ESP_MINUTES_NOVEMBER_2010
advertisement
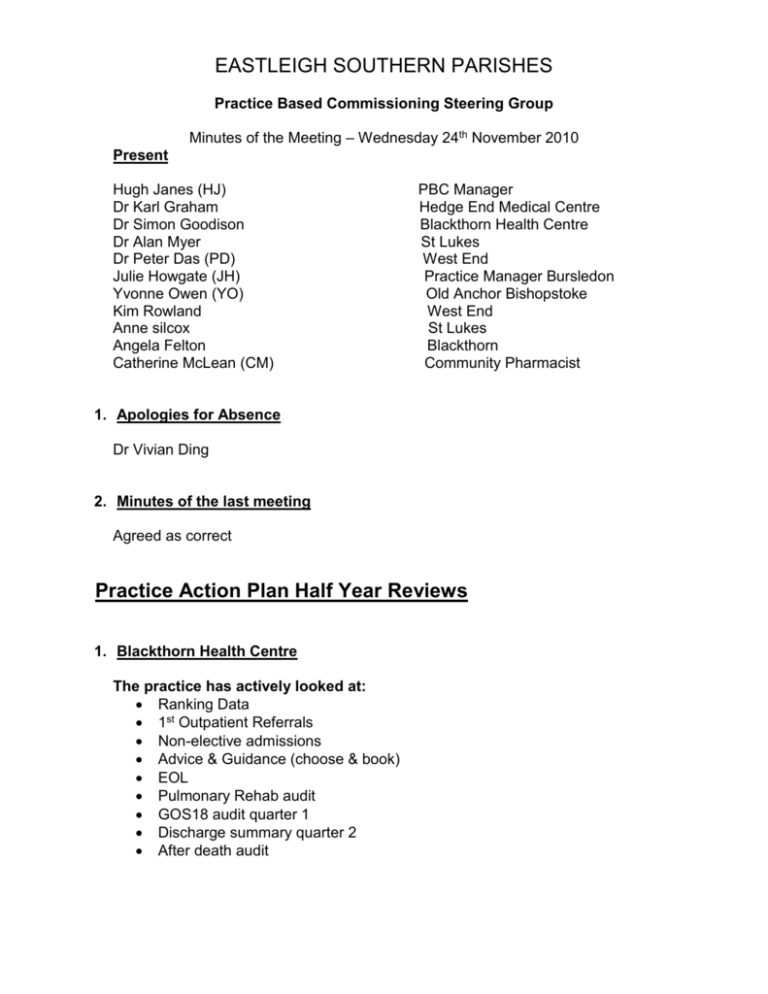
EASTLEIGH SOUTHERN PARISHES Practice Based Commissioning Steering Group Minutes of the Meeting – Wednesday 24th November 2010 Present Hugh Janes (HJ) Dr Karl Graham Dr Simon Goodison Dr Alan Myer Dr Peter Das (PD) Julie Howgate (JH) Yvonne Owen (YO) Kim Rowland Anne silcox Angela Felton Catherine McLean (CM) PBC Manager Hedge End Medical Centre Blackthorn Health Centre St Lukes West End Practice Manager Bursledon Old Anchor Bishopstoke West End St Lukes Blackthorn Community Pharmacist 1. Apologies for Absence Dr Vivian Ding 2. Minutes of the last meeting Agreed as correct Practice Action Plan Half Year Reviews 1. Blackthorn Health Centre The practice has actively looked at: Ranking Data 1st Outpatient Referrals Non-elective admissions Advice & Guidance (choose & book) EOL Pulmonary Rehab audit GOS18 audit quarter 1 Discharge summary quarter 2 After death audit Findings Ranking data was fairly static There has been a significant rise in ophthalmology, gynae and general surgery referral Differences in referrals to ENT and Orthopaedics were identified between GP’s 50% of Ophthalmology referrals were generated from GOS18. Referrals have now been split between GOS18 and direct referrals and this process will continue to be reviewed monthly There were no alternative pathways identified for Ophthalmology or Cardiology. All GP’s regularly used the MAP of medicine toolkit which has been installed on every ones desktop It was felt that by using Advice and Guidance for Gynaeology and Neurology would not only reduce referrals but also admissions GP acute admissions were considered appropriate with no alternative pathway Antibiotic prescribing over the telephone for incorrect diagnosis may have led to the condition worsening which in turn may have led to admission Introduction of rescue medicines and antibiotics by the respiratory home care team may have reduced acute admissions 7 out of the 28 patients reviewed over the age of 65 yrs for non-elective admissions may have been prevented with enhanced nursing care in the community, rapid medical assessment step up beds and enhanced discharge planning Increased support over the weekend could have prevented those patients where were admitted over that weekend but who had been in contact with the GP on the Friday Antibiotic ciprofloxacin used in MRSA patient thought to have precipitated MRSA sepsis. The practice is planning to invite a microbiologist to come in to talk to the GP’s re antibiotic prescribing Epistaxis admission may have been prevented by the practice cauterisation or application of topical antibiotic Falls – if step-up beds were available for rehab admissions may have been prevented Elderly care/mental health liaison might have prevented admission of patients with UTI/Dementia Learning points Trial of PPI for chronic cough patients prior to referral to ENT Cervical polyps could be removed in the practice Rescue antibiotics and steroids for acute exacerbation of COPD could prevent admission Avoid the use of ciprofloxacin in MRSA patients Consider support and added needs of patients over the weekend GP’s to use Map of Medicine toolkit when uncertain on referral pathway Use of emergency HOOF oxygen and increased support over weekends could reduce the possibility of admission Alternative Pathways Identified GOS18 triage Direct referral to gynecology would be useful Minor op clinic in the community for hernias and lipomas More use of respiratory home care team Rapid elderly care medical assessment Enhanced nursing in the community and discharge planning Step up beds Nasal cauterisation for expistaxis could be performed in the practice Wax removal for patient with previous perforation in the community Adolescent audiology Orthopaedic Choice – improved community physio is necessary as poor provision leads to earlier referral or Orthopaedic Choice What has been useful Meetings to discuss referrals an admissions had be educational Discussion about admissions of patients who had been seen in the previous week Non elective admissions of patients aged over 65 Using the Map of Medicine too What has been less useful Ranking data Discussing all patients GP’s making own decisions on appropriateness of their referrals which has not been challenging enough Future Plans GP’s will review each other’s referrals to Dermatology GP’s will discuss each referral with another GP if they feel there may be an alternative pathway 2 St Lukes Surgery The practice has actively looked at Referral data Practice Ranking data Use of PBC tool EOL Pulmonary Rehab audit GOS18 audit quarter 1 Discharge summary quarter 2 After death audit Findings Ranking data was fairly consistent with the activity across the PCT locality Numbers have increased for elective admissions Reduction in A&E attendances Outpatient 1st referrals are high and the practice are considering how this can be improved Highest 3 areas are Orthopaedics, ENT and dermatology There have been problems within the practice with inappropriate referrals from locum GP’s The practice has been going through a very difficult time in the last 9 months with a lot of changes Not all GP’s are using the Teledermatology pilot Learning Points Over use of locums to meet current shortfalls has been leading to unnecessary referrals Teledermatology Pilot needs to be encouraged with all GP’s Poor Physiotherapy waiting times and direct access to podiatry is a likely reason why Orthopaedic choice referrals have increased The practice needs to dedicate a regular weekly meeting to PBC and look at getting specialist in for educational meetings The practice needs to organise monthly referral meetings and peer reviews Alternative Pathways Identified Direct access to podiatry Quicker Physiotherapy appointments What has been useful Looking at referral data Identifying inappropriate Locum referrals 3 West End Surgery The practice has actively looked at Referral review Teledermatology EOL Pulmonary Rehab audit GOS18 audit quarter 1 Discharge summary quarter 2 After death audit Findings Referrals recorded weekly and discussed quarterly All COPD patients have been referred to the rehabilitation pilot scheme Successful use of Teledermatology Learning Points Dr Peter Das acknowledge that there has been a lack of direction within the practice and they required more help from the locality Referrals have been modified appropriately after discussion within the practice Continue to refer to Pulmonary Rehab Continue to use Teledermatology High A&E attendances were identified and it was agreed to come up with some form of education/help pack for patients Alternative Pathways Identified GOS18 referral triaged 4 Hedge End Surgery The practice has actively looked at Ranking Activity 1ST Patient referrals Weekly referral data Using PBC tool EOL Pulmonary Rehab audit GOS18 audit quarter 1 Discharge summary quarter 2 After death audit Choose & Book advice and guidance Findings Not all referrals had been initiated by the practice A large number of referrals were consultant to consultant Follow up appointments were charged as 1ST outpatient appointments Learning Points Using Choose & Book guidance could reduce the number of referrals Reduce referrals for was impaction by using a difference pathway Invite an ENT consultant for educational meetings Alternative Pathways Identified Nasal Scoping could be done in practice ENT wax impaction could be done in the community Punch biopsy could be carried out in the practice Acne – initiation specialist prescribing within the locality What has been useful Identifying new pathways Looking at referral data What has been less useful The biggest problem the practice has is time for the practice to keep meeting on a regular basis to discuss referrals and new care pathways 5 Old Anchor Surgery The practice has actively looked at 1st Out patient referrals Ranking data EOL Pulmonary Rehab audit GOS18 audit quarter 1 Discharge summary quarter 2 After death audit Medicines management Findings Some referrals were not perceived to benefit the patient Patients declined surgery when offered Dermatology referrals could have been dealt with in a community setting Patient pressure indicated inappropriate referrals More education and discussion was needed when explaining a referral or surgery to the patient The surgery has recently been without a partner and they have been using locum GP’s which has resulted in higher referral rates and possibly inappropriate referrals Improved care for COPD patients through the pulmonary rehab service Patients have poor inhaler technique No access to nebuliser loan and no community rapid response team Learning Points Difficulty in organising meetings due to problems within the practice Problems with locums making unnecessary referrals Alternative Pathways Identified Community Rapid response team ENT micro suction What has been useful What has been less useful Biggest problem for the practice is that they have not got a regular partner and are using locum GP’s 6 Bursledon Surgery The practice has actively looked at Findings Learning Points Alternative Pathways Identified What has been useful What has been less useful Future Plans Actions Agreed for the next meeting A & E Admission’s avoidance audit Identify 10 patients over 65 yr of age who have over a period of 1 month (any month) Been admitted to either A&E or Eye casualty 1 day plus Who initiated the attendance Was there an alternative pathway Agreed Topics we would work on as a locality DVT avoidance – look at referrals ENT Gynaecology Cardiology BNP – Echo Referrals for Heart Failure Date of next meeting Steering Group Wednesday 15th December 2010