Lecture 2 - Diseases of the Ear
advertisement
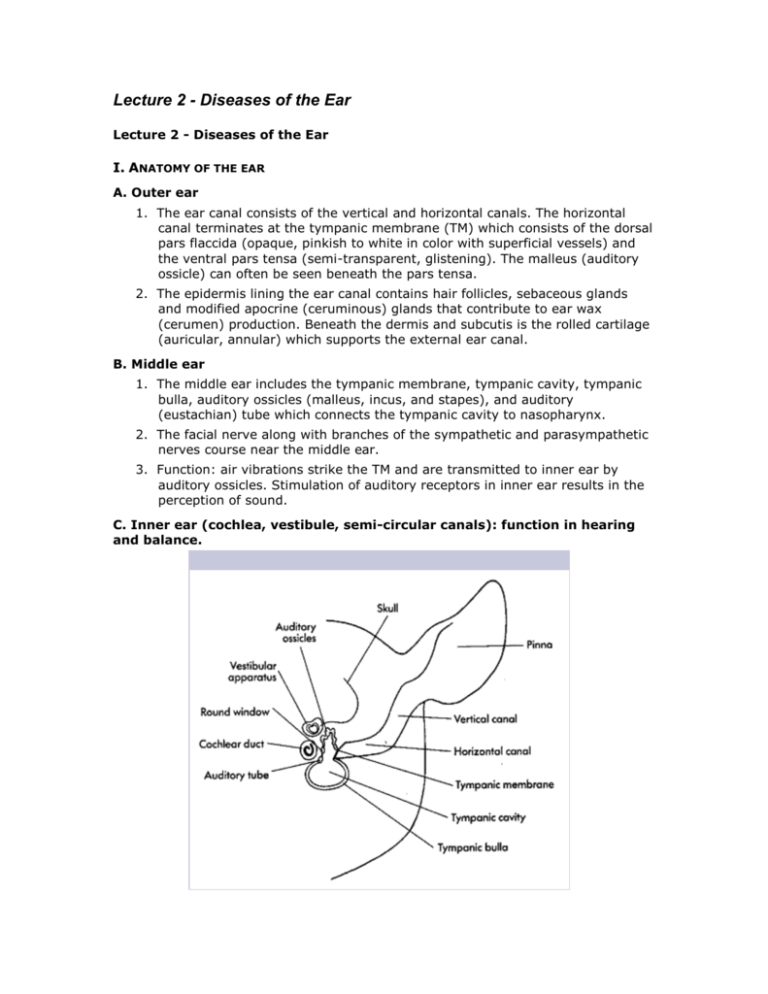
Lecture 2 - Diseases of the Ear Lecture 2 - Diseases of the Ear I. ANATOMY OF THE EAR A. Outer ear 1. The ear canal consists of the vertical and horizontal canals. The horizontal canal terminates at the tympanic membrane (TM) which consists of the dorsal pars flaccida (opaque, pinkish to white in color with superficial vessels) and the ventral pars tensa (semi-transparent, glistening). The malleus (auditory ossicle) can often be seen beneath the pars tensa. 2. The epidermis lining the ear canal contains hair follicles, sebaceous glands and modified apocrine (ceruminous) glands that contribute to ear wax (cerumen) production. Beneath the dermis and subcutis is the rolled cartilage (auricular, annular) which supports the external ear canal. B. Middle ear 1. The middle ear includes the tympanic membrane, tympanic cavity, tympanic bulla, auditory ossicles (malleus, incus, and stapes), and auditory (eustachian) tube which connects the tympanic cavity to nasopharynx. 2. The facial nerve along with branches of the sympathetic and parasympathetic nerves course near the middle ear. 3. Function: air vibrations strike the TM and are transmitted to inner ear by auditory ossicles. Stimulation of auditory receptors in inner ear results in the perception of sound. C. Inner ear (cochlea, vestibule, semi-circular canals): function in hearing and balance. From: Current Veterinary Dermatology: Griffin, Kwochka, MacDonald Mosby 1993 OTITIS EXTERNA II. General considerations A. Incidence: otitis externa is common Otitis externa occurs in about 15 - 20% of canine and 4 - 7% of feline cases presented. The lower incidence in the cat is likely due to anatomical factors (more erect ear, less hair, and shorter vertical canal). B. Pathophysiology 1. Chronic inflammation results in hyperplasia of epidermis and apocrine glands, dermal edema, and fibrosis. These changes cause swelling and stenosis of the ear canal. 2. Long-standing chronic irritation can result in mineralization and subsequent ossification of the annular and auricular cartilages (rock hard on palpation). III. ETIOLOGY A. Multifactorial disease process: predisposing, primary and perpetuating factors Predisposing factors change the microclimate in the ear and increase the risk of disease, primary factors directly induce disease, and perpetuating factors tend to complicate otitis and prevent resolution. 1. Predisposing factors: conformation of ear (droopy ears, etc.), excessive moisture or hair in ear, treatment with irritating topical agents, tumors, polyps, and underlying systemic disease. 2. Primary causes: parasites, dermatophytes, atopy, food allergy, contact allergy, primary seborrhea, autoimmune disease, foreign bodies, glandular hyperplasia, 3. Perpetuating factors: underlying otitis media, ear pathology (hyperplasia, edema, fibrosis), bacteria, and yeast. B. What's most common? 1. Cats frequently suffer otitis externa due to Otodectes cynotis and dogs often due to underlying atopy, food allergy, or keratinization disorders. 2. Obtain a good history, examine the animal carefully and perform basic diagnostic tests to identify likely predisposing, primary, and perpetuating factors. IV. DIAGNOSIS A. History Head shaking, aural pruritis, otic discharge, and malodor are common. Aural hematomas may occasionally develop secondary to self-trauma/head shaking. B. Physical exam 1. General exam: look for underlying diseases that predispose to otitis *Q: What clues on physical exam are suggestive of underlying atopy? Food allergy? Hypothyroidism? Keratinization defects? Demodex? 2. Appearance of otic discharge: may provide clues A "coffee-grounds" appearance is suggestive of ear mites, a moist brown exudate suggests yeast or Staph, oil yellow to tan discharge suggests ceruminous otitis, and a purulent cream-yellow discharge suggests gram negative bacteria. C. Examination of the ear 1. Appearance of ear canal a. The normal ear canal is pale to light pink in color and slightly moist with cerumen. Some animals may have hairs in the vertical ear canal. b. The ear canal becomes erythematous, swollen, and narrowed with acute otitis. As inflammation continues, increased sebaceous gland secretions, hyperplasia of the epidermis, and dermal edema occur. Edema causes constriction of the canal lumen and pain from entrapment of nerves against the cartilage. c. With chronicity, proliferation of connective tissue in the dermis and subcutis gives rise to fibrosis and additional thickening of skin. Further occlusion of the ear canal occurs ("cauliflower ear") and ossification of auditory cartilage may occur. 2. Otoscopic exam a. Use aseptic cones soaked in cold sterile solution (rinse prior to use). Examination of the inflamed ear is uncomfortable and painful - don't hesitate to use adequate sedation or general anesthesia. It may be necessary to treat firstto help alleviate swelling and pain and facilitate adequate otoscopic exam. b. Tympanic membrane (TM): may be difficult to visualize (one study showed that a satisfactory view of the tympanic membrane in patients with chronic otitis was only obtained in 28% of patients). Chronic otitis externa inevitably gives rise to otitis media (see later). D. Diagnostic evaluation 1. Samples of otic discharge Obtain specimens from horizontal ear canal (place Q-tip through guarded lumen of otoscope cone). Harvest samples from both ears. a. Cytology: roll a small amount of discharge on glass slide, heat fix, and stain (Diff-Quik). Evaluate for microorganisms (bacteria, yeast) and inflammatory cells. *Q: Do dogs normally have microorganisms in their ears? Yes, small numbers of yeast (Malassezia pachydermatis) and gram positive cocci (Staph, Strep) are normal. b. Oil smear: place small amount otic discharge on a slide and mix with oil to look for Otodectes cynotis. 2. Pursue additional diagnostic tests as indicated a. Unless underlying causes of otitis externa are addressed, treatment will only temporarily ameliorate clinical signs. b. Perform allergy testing, skin scrapings, DTM culture, endocrine testing, etc. as indicated i. Hypersensitivity (allergic) disease: is the most common cause of persistent bilateral otitis externa in the dog. Up to 55% of dogs with atopic dermatitis and 80% of dogs with food allergy have concurrent otitis externa (and some will have just unilateral signs). Otitis externa (pruritis or erythema of the ears) may be the ONLY sign in 5% of atopic dogs and 25% of food allergic dogs. ii. Keratinization defects and endocrinopathies: may see chronic ceruminous otitis externa. 3. Other diagnostic tests Culture/sensitivity is indicated in cases of chronic otitis externa and otitis media/interna to help guide systemic antibiotic therapy (see later). V. Treatment A. General guidelines 1. Clean the ears first - topical medications are often ineffective in the face of inflammatory exudate. 2. Sedation or general anesthesia is frequently required for exam and treatment of an inflamed and painful ear. Treatment prior (with glucocorticoids) helps alleviate inflammation and allows for a more effective otoscopic exam. 3. If the integrity of the tympanic membrane is compromised, ruptured, or unknown DO NOT use potentially ototoxic cleansing solutions or medications. B. Glucocorticoids (GC's) (see table) 1. Systemic GC's (prednisone, prednisolone) Indicated if inflammation, swelling, and stenosis of the ear canal are present. Treatment helps to "open" the ear canal and allow for more effective topical therapy. Dose: anti-inflammatory dose of oral prednisolone (0.5 - 1.5 mg/kg/day in the dog and 1 - 3 mg/kg/day in the cat) for 3 to 5 days. 2. Topical glucocorticoids: beneficial in most Decreases inflammation, pain, swelling, pruritis, exudation, and proliferative changes thus facilitating drainage and ventilation. Most topical otic preparations contain steroids (see table). C. Cleaning the ear 1. Remove excess hair. *Q: How would you do this? Clippers can be used to gently remove excess hair at entrance to external ear canal. Plucking hair from the vertical ear canal should only be performed if hairs are thought to be directly contributory to otitis. 2. Cleansing solutions (see table) a. Ceruminolytics: emulsify waxes and lipids so they can be flushed from ear - helpful if excessive waxy secretions are present. Some products are ototoxic (do not use with compromised TM). b. Cleansing agents: mechanically flush away otic debris. Some have antibacterial activity, anti-yeast activity, or drying effects. Many (such as chlorhexidine) are potentially ototoxic. Solutions safe to use in face of ruptured eardrum include sterile lukewarm 0.9% saline, DermaPet Ear/Skin Cleanser, and acetic acid preparation (white vinegar diluted 1:1 with water). c. Technique: BE VERY GENTLE as the TM is easily injured. *Q: What complications may result from poor technique? A: Ruptured eardrum, vestibular signs, Horner's and hearing loss. i. In awake animal, fill ear canal with cleansing solution, massage thoroughly, allow animal to shake head, and gently wipe away dislodged debris. ii. Anesthetized animal: gently infuse cleansing agent, massage ear canal, and then suction using red rubber catheter attached to 12 ml syringe while observing through otoscope cone. An ear loop is helpful for removing debris lodged near TM. The MedRx Video Vetscope allows for magnified exam, flushing, and suctioning under direct visualization. iii. At home: have owners fill ear canal completely, massage base of ears, let animal shake, and then wipe away loosened debris. Clean ears once daily for 7 to 10 days; follow with once to twice weekly maintenance cleaning. Monitor response to therapy with recheck exam and cytology. d. Drying agents: helpful in dogs susceptible to moist ears (swimmers, etc.). Apply weekly to help facilitate evaporation. VI. THERAPEUTICS FOR SPECIFIC DISEASES (SEE TABLE) A. Bacterial otitis 1. Common pathogens include Staph intermedius (most common), Pseudomonas aeruginosa, Proteus mirabilis, E. coli, Corynebacterium, and Streptococcus spp. Multiple organisms are often present in cases of chronic otitis. 2. Cleansers: purulent discharge will inactivate many antibiotics, so ears must be clean for effective therapy. Chlorhexidine, dilute povidone-iodine, or acetic acid based flushes work well. 3. Topical antibiotics: products containing neomycin and polymxyin B, are usually effective in uncomplicated cases while antibiotics with extended spectrum (fluroquinolones, aminoglycosides) are used for more severe or resistant cases. See otitis media (below) as well as table for listed antibiotics. 4. TrisEDTA: helpful in treatment of gram negative infections (such as Psuedomonas). Promotes an alkaline pH (8.0) and facilitates increased antibiotic efficacy. 5. Systemic antibiotics: indicated in cases of suppurative or chronic otitis, or otitis media (see below). B. Yeast otitis: usually due to Malassezia pachydermatis 1. Cleansers: acetic acid based solutions (DermaPet Ear/Skin Cleanser or white vinegar/water) may effectively address yeast overgrowth. 2. Topical anti-yeast preparations: include 2% miconazole, clotrimazole, and Tresaderm (containing thiabendazole). Baytril Otic (containing the antifungal ingredient silver sulfadiazine) may also be used. Thiabendazole and silver sulfadiazine are purportedly less efficacious. 3. Systemic agents: indicated in chronic refractory otitis externa or otitis media (see later). Malassezia pachydermatis Otodectes cynatis Diagrams from: Muller & Kirk's 5th edition. C. Otodectes cynotis: ear mites 1. Overview Ear mites are a common cause of otitis externa (50% of cases seen in the cat and 5 - 10% of cases in the dog). Mites feed on lymph and epidermal debris, inject mite antigen and induce host hypersensitivity reaction. As few as 2 - 3 mites can cause severe clinical signs. Mites may migrate to other areas of the haircoat (important to treat entire body) and are highly contagious (treat all in-contact dogs and cats). Treatment should continue for 4 weeks (to insure complete therapy as not all products are effective against incubating mite eggs). 2. *Topical otic preparations Topical preparations include: Tresaderm (active ingredient - Thiabendazole), Acarexx (active ingredient ivermectin), Milbemite (active ingredient milbemycin) (latter two are licensed for use in cats), Cerumite (active ingredient pyrethins), and Revolution (active ingredient selamectin). *Consult package inserts for dosing instructions. 3. Topical body treatments a. Revolution: treatment of choice. Safe, effective and labeled for treatment of ear mites. Dosing regimen (labeled instructions): apply once monthly for two treatments. b. Systemic ivermectin: alternative therapy, not a first-line treatment This drug is not labeled for this use. MUST test for heartworm disease first, do NOT use in Collie breed or any crosses thereof, and avoid use in animals < 4 months of age. Dosing regimen: 250 ug/kg SQ: repeat every 10 - 14 days for 2 to 3 treatments. D. Ticks 1. Otobius megnini: spinous ear tick Found in the southwest United States. Parasitic larvae and nymphs feed within ear causing a significant inflammatory reaction in the ear canal. Treatment = removal of ticks, tick control measures (see later) and management of secondary otic inflammation. 2. Other ticks (Dermacentor, Rhipicephalus sanguineus, etc): may also infest ear canal. Treatment involves symptomatic ear care, removal of ticks and control of ticks on the body as well as in environment. Potential treatment options include Preventic collar, Amitraz dips, Frontline, Advantix, and Revolution (*consult package inserts for dosing instructions). E. Other 1. Foreign bodies: remove and provide symptomatic ear care Heavy sedation to general anesthesia may be necessary for removal. Alligator forceps can be advanced through otoscope cone to aid in retrieval of foreign bodies (such as grass awns). 2. Neoplasia: typically unilateral a. Benign: nasopharyngeal polyps (cats). Usually arise from the mucosal lining of the middle ear, Eustachian tube, or pharynx. Nasopharyngeal polyps tend to extend through TM (causing signs of otitis) or into nasopharynx (causing respiratory signs). Etiology unknown, and most successfully managed via complete surgical excision (consult reference source). b. Malignant: ceruminous gland adenocarcinoma, squamous cell carcinoma, other. Ceruminous gland tumors are the most common ear canal tumor in both the dog and cat. OTITIS MEDIA/INTERNA A. Etiology 1. Otitis externa Otitis media usually results from chronic (> 45 - 60 days) otitis externa (infection spreads across the tympanic membrane). Otitis media is present in > 50% of dogs with chronic otitis externa. 2. Ascension via eustachian tube In the cat, otitis media may also result from upper respiratory tract disease, invasion of nasopharyngeal polyp across TM, or damage to the TM from ear mites. 3. Microbes Staph intermedius and Psuedomonas aeruginosa (as well as Strep, Proteus, Klebsiella and E.coli). are common isolates in the dog. Staph intermedius, Strep and Mycoplasma have been isolated in cats (as well as Psuedomonas and others). Yeast otitis media is usually due to Malassezia pachydermatis. B. Clinical signs 1. As for chronic otitis externa (otitis media is a major cause of recurrent otitis externa). 2. Tympanic membrane: may be normal or abnormal a. The TM may appear discolored, bulging, ruptured, absent, or normal. In one study, 70% of eardrums in dogs with documented otitis media were intact (eardrum can seal with infection trapped inside bullae). b. Mucoid exudate in bulla or horizontal ear canal: produced by lining of tympanic bulla and may be noted in horizontal ear canal when it leaks through ruptured TM. 3. Cranial nerve signs: may note Horner's (damage to sympathetic supply), facial nerve palsy (damage to facial nerve), or KCS (damage to parasympathetic nerve supply to lacrimal gland). 4. Hearing deficits: may result from fluid accumulation in middle ear, damage to auditory ossicles (osteomyelitis), or damage to the cochlear nerve. 5. Pain: may be noted on palpation of base of ear and some dogs may be reluctant to open mouth. 6. Drainage of exudate from middle ear (via Eustachian tube) may give rise pharyngeal signs. 7. Otitis interna: usually results from extension of otitis media May note signs of peripheral vestibular disease (head tilt, nystagmus, circling) due to damage of vestibulocochlear nerve. *Q: What type of nystagmus would you expect to find in these patients? C. Diagnostic evaluation 1. Preliminary workup as for otitis externa. 2. Cytology, culture/sensitivity from middle ear a. General anesthesia is usually necessary Prior treatment with systemic steroids (see above) may help facilitate a more complete otoscopic exam. A cuffed endotracheal tube should be placed to protect airway from drainage of secretions from middle ear. b. Obtain specimens for cytology and culture/sensitivity (C/S) Obtain samples from middle ear (tympanic bulla) for culture and sensitivity (C/S of horizontal canal may differ from C/S of bulla in up to 80% of cases). i. If eardrum is ruptured, gently advance sterile catheter (through lumen of sterile otoscope cone) into tympanic bulla to obtain diagnostic specimens. ii. If eardrum is intact, perform myringotomy (consult reference source) in region of pars tensa to obtain diagnostic specimens. 3. Bulla radiographs: look for soft tissue or bony changes Perform radiographs before taking diagnostic specimens or infusing fluids. Radiographic signs may not always be apparent in middle ear disease. CT and MRI are more sensitive than radiographs in the detection of disease. D. Treatment 1. General tenants of therapy as for otitis externa (see above and attached table) 2. Flush tympanic bulla If mucoid to purulent exudate is present within middle ear, you must flush bulla to effectively treat (medications often ineffective in presence of exudate). Flush with warmed non-ototoxic solution (such as sterile saline or dilute povidone-iodine). After flushing, infuse bulla with non-ototoxic aqueous topical medications (see below). May need to repeat treatment several times to effect resolution of disease. 3. Topical medications (or infusions): avoid any preparations that are potentially ototoxic a. Topical antibiotic infusions into bullae enables very high levels of local antibiotics to be attained at site of infection. Tris-EDTA may be helpful for bacterial infections (see above). b. Ototoxic preparations may result in hearing loss and vestibular signs. Agents safe to instill in the middle ear include aqueous dexamethasone sodium phosphate, ciprofloxacin, enrofloxacin, ofloxacin, aqueous penicillin G, ticarcillin, some cephalosporins (ceftazidime), and the antifungal agents clotrimazole, miconazole, and nystatin. Selection of appropriate agents should be based on C/S results. c. "Gemish" solutions: these homemade solutions are an alternate therapeutic option for topical therapy of bacterial or yeast otitis externa/media (but perform C/S if otitis media). They are not ototoxic (safe to use in the face of a ruptured eardrum). i. Bacterial Gemish: 12 mls DermaPet Ear/Skin Cleanser (+) 2 mls injectable Baytril (22.7 mgs/ml) (+) 6 mgs dexamethasone sodium phosphate. ii. Malassezia Gemish: 12 mls DermaPet Ear/Skin Cleanser (+) 6 mgs dexamethasone sodium phosphate. Directions: apply 0.5 to 1.0 mls (depending on size of patient) to affected ear twice daily for 14 days. 4. Systemic medications a. Oral glucocorticoids: prednisone, prednisolone (see above) help to alleviate inflammation (and hence open ear canal), as well as decrease mucus production from the mucoperiosteum of middle ear. b. Systemic antibiotics: select based on C/S results. Potential choices include the fluoroquinolones (useful for rods) and Clavamox as well as some cephalosporins (useful for cocci), and azithromycin (activity against Mycoplasma and Bordetella in the cat). Therapy should be continued for a minimum of 3 to 6 weeks and up to 6 months in some cases. Use high end of dose range due to poor penetration into ear. Systemic antifungals: oral ketonconazole or itraconazole are usually effective for Malasezia. 5. Surgery (see below) Cases unresponsive to medical therapy or those with severe proliferative tissue require surgery for successful management (total ear canal ablation with bulla osteotomy most successful). VII. HOME CARE AND RECHECKS A. Educate owner as to chronic nature of disease. Many animals with otitis externa require continued ear care at home due to persistence of predisposing factors (anatomy, moisture, underlying disease, etc.). Otitis externa is often a manageable but not curable disease. B. Demonstrate proper ear cleaning technique You must take the time to explain the anatomy of the ear and demonstrate proper cleaning technique so the owner understands. In some cases, intermittent use of a cleansing/drying agent will suffice, in other cases owners will need to utilize ceruminolytics and ear bulb flushes followed by instillation of medication. C. Advise owners to wipe away debris mobilized by ear cleaning with cotton balls. Q-tips should be avoided as they are abrasive to the lining of the ear canal and can drive debris further down. D. Perform frequent rechecks to assess response to therapy and owner compliance. VIII. SURGICAL TREATMENT A. Indications: chronic or severe cases of otitis. Surgery is indicated in management of otitis media/externa when chronic changes (fibrosis, ossification, stenosis of the ear canal), or patient uncooperation preclude effective medical management. B. Techniques 1. Lateral wall resection (Zepp): resection of lateral wall of ear canal. In one study, surgery resulted in elimination of clinical signs in only 23% of patients (as most often otic disease is not limited to vertical canal). Generally believed to be ineffective. 2. Vertical ear canal ablation: resection of entire vertical ear canal. Not effective if horizontal canal is diseased or if otitis media is present (and > 50% of patients with chronic otitis externa have otitis media). Does not allow for drainage of infected middle ear. 3. Total ear canal ablation (TECA) with bulla osteotomy: most likely to be effective. The total ear canal and lateral wall of the tympanic bulla is removed. Secretory tissue lining the bulla is removed by gentle curettage. This procedure typically results in hearing loss (although loud noises may still be appreciated via bone conduction). Goals of Lecture 2 - Diseases of the ear References (for all dermatology lectures): Muller & Kirk's Small Animal Dermatology 5th edition 1995. Kirk's Current Veterinary Therapy XII. Bonagura. W.B. Saunders Co. 1996. WB Saunders Co. Selected excerpts from ACVIM 1995 and 1996 proceedings, and JAVMA, JIVM, and Compendium 1992-2006. Small Animal Dermatology Secrets: Karen L. Campbell 2004. Skin Diseases of the Dog and Cat Richard Harvey, Patrick McKeever 2003. Small Animal Dermatology A Color Atlas and Therapeutic Guide Linda Medleau, Keith Hnilica 2001 and Small Animal Ear Diseases An Illustrated Guide 2nd edition. Gotthelf 2005. Supplemental information also provided courtesy of Dr. Danny Scott and Dr. Miller, Cornell University. 1. Be familiar with the basic anatomy of the ear (overview only) - what constitutes outer ear? middle ear? inner ear? What important nerves course near the region of the middle ear? (B.2.) 2. What happens to the ear in the patient that develops chronic otitis externa? (II. B.). Is otitis externa usually due to a single cause? Be able to explain (understand the "concept" of why otitis is multifactorial) (overview only III.A.) What are some of the more common inducers of otitis in the dog? In the cat? 3. Be familiar (able to recognize) common historical complaints associated with otitis. Why is it important to perform a physical exam? What clues may the otic discharge afford? What are common changes noted on otoscopic exam? 4. Is it always possible to see the tympanic membrane on otoscopic exam? How may treatment FIRST help insure a better otoscopic exam? What two procedures should be routinely run on otic discharge specimens and what are you looking for? (D.1.a.b.) When are additional diagnostic tests indicated? (2.b.3.) 5. In regards to treatment, be familiar with approach to ear care, ear cleaning and techniques utilized (section V. A.B.C.). Understand the general principals of treatment for bacterial and yeast otitis (brief overview only). What cleansing agents are particularly beneficial for yeast? When are systemic antibiotics or systemic anti-fungal agents indicated? 6. Understand the basic tenants of treatment for the patient with ear mites (why is it important to treat the ears, the patient and all in-contact animals?). Why should most treatment regimens continue for 3 to 4 weeks? 7. What causes otitis media? (A.1.2.) What clinical signs may be present? (B.) and how does diagnostic work-up differ from that of the patient with otitis externa? (C.2.3.). What additional therapeutic strategies are often beneficial in the management of otitis media? (D.2.3.4.). Why is it important to know the impact of topical products on middle ear? (eg, ototoxicity) 8. Which surgery is typically most helpful for patients with chronic otitis externa and media that fails to respond to medical therapy? Tables below from: Western Veterinary Conference 2005 Otitis Externa II (V70) Marcia Schwassmann, DVM, DACVD Veterinary Dermatology Center Maitland, FL, USA **The reader is advised to check all doses stated below in appropriate reference source prior to use. Ceruminolytic Otic Agents Proprietary Name Ingredients Adams Pan-Otic Purified water, isopropyl alcohol, aloe vera, diazolidinyl urea, methylparaben, dioctyl sodium sulfosuccinate, octoxynol, sodium lauryl sulfate, parachlorometaxylenol, propylene glycol ADL Ear Cleanser Cocamidopropyl betaine, peg almond glycerides, almond glycerides, isostearamidopropyl morpholine lactate, salicylic acid, eucalyptol Cerumene 25% squalene in isopropyl myristate liquid petrolatum base ClearX Ear Cleansing Solution 6.5% dioctyl sodium sulfosuccinate, 6% urea peroxide Corium-20 Purified water, SDA-40B 23%, glycerol Earoxide Ear Cleanser 6.5% carbamide peroxide in a glycerin base Otifoam Water, cocamidopropyl betaine, PEG-60, almond glycerides, mackalene 426, salicylic acid, oil of eucalyptus Cleaning/Drying Otic Agents Proprietary Name Ingredients ADL Ear Flushing Drying Lotion Isopropyl alcohol, salicylic acid, eucalyptol, acetamide MEA, propylene glycol, acetic acid, aluminum acetate, hydrolyzed oat protein, wheat amino acids Ace-Otic Cleanser Acetic acid, lactic acid, salicylic acid in surface-active vehicle containing docusate sodium and propylene glycol AloCetic Acetic acid, aloe Bur-Otic Propylene glycol, water, burrow's solution, acetic acid, benzalkonium chloride ClearX Ear Drying Solution Acetic acid, colloidal sulfur, hydrocortisone Chlorhexiderm Flush Chlorhexidine gluconate DermaPet Ear/Skin Cleanser for Pets Acetic acid, boric acid, surfactants Epi-Otic Cleanser 2.5% lactic acid, 0.1% salicylic acid in docusate sodium and propylene glycol base Epi-Otic Cleanser with Spherulites Lactic acid and salicylic acid are present in encapsulated and free forms, chitosanide is present in encapsulated form, in docusate sodium and propylene glycol base Euclens Otic Cleanser Propylene glycol, malic acid, benzoic acid, eucalyptus oil Fresh-Ear De-ionized water, isopropyl alcohol, propylene glycol, glycerin, fragrance, salicylic acid, PEG 75 lanolin oil, lidocaine hydrochloride, boric acid, acetic acid Gent-L-Clens Lactic acid, salicylic acid in propylene glycol Hexadene Flush Water, propylene glycol, 0.25% chlorhexidine gluconate, triclosan, fragrance Nolvasan Otic Special solvent, surfactant Oticalm Benzoic acid, malic acid, salicylic acid, oil of eucalyptus Otic Clear Deionized water, isopropyl alcohol propylene glycol, glycerin fragrance, salicylic acid, PE 75 lanolin oil, lidocaine hydrochloride, boric acid, acetic acid Oti-clens Propylene glycol, malic acid, bend acid, salicylic acid OtiRinse Water, Propylene glycol, SD Alcohol 40, DSS, Glycerin, Nonoxynol-12, Salicylic acid, Lactic acid, Benzoic acid, Benzyl Alcohol, Aloe Vera Otocetic Solution 2% boric acid, 2% acetic acid, surfactants Solvadry 2.7% boric acid, 90% isopropyl alcohol Systemic antibiotics and antifungal agents for otitis Antibiotic Proprietary Recommended Name Dosage Amoxicillin trihydrate-Clavulanate Clavamox potassium 14-22 mg/kg, ql2 h Cefadroxil Cefa-Tabs, CefaDrops 22 mg/kg, ql2 h Cephalexin Generics 22 mg/kg, ql2 h Clindamycin hydrochloride Antirobe 5.5-11 mg/kg, ql2 h Difloxacin hydrochloride Dicural 5-10 mg/kg, q24 h Enrofloxacin Baytril 5-20 mg/kg, q24 h Itraconazole Sporonox 5 mg/kg,q24h Ketoconazole Nizoral 5 mg/kg, ql2 h Orbifloxacin Orbax 2.5-7.5 mg/kg, q24h Marbofloxacin Zeniquin 2.5-5 mg/kg, q 24 h Ormetoprim-sulfadimethoxine Primor 55 mg/kg, q24 h, day 1, then 27.5 mg/kg, q24 h Trimethoprim-sulfadiazine Tribrissen, Di-Trim 20-30 mg/kg, ql2 h Trimethoprim-sulfamethoxazole Generics 20-30 mg/kg, ql2 h Topical Antimicrobial Otic Preparations Proprietary Name Ingredients Conofite Lotion Miconazole Derma 4 Ointment Nystatin, neomycin sulfate, thiostrepton, triamcinolone acetonide Dermagen Ointment Nystatin, neomycin sulfate, thiostrepton, triamcinolone acetonide Dermalone Ointment Nystatin, neomycin sulfate, thiostrepton, triamcinolone acetonide Forte-Topical Hydrocortisone, neomycin sulfate, penicillin G procaine, polymyxin B, chlorobutanol anhydrous Gentocin Ophthalmic Gentamicin sulfate Gentocin Otic Solution Gentamicin sulfate, betamethasone valerate Liquichlor Chloramphenicol, prednisolone, tetracaine, squalene Otomax, DVMax Gentamicin sulfate, betamethasone valerate, clotrimazole Panolog Cream and Ointment Nystatin, neomycin sulfate, thiostrepton, triamcinolone acetonide Quadritop Ointment Nystatin, neomycin sulfate, thiostrepton, triamcinolone acetonide Topagen Ointment Gentamicin sulfate, betamethasone valerate Tresaderm Thiabendazole, dexamethasone, neomycin sulfate Tritop Neomycin sulfate, isoflupredone acetate, tetracaine hydrochloride Veltrim Clotrimazole Additional Topical Therapy for Pseudomonas Otitis Treatment Preparation Dosage Injectable enrofloxacin 1 part injectable enrofloxacin (22.7 mg/ml) + 4 parts vehicle (saline, Synotic, or hydrocortisone) = 4.5 mg/ml 5-10 drops/ear BID Tris-EDTA 12g Tris buffer, 6.05 g EDTA, 1 L Fill ear 15 min prior to distilled water, pH 8, autoclave topical ab BID 15 min Silver sulfadiazine 1:1 up to 1:50 mixed with water 1% 0.5 ml/ear BID Polymyxin B or E 5-10 drops q 4-6 hr. Ticarcillin(Ticar) 40 ml water into 3 gram vial Acetic Acid (2.5 to 5%) 0.5-1 ml q 8 hr. Fill ear canal 2-3 x daily; needs > than 1 minute contact times Available Steroid Preparations Proprietary Name Ingredients Bur-Otic HC 1% hydrocortisone, propylene glycol, water, burrow's solution, acetic acid, benzalkonium chloride ClearX Drying Solution Acetic acid, colloidal sulfur, hydrocortisone Cort/Astrin Solution Burrow's solution, 1% hydrocortisone CortiSpray 1% hydrocortisone Synotic Otic Solution 0.01% fluocinolone acetonide, 60% DMSO Recommended Steroid Preparations for Bacterial Otitis Topical Steroids Oral Prednisone* Mild infection Hydrocortisone (12.5%) Usually not necessary Acute Dexamethasone (0.1%) Chronic Dexamethasone (0.1%) Triamcinolone (0.1%) Betamethasone (0.1%) May Be needed Severe Infections (Pseudomonas) Hydrocortisone (12.5%) May be necessary but use as low a dose as short a time as possible *Prednisone 1.1 to 2.2 mg/kg divided q12hr for 3 to 10 days stop as soon as possible