Lecture: The Immune System
advertisement

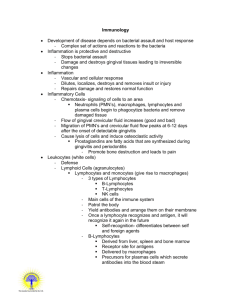
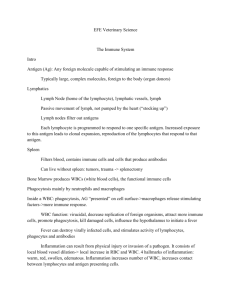
Lecture: The Immune System I. Nonspecific Immune Defenses A. Membrane as Surface Barriers 1. Skin and Mucous Membranes (Epithelium) a. Acidity of the skin and GI tract b. Lysozyme - enzyme of tears/saliva, kills bacteria by damaging cell wall c. Mucus - traps pathogens in nose and bronchi B. Phagocytes (macrophages, neutrophils) 1. Macrophages - “big eaters” that engulf foreign cells a. Kupffer cells - macrophages of liver b. Langerhan’s cells - macrophages of skin c. Histiocytes - macrophages of connective tissue 2. Neutrophils - become phagocytic 3. Opsinization - process by which complement proteins and antibodies bind to pathogen, makes it easier for macrophages and neutrophils to bind and destroy C. Natural Killer Cells (NK’s) 1. Identify and kill cancer cells and virus-infected cells before specific immunity develops D. Inflammation: Response to Tissue Injury 1. Principle signs - redness, heat, swelling, pain 2. Vasodilation and Capillary Permeability a. Chemical mediators - histamine, complement proteins, kinins, prostaglandins, lymphokines b. Hyperemia - above normal blood flow, leads to redness and heat in inflamed area c. Exudates - fluid released at site of inflammation; leads to local swelling and pain i. Aspirin - block prostaglandin production; reducing swelling and pain at inflamed site E. Phagocyte Mobilization 1. Inflammation leads to immediate response by macrophages and neutorphils 2. Leukocytosis inducing factors - act as “chemotactic” guides to lead WBCs to area of inflammation 3. Monocytes slowly join the nonspecific response to injury, becoming contributors over time 4. WBCs engulf microbes and dead tissue so that natural healing of the tissue can occur 5. Pus - mixture of dead neutrophils, tissue, debris 6. Abscess - sac of pus walled off by collagen 7. Infectious granulomas - bacteria surrounded & protected by macrophages (eg. tuberculosis) F. Antimicrobial Proteins 1. Complement system (complement) a. Classical pathway - antibodies bind to antigen; C1, C2, C4 proteins bind C3a + C3b b. Alternate pathway - Factors B, D, P bind to polysaccharide on membrane C3a + C3b c. C3a complement - leads to increased inflammation, capillary permeability, chemotaxis d. C3b complement - activates ‘Membrane Attack Complex” (MAC) of proteins C5, 6, 7, 8, 9; the MAC forms hole in infecting microbe to lyse it 2. Interferons - proteins made by virus-infected cells that signal other cells to protect themselves; also activate macrophages and NK’s a. Treatments - rare leukemias, Karposi’s Sarcoma (AIDS), hepatitis C; experimental for AIDS and other viral infections G. Fever (Body Temperature Above Normal) 1. Pyrogens - molecules released by macrophages in response to infectious agent; increases the temperature “set point” for the body in the hypothalamus 2. Causes the sequestering of Fe and Zn needed by many bacteria to survive; allows increase in metabolic rate in order to fight the infection THE IMMUNE SYSTEM: SPECIFIC BODY DEFENSES II. Overview of Immune System A. Levels of Defense 1. First line of defense - epithelial barriers (skin) 2. Second line of defense - the inflammatory response 3. Third line of defense - the IMMUNE Response B. Features of Specific Immune Response 1. Antigen-specificity - the immune system recognizes and reacts to SPECIFIC foreign molecules 2. Systemic reaction - the entire body reacts, not just the site of infection as in inflammation 3. Memory - the immune system is able to react more quickly and forcefully on future encounters 4. Humoral immunity - production and action of antibodies (B-lymphocytes) 5. Cellular immunity - response of the lymphocytes (cells) to a specific antigen (Tlymphocytes) III. Immune System Cells (B + T lymphocytes, macrophages) A. Features of B + T Lymphocytes 1. B lymphocytes (B Cells) - humoral immunity by producing antibodies against a specific antigen; mature and become “immunocompetent” in bone marrow 2. T lymphocytes (T cells) - cellular immunity; mature and become “immunocompetent” in thymus with hormone direction 3. Antigen receptors - B + T cells produce random receptors on cell surface for random antigens by random combination of genes during fetal development 4. Self-tolerance - those cells that have receptors against “self molecules” are immediately destroyed 5. Differentiation - T + B cells will only reach final maturation when/if their receptor binds to a specific antigen in lymph nodes/organs or the spleen B. Features of macrophages 1. Antigen presenters - most macrophages will engulf foreign material/cells, chop it up, and then “present” parts of molecules on their cell surface to T cells to recgonize and become activated 2. Activated macrophages - activated T cells then release messengers to turn macrophages into killers IV. Antigens (non-self molecules) A. Features of Antigens 1. Types of molecules - almost any molecule that is NOT native to the person can be an antigen; particularly proteins, nucleic acids, lipids, and large polysaccharides 2. Complete antigens - generally larger antigens, can stimulate response by themselves a. Immunogenicity - stimulate development of immunocompetent B + T lymphocytes b. Reactivity - ability to react with B/T cells 3. Incomplete antigen (hapten) - smaller molecule; can react with antibody or T cell, but CANNOT stimulate B/T cell development (non-immunogenic) a. Allergic reaction - haptens may bind with self-proteins and be attacked by immune system 4. Antigenic determinants - those certain portions of an antigen molecule that can be recognized by antibodies, B cells, or T cells V. Humoral Immune Response (Antibodies B-Cell) A. Antigen Challenge & Clonal Selection 1. Antigen challenge - first exposure of antigen with immunocompetent lymphocytes 2. B cell activation - many determinants on antigen bind to receptors of specific B cell 3. Capping - receptors gather together to bind antigen 4. Endocytosis - receptor/antigen complex engulfed 5. Clonal selection - B cells activated by capping duplicate rapidly to produce identical receptors; only B cells with that SPECIFIC antigen receptor will form more and more clones 6. Plasma cell differentiation - B cells differentiate into antibody-producing plasma cells; antibodies are SPECIFIC to that particular antigen 7. Memory cell differentiation - other B cells become longer living “memory” cells 8. Immunologic Memory - Secondary Immune Response - produce identical antibodies in future B. Active vs. Passive Humoral Immunity 1. Active humoral immunity - when B cells encounter antigens; actively produce antibodies a. Natural acquisition - normal exposure to bacteria, viruses, other foreign agents b. Artificial acquisition (vaccine) - person exposed to “weakened” antigens 2. Passive humoral immunity - antibodies from serum of other person/animal harvested and injected a. Gammaglobulin - immune sera for hepatitis b. Other immune sera - used to fight antigens such as venom, botulism, rabies, tetanus VI. Antibody Immunoglobulin - Ig) Structure and Function A. Basic Structure of Antibodies (Immunoglobulins) 1. Antibody monomer - one Y-shaped antibody; composed of 2 LIGHT and 2 HEAVY chains a. Heavy chains - large polypeptides (400 amino acids) bent at a hinge point in middle; connected at the constant region by disulfide bonds b. Light chains - smaller polypeptides attached to heavy chains by disulfide bonds c. Constant © region - area of each that has similar amino acids among Ig type d. Variable (V) region - area of each chain that has DIFFERENT amino acid sequences for each different antibody SPECIFIC for a particular antigen i. Antigen-binding site - area at top of Y where antibody attaches to the antigen ii. Somatic recombination - recombination of genes for the variable region lead to billions of different antibodies for future antigens B. Classes of Antibodies (IgD, IgM, IgG, IgA, IgE) 1. IgD (monomer) - receptor on B cell surface 2. IgM (pentamer) - first Ab released to serum by plasma cells; can “fix” complement for attack 3. IgG (monomer) - most abundant Ab in plasma; generally produced during secondary immune response; can cross placental blood barrier; can “fix” complement proteins for attack 4. IgA (dimer/monomer) - bathe the body surfaces; especially found in mucus 5. IgE (monomer) - involved in allergies (haptens) C. Antigen-Antibody Complex and Its Action 1. Antigen-antibody complex - the structure resulting when Ig binds to its specific antigen 2. Complement fixation/activation - Ig binding to antigen on a foreign cell (bacteria/blood) allows complement to bind and lyse the cell 3. Neutralization - Ig binds to antigen on virus or bacterial exotoxin, leading to phagocyte identification and engulfment 4. Agglutinization - clumping of cells resulting from multiple binding sites of Ig (like IgM); easier to be identified and engulfed by phagocytes 5. Precipitation - clumping of antigen molecules D. Monoclonal Antibodies - hybridized cancer cell and B lymphocyte to make large quantities of desired antibody 1. Diagnosis - used to find particular molecules 2. Treatment - used to fight cancer; used to deliver “attached drugs” to certain cells of body VII. Cell-Mediated Immune Response (T lymphocytes) A. Overview of T cells 1. Effector cells - cytotoxic T cell 2. Regulatory cells - helper T cell, suppressor T Cell 3. CD4 (T4) cells - primarily helper T cells 4. CD8 (T8) cells - cytotoxic and suppressor T cells B. Primary Functions of T Cells 1. B cells can recognize and make antibodies to free antigens in serum or on the surface of microbes; prepares antigen for destruction 2. T cells can only recognize antigens that have been processed and are present on membranes of diseased cells (cancer/virus) a. Viral/bacterial/parasite infected cells b. Cancer cells with antigenic surface proteins c. Infused or transplanted cells 3. Lymphokines - enhance T/B cell + macrophage activity 4. Monokines - stimulate T cells C. T Cell Receptors & Major Histocompatibility Complex (MHC) 1. Major histocompatibility complex (MHC) - proteins on the surface of ALL cells that “present” antigen to cells of the immune system; T cell receptors indentify and bind the MHC-antigen complex a. Class I MHCs - present on ALL cells; cytotoxic T Cells bind to MHCI/antigen complex b. Class II MHCs - present on many WBCs; helper T cells bind to macrophages presenting an antigen c. Immunologic surveillance - process by which T cells “frisk” MHCs of cells look for antigen 2. T cell activation - like B cells, once bound to MHC-antigen complex, T cells multiply; some differentiate into memory T cells for future encounters a. Interleukin 1 (IL-1) - released by macrophages when bound to helper T cell, causes release of IL-2 from the helper T cell b. Interleukin 2 (IL-2) - released by helper T cells, causes quick proliferation of other helper Ts, cytotoxic Ts, and B cells against the same antigen bound to macrophage MHC c. Macrophage activating factor - enhances the ability of macrophages to engulf and destroy VIII. Functions of the Different T Cells A. Helper T cells 1. Stimulate T cells and B cells bound to antigen to proliferate and eradicate the invading antigen 2. Lymphokines - chemical signals released by helper Ts mobilize other Ts, Bs, And neutrophils B. Cytotoxic T Cells (killer T Cells) 1. Hunt down and kill cells presenting MHC-antigens, virus infected cells, bacteria infected cells, cancer cells, and foreign cells (transplants) 2. Steps in killer T Cell Binding/Lysis: a. Killer T cell binds to MHC class I - antigen complex, thereby releasing perforin b. Perforin polymerizes on target cell membrane, forming hole for ion influx and cell lysis c. Tumor necrosis factor - chemical released to destroy cancer cells C. Suppressor T Cells 1. Release lymphokines that slow down and eventually halt the immune response to an antigen IX. Organ Transplants and Preventing Rejection A. Types of Transplants (Grafts) 1. Autograft - tissue taken from one part to another on the same person (skin grafting) 2. Isograft - from one identical twin to another 3. Allograft - graft from within the same species 4. Xenograft - graft from a different species (baboon) B. Preventing Rejection 1. Autografts and isografts rarely rejected 2. Xenografts extremely rare success 3. Allografts much be looked at for ABO blood type and MHC-antigen compatibility 4. Immunosuppressive therapy - suppress the rejection; corticosteroids as antiinflammatory (prednisone) and lymphokine inhibitors (cyclosporine) X. Pathologies of Immune Response A. Immunodeficiencies 1. Congenital thymic aplasia - thymus fails to develop in fetus, T cell production is limited 2. Severe combined immunodeficiency disease (SCID) - few B and T cells, “boy in plastic bubble” 3. Hodgkin’s disease - cancer of lymph nodes 4. AIDS - HIV virus infects CD4 T cell population B. Immediate Hypersensitivity (Type I) 1. Allergen - antigen that stimulates allergic response 2. Anaphylaxis - allergen cross-links IgEs on mast cells and basophils, causing release of histamine and heparin leading to inflammatory response a. Local - runny nose, watery eyes, hives b. Systemic (anaphylactic shock) - allergen enters circulation; bronchiole constriction, circulatory collapse, and possible death 3. Atopy - atypical allergic reaction C. Subacute Hypersensitivity 1. Antibody dependent cytotoxic reaction (TYPE II) - agglutination and lysis of wrong blood transfusion 2. Immune complex hypersensitivity (Type III) - buildup of antibody-antigen complex in local region D. Delayed Hypersensitivity (Type IV) 1. Allergic contact dermatitis - reaction may take 1 to 3 days before symptoms appear XI. Autoimmune Diseases (Self protein becomes Non-self) 1. Change in structure of self-antigens a. Autoimmune thrombocytopenia - T cells attack body platelets when aspirin/antihistamine used b. Rheumatoid arthritis - IgM reaction against altered IgG after streptococcal infection of a joint c. Multiple sclerosis - immune system attacks myelin d. Juvenile diabetes - immune system attacks insulin 2. Self-proteins not exposed during development 3. Cross-reaction of natural antibodies with self proteins a. Rheumatic fever - antibodies against streptococcal infection attack proteins on cardiac muscle