PRE-CONCEPTION ADVICE FOR
TYPE 2 DIABETES
Why Bother?
If conception HbA1c is >10% the congenital
malformation rate is 10%
If the conception HbA1c is <7% the congenital
malformation rate is that of the population.
Abnormalities
Cardiac malformation (4x)
Neural tube defects (5x)
Caudal regression (252x)
Duodenal/anal atresia (4x)
Renal anomalies (5X)
Situs invertus (84x)
CEMACH factors around poor
outcomes
Maternal social deprivation
No contraception in preceeding year
No folic acid in preceeding year
Poor pre-conceptive care
Poor glycaemic control before/during
pregnancy
Pre-existing complications
Pre-conception care
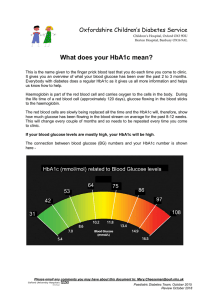
• Aim for pre-conception HbA1c <7% (NICE
•
•
•
•
•
•
state <6.1%)
Stop teratogenic medications (esp ACE1)
Lifestyle advice – smoking, alcohol, diet,
exercise
Start folic acid 5mg
Complications may deteriorate
Schedule of events
Who to contact immediately when pregnant
Glycaemic control pre-pregnancy
• Continue Metformin
• Stop ALL other oral anti-diabetic agents
•
•
•
•
•
including injectables (Exenatide, Liraglutide)
Start insulin if necessary
Background – Isophane vs Lantus/Levemir
Short acting analogues Novorapid &
Humalog are safe
Blood glucose monitoring
Ketone testing strips
Contraception
• All methods are acceptable
• Women for whom pregnancy would be
dangerous need a method with low failure
rate
• OCP – may cause transient change in
diabetes control
• Combined OCP – hypertension may cause
acceleration of nephropathy & retinopathy
• Monitor closely or avoid if complications
already present
Metabolic changes
Increased glucose to foetus
- pre meal hypoglycaemia
- increased starvation & ketosis
Insulin resistance (to increase available
nutrients to foetus)
- post meal glucose peaks
Foetal hyperinsulinaemia & macrosomia
Glycaemic targets
Organogenesis to week 12
Risk of severe hypo’s up to 14 weeks as lowest
period of insulin requirement (12 – 14 weeks)
Weeks 14 – 28 most crucial time for
preventing macrosomia etc
Third trimester – increased requirements
Glycaemic targets continued
Fasting level 3.5 – 5.9 mmols/l (NICE)
2 hours post meal <7.0 mmols/l
HbA1c unreliable – high rate cell turnover
Post delivery
Mostly delivered 38 to 39 weeks
Hypo’s common in third trimester
T2D – return to pre-pregnancy therapy unless
breast feeding (Metformin safe)
If breast feeding – reduce insulin dose by
approx. 30%
Contraceptive advice
Gestational Diabetes
Any degree of glucose intolerance with an
onset or first recognition in pregnancy – WHO
definition 1998
Fasting glucose >6mmol/l
2 hour glucose>7.8mmol/l (75G OGTT)
Marker of maternal risk of type 2 diabetes
Long term implications for the baby
Screening for GDM
Previous GDM
Persistent glycosuria
Previous large babies (>4kg)
Current large baby (>95th centile)
Polyhydramnios
First degree relative with diabetes
PCOS
Previous unexplained stillbirth
BMI >35
Ethnicity (Asian, Afrocaribbean)
Screening for GDM
When? – when risk factor identified and again
at 28 weeks
How? – 75G OGTT
Interpretation – positive if:
EITHER fasting >6.9mmol/l or
2hour >7.8mmol/l
Management
Pre-meal <5.5mmol/l
2 hour < 7.0mmol/l until 35 weeks then
<8.0mmol/l
Use diet, then Metformin, then insulin if
necessary
Ongoing management
6 week repeat OGTT to exclude ongoing DM
or IGT
NICE – fasting glucose at 6 weeks and then
annually
2 – 3% still have diabetes
31% have pre-diabetes
Remember: Type 2 diabetes has same risks as type1
Pre-pregnancy counselling reduces risks (RR
0.4)
Tight glucose control improves outcomes –
refer immediately
Keep on Metformin, all other anti diabetic
meds stop. Insulin as necessary
GDM have high risk of future diabetes
Thank you to Dr Julia Platts at Llandough
Hospital for the use of her information from a
previous lecture.