IBW, which improves outcomes. Goal plateau P should be <30-35. Causes permissive hypercapnea. Use PEEP and other maneuvers to recruit and maintain alveoli. 5. Remember the MICU vent order set. Cases: 1. 60yoM with 50 pack year of tobacco and COPD, presents with increased dry cough and respiratory difficulty x 2 days. He is mentating well, but is tachypneic and has increased work of breathing. 37.0, 100, 24, 110/70, 86% on RA. ABG 7.25/70/50 What medical treatment does he need? What respiratory support does he need? 2. 22yoM college student presents with fever and AMS. He has purpura everywhere and looks extremely toxic. 40.1, 145, 30, 75/40, 90% on RA. ABG 7.10/30/60, lactate 7.0, hgb 12. He gets 6L of NS but is still in shock. Is started on pressors. He can communicate but is confused. He is intubated with the plan to provide mechanical ventilation. Why? What is a reasonable ventilation strategy? 2 days later the patient develops bilateral pulmonary infiltrates. Ventilated FiO2 is 70%. What ventilator adjustment do you make?