D_0519_Gestational_Diabetes_Mellitus
advertisement
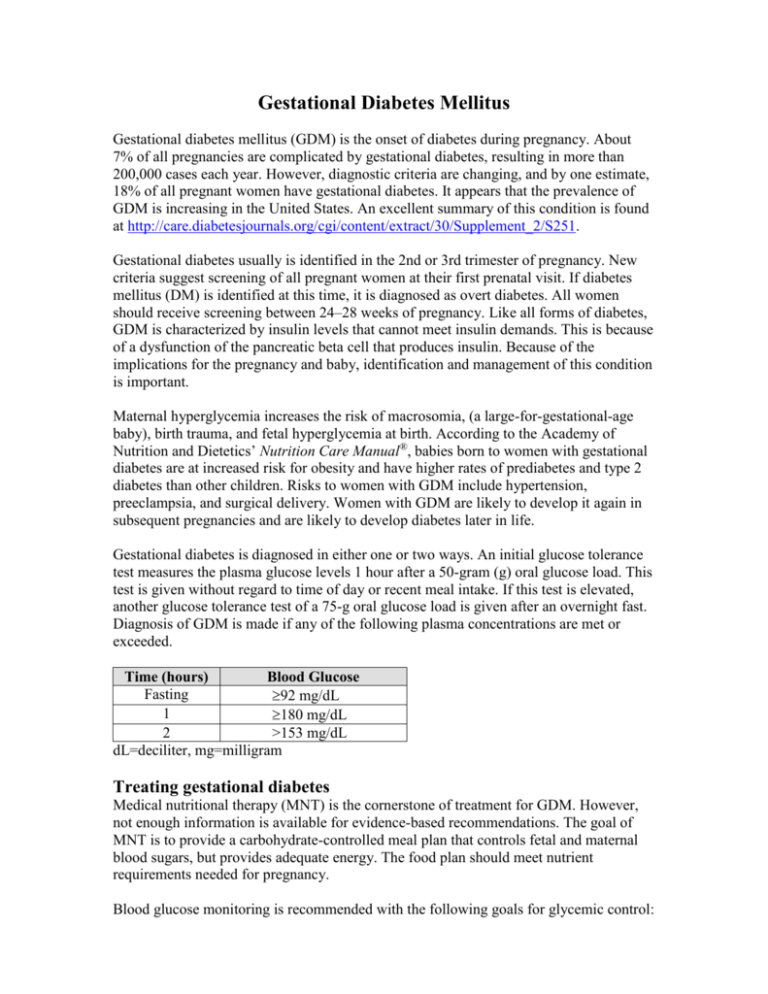
Gestational Diabetes Mellitus Gestational diabetes mellitus (GDM) is the onset of diabetes during pregnancy. About 7% of all pregnancies are complicated by gestational diabetes, resulting in more than 200,000 cases each year. However, diagnostic criteria are changing, and by one estimate, 18% of all pregnant women have gestational diabetes. It appears that the prevalence of GDM is increasing in the United States. An excellent summary of this condition is found at http://care.diabetesjournals.org/cgi/content/extract/30/Supplement_2/S251. Gestational diabetes usually is identified in the 2nd or 3rd trimester of pregnancy. New criteria suggest screening of all pregnant women at their first prenatal visit. If diabetes mellitus (DM) is identified at this time, it is diagnosed as overt diabetes. All women should receive screening between 24–28 weeks of pregnancy. Like all forms of diabetes, GDM is characterized by insulin levels that cannot meet insulin demands. This is because of a dysfunction of the pancreatic beta cell that produces insulin. Because of the implications for the pregnancy and baby, identification and management of this condition is important. Maternal hyperglycemia increases the risk of macrosomia, (a large-for-gestational-age baby), birth trauma, and fetal hyperglycemia at birth. According to the Academy of Nutrition and Dietetics’ Nutrition Care Manual®, babies born to women with gestational diabetes are at increased risk for obesity and have higher rates of prediabetes and type 2 diabetes than other children. Risks to women with GDM include hypertension, preeclampsia, and surgical delivery. Women with GDM are likely to develop it again in subsequent pregnancies and are likely to develop diabetes later in life. Gestational diabetes is diagnosed in either one or two ways. An initial glucose tolerance test measures the plasma glucose levels 1 hour after a 50-gram (g) oral glucose load. This test is given without regard to time of day or recent meal intake. If this test is elevated, another glucose tolerance test of a 75-g oral glucose load is given after an overnight fast. Diagnosis of GDM is made if any of the following plasma concentrations are met or exceeded. Time (hours) Blood Glucose Fasting 92 mg/dL 1 180 mg/dL 2 >153 mg/dL dL=deciliter, mg=milligram Treating gestational diabetes Medical nutritional therapy (MNT) is the cornerstone of treatment for GDM. However, not enough information is available for evidence-based recommendations. The goal of MNT is to provide a carbohydrate-controlled meal plan that controls fetal and maternal blood sugars, but provides adequate energy. The food plan should meet nutrient requirements needed for pregnancy. Blood glucose monitoring is recommended with the following goals for glycemic control: Premeal: ≤95 mg/dL 1-hour postmeal: ≤140 mg/dL 2-hour postmeal: ≤120 mg/dL MNT should consider lifestyle, food likes and dislikes, and culture of patients. A minimum of 175 g of carbohydrate/day (the recommended daily allowance [RDA] for pregnancy to allow for maternal and fetal growth and development) is recommended, broken down into three small to moderate meals and two to four snacks. An evening snack sometimes is needed to prevent ketoacidosis overnight. Patients should limit their intake of foods that are high in total carbohydrate and low in nutrients, such as soft drinks and other sweetened beverages, candies, etc. However, if blood sugar levels are maintained, patients can include these foods as part of their meal plan. Non-nutritive sweeteners generally are considered safe during pregnancy. As per the RDA for protein during pregnancy, 1.1 g/kilogram (kg) body weight/day is recommended. The remaining calories in the diet will come from fat, which is sometimes higher than normal because of increased protein intake. No agreement exists on the minimum calorie requirements for women with GDM. Patients should not have energy restrictions during pregnancy, because this can result in ketonemia and ketonuria, and cause damage to the fetus. Weight loss is not recommended during pregnancy. For overweight and obese women with GDM, modest energy and carbohydrate restriction sometimes is appropriate to prevent excessive weight gain. No data exist on optimal weight gain during pregnancy for women with GDM. Regular exercise is shown to lower fasting and postprandial blood-glucose levels, and is recommended during pregnancy for patients with GDM. Dietetics practitioners should recommend exercise during pregnancy only with the knowledge and consent of the patient’s physician. If optimal blood glucose levels are not maintained with medical nutrition therapy, pharmacological therapy (insulin and glyburide) is recommended. Implications for dietetics practitioners Management of GDM is individualized, based on patient weight, blood glucose levels, and activity level. Prescribe at least 175 g of carbohydrate/day, broken down into several meals and snacks daily. Provide adequate calories to maximize fetal growth and development, and to prevent ketoacidosis. Recommend regular blood glucose monitoring to evaluate lifestyle modifications and determine if insulin therapy is needed. References and recommended readings American Diabetes Association®. Gestational diabetes. Available at: http://www.diabetes.org/diabetes-basics/gestational/?loc=DropDownDB-gestational. Accessed June 12, 2012. American Diabetes Association, Bantle JP, Wylie-Rosett J, et al. Nutrition recommendations and intervention for diabetes: a position statement of the American Diabetes Association. Diabetes Care [serial online]. 2008;31(suppl 1):S61-S78. Available at: http://care.diabetesjournals.org/cgi/reprint/31/Supplement_1/S61. Accessed June 12, 2012. Academy of Nutrition and Dietetics. Nutrition Care Manual®. Available to subscribers at: www.nutritioncaremanual.org. Accessed June 12, 2012. Metzger BE, Buchanan TA, Coustan DR, et al. Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care [serial online]. 2007;30(suppl 2):S251-S260. Available at: http://care.diabetesjournals.org/cgi/content/extract/30/Supplement_2/S251. Accessed June 12, 2012. Review Date 6/12 D-0519