Mech77-IntroImmuneCells

(2)
MOD#77
Friday, May 09, 2003, 11 AM
Dr. Simecka
Rachel Eason for Erica Ayoub
Page 1 of 10
Introduction and Cells of the Immune System
Dr. Puttoff addressed the class before the lecture started. He spoke about 4 issues:
(1) Excused absences—there is a change in procedure regarding this.
They will now be dealt with by Dr. Martin’s office (located at rm
402). Please read the e-mails regarding the new procedures requesting an excused absence.
He is receiving huge amounts of e-mail regarding questions students have. If you are not present at a lecture, CIL, post-exam review, etc.,
(3) please do not send him an e-mail to ask a question about anything you don’t understand. He is a busy man and does not have time to be looking at a bunch of e-mail. He said to look it up in the text.
Cheating—He also has received numerous e-mails regarding this, and in turn, contacted administration himself. He has made changes in the format of the CILs—scantrons will be completed and picked up first, and then there will be a discussion about the questions. This will be a formal examination and should prevent any type of cheating. If he hears about one more case of cheating, the attendance points for the course will also be changed to scored quizzes.
Post-exam reviews—There have been requests for detailed (4) explanations of some of the questions missed. Again, he and other professors do not have time for this, and the answers to these questions can also be looked up in the text.
He introduced Dr. Jerry Simecka who will be in charge of the section on Immunology for the course and also collaborate with him for the Microbiology portion of the course. Dr.
Simecka is head of the section of Microbiology and Immunology in the Department of
Molecular Biology and Immunology. He received his PhD at the University of Alabama at Birmingham.
Dr. Simecka & Dr. Mathews has placed power points on the web along with an outline of topics and a number of study questions from his section. His test questions may be more difficult with use of clinical vignettes.
I. Introduction
A.
Immunology-the study of host response against pathogens/disease, some sort of irritant. It could be cancer, infectious agents, environmental agents, or anything that causes damage to the human. Looks at processes against these entities.
B.
Pathogens—includes 4 major classes
1.
Extracellular—live outside of cells in the tissues
2.
Intracellular—bacteria or parasites that spend part of life cycle inside the cell, a hiding place from the host.
3.
Viruses (intracellular)—replicate using the host’s genetic machinery.
A portion of their life is spent extracellularly.
4.
Parasitic worms
MOD#77
Friday, May 09, 2003, 11 AM
Dr. Simecka
Rachel Eason for Erica Ayoub
Page 2 of 10
5.
Each has a different immune mechanism to attack them. There is some overlap of these immune processes. We should think about the different types of pathogen and which immune response acts best against them as we study this topic.
C.
Defenses and host response
1.
Physical barriers—we are exposed to a number of potential pathogens daily and do not get sick. This is because we have physical barriers such as skin, tears, mucous that protect us against them. In tears, there are enzymes that attack and digest pathogens. Successful pathogens must be able to cross the physical barriers first
2.
Innate immunity—if the physical barriers are breached, there is an immediate response to a pathogen. It (innate immunity) is nonspecific, recognizes a bacteria that is foreign and immediate responds to it.
There are two levels of innate immunity a.
Resident-occurs immediately at the site of recognition and takes care of the problem b.
Induced (inflammation, activated macrophages, etc.)—initial reaction does not work, so a greater response is generated.
3.
Adaptive immune response-if the innate system is not enough, this system is activated. The major difference between the adaptive and the innate system is that the adaptive system has specificity and memory and the innate does not. This system recognizes a specific pathogen and attacks only it. The innate recognizes anything foreign, any sort of pathogen, and will attack it (it has mechanisms for this). It is divided into 2 categories: a.
Humoral (antibody mediated) b.
Cell-mediated (effector T cells)
4.
There is a lot of overlap and interaction between the adaptive and innate immune systems. The innate immunity system can help induce adaptive immunity and adaptive immunity enhances innate immunity.
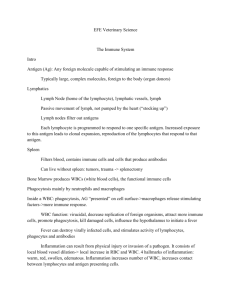
II. Innate immune system
A.
Think of phagocytes-cells that “eat bacteria” –or engulf and destroy them.
There are two major professional phagocytes
1.
Neutrophils
2.
Monocytes/macrophages—monocytes are present in the blood stream and they become macrophages as they migrate out of the blood stream into the tissues.
B.
Natural Killer cells (NK cells)-another cell type that participates in the innate immune system. (This is the area of research of Dr. Mathew)
1.
Their main function is to kill virally infected and tumor cells. They recognize cells that have become ill and then remove them
2.
Produce cytokines, small peptide hormones of the immune system that allows it to communicate between cells. Cytokines can influence the
MOD#77
Friday, May 09, 2003, 11 AM
Dr. Simecka
Rachel Eason for Erica Ayoub
Page 3 of 10 type of immune response, enhance phagocyte function, especially the macrophages. They are, thus, very important.
C.
Complement-Is a cascade of proteins in the plasma that recognizes pathogens and attacks them via the alternative pathway. This system also enhances phagocytosis and recruits other cells.
D.
Inflammation—accumulation of fluids and white blood cells to localize and remove irritants from a site of infection. It also sets up the area for repair of tissues.
III. Adaptive immunity
A.
Specifity and memory are major characteristics.
B.
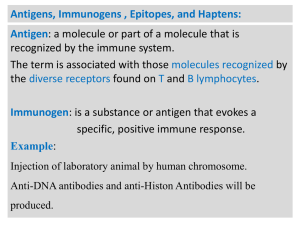
Look at the response of an antibody. (see Figure 1 at end of notes.)
1.
On the x-axis is an individual measured over time. On the y-axis, is a graph of antibody response. Give the person an antigen, a foreign substance that can induce an immune response. Inject the individual with the Ag, and we do not see any response for 3-5 days. Then we will see an antibody response develop that will subsequently fade off.
If we give the individual a second dose of the same antigen, we will see a lag period of only 1-2 days with a much greater response. If we immunize the person at the same time with a completely different antigen, this will take 3-5 days and have a similar response as with the first time we gave the 1 st antigen. The period in which the first antigen was presented is termed the primary response (see graph). The second time the same antigen is presented; it is termed the secondary response. Pay attention to the lag period, with the primary response it is 3-5 days and with the secondary response it is 1-2 days. Also note that there is a much greater response, the second time the antigen is presented. This indicates that there is memory response; this individuals remembers that it saw the antigen before and responds to it more rapidly and greater than before. Finally, this graph shows that the response is specific: as a completely different antigen is given at the same time as the initial antigen, the individual responds to that antigen differently, like the primary response.
2.
There are a number of different classes of antibodies: IgG, IgM, and
IgA (will be discussed in greater detail on Monday). Usually in the primary response, the Ab class is IgM initially, and then we see a IgG response. In the secondary immune response, will see IgG and less
IgM (about the same as the first). There is a switch between being an
IgM dominant response in the primary response to an IgG dominated response in the second immune response. IgM response here will be faster (in the secondary response), but the important thing is that the
IgG response is much greater.
3.
Also affinity maturation, the affinity of the Ab for the Ag (strength of binding, how specific the response is), is much higher in the secondary response than in the primary response.
MOD#77
Friday, May 09, 2003, 11 AM
Dr. Simecka
Rachel Eason for Erica Ayoub
Page 4 of 10
C.
Major cell type is the lymphocyte with two major types of responses
1.
T lymphocytes-regulate immunity, kill infected cells, activate macrophages, etc. He called them the “conductors of immune response.” There are 2 major T-cell populations a.
cytotoxic T cells (with marker on surface, CD8, so known as
CD8+ cells) kill virally infected and cancer cells, as well as cells with intracellular bacteria. So do some of things that
NK cells do, but NK cells recognize cells that are sick and these cells recognize cells that are infected with a specific virus. They recognize the viral antigen that is present on the surface of a virally infected cell. Thus, they recognize things differently. b.
T helper cells (with marker on surface, CD4, so known as
CD4+ cells)
(1) H.I.V. causes depletion of this population of cells so monitor CD8+ to CD4+ ratio and CD4+ number to stage the disease and determine when the patient develops A.I.D.S
(2) They help direct/regulate immune response.
(3) There are two major classes of T helper cells divided based on the different cytokines they produce and determine their function (we need to know these cytokines)
(i) TH1 cells → cell mediated immunity-
IL-2, IFN-γ, TNF-β, and GM-CSF
(ii) TH2 cells involved with humoral immunity-
(activate B cells and help produce more Ab)
IL-4, IL-5, IL-6, IL-13
IV. Adaptive immunity
A.
Humoral (antibody-mediated) immunity
1.
Antibody [Ab] (immunoglobulin) specifically binds to antigen [Ag] and targets its destruction. See figure 2 for structure. The antibody consists of 2 heavy chains that are identical and 2 light chains that are identical. It has a region that binds to a foreign antigen called the variable region. Another portion is called the Fc portion. The Fc portion tells how the foreign Ag will be destroyed and the variable region tells what will be destroyed. An individual can respond to any viruses or foreign material it has not seen. This is because there is a system to generate variable regions that will react with anything. The heavy chain, particularly the Fc portion, determines the class of the
Ab.
2.
Functions of antibodies: a.
Neutralization: Ab binding to Ag inhibits its activity. Toxin works by binding to a receptor on a cell, entering it, and
MOD#77
Friday, May 09, 2003, 11 AM
Dr. Simecka
Rachel Eason for Erica Ayoub
Page 5 of 10 causing effects. The binding of the Ab to it and inhibits it interaction with the receptor prevents this from happening.
Ab can also bind to a virus and prevent it from interacting with a cell receptor. b.
Opsonization: phagocytes have receptors for the Fc portion of an Ab and when an Ab binds to the bacteria, it marks it for phagocytosis more effectively and efficiently. Certain classes of Ab are better at doing this than others. c.
Complement activation: Ab binding to bacteria will help this. d.
Antibody-dependent cell-mediated cytotoxicity (ADCC):
Cells (NK cells, macrophages, neutrophils) recognize Ab bound to target cell and release substances to destroy the target cell. Is different from phagocytosis, which a cell is engulfed.
B.
Cell-mediate immunity—Antigen-specific T cells play a major role
1.
Cytotoxic T cells-lysis of viral and tumor cells
2.
Activation of macrophages by TH 1 cells, e.g., produces cytokines such as gamma-interferon to activate macrophages.
V. Acquired immunity
A.
Passive immunization (host does not generate own response, host given Ab)
1.
Host given antibody, e.g. antivenom, Ab specific for snake venom, binds to snake venom toxins and neutralizes it. Another e.g., is maternal Ab, which are given to fetus via placenta during pregnancy.
At 6 months, an infant seems to get ill more frequently. The maternal
Ab present in the infant are decreasing below levels that are protective, and this is the period of transition when the child starts to generate his own immune response
2.
Is rapid and transient
B.
Active immunization
1.
Host generates own humoral and cell-mediated immune responses, e.g. vaccination
2.
Involves a lag-time (requires 3-5 days before generates a response) and is long-lived (perhaps, a lifetime).
VI. Development of an immune response
A.
Clonal selection theory-Nobel Prize for it (see figure 3)
In bone marrow or developmental tissue (thymus), we have lymphocytes that randomly generate unique receptors in the absence of an antigen or foreign stimulus. The first step is that we need to remove cells with receptors that are specific for self, in order to prevent an immune response against self. If not done, will have a high death rate for the progenitor lymphocyte cells. Other cells survive that do not recognize self, but have unique surface receptors that are not specific. If Ag present now, a cell will become activated and produce many more cells like it. Select a clonal cell that is not reactive to self, but to
MOD#77
Friday, May 09, 2003, 11 AM
Dr. Simecka
Rachel Eason for Erica Ayoub
Page 6 of 10 some specific Ag and expanding it to react quicker at a later time period. Can be B cells also—in the bone marrow. T cells in the thymus.
B.
Activation of lymphocytes requires more than antigen recognition (same concept holds for B cells)
1.
First thing that happens is—cell adhesion molecules (CAM) mediate interactions between T cells and antigen presenting cells (APC). Is non-specific and transient. APC include macrophages, dendritic cells, and B cells
2.
Once the T cell is bound, it is looking for Ag it is specific for. It recognizes peptide bound to Major Histocompatibility Complex
(MHC) molecules. Called HLA in humans. These are the first signals.
These molecules are important in antigen presentation. They are what you match for tissue grafts—called MHC because first recognized in rejected skin grafts. There are two types that are structurally and functionally different a.
CD8+ T cells: recognize peptide bound to MHC I: endogenous antigen b.
CD4+ T cells: recognize peptide bound to MHC II: exogenous antigen ***Remember by 8 x1=8 and 4 x 2=8 c.
T cells only recognize peptide, don’t recognize entire protein. d.
Process of Antigen processing-degrades proteins into peptides. Where peptides arise determines if are MHC I
(from inside cell) or MHC II (outside cell, in phagocytes)
3.
Cells become anergic if they don’t do anything else (only see Ag).
Will forget if Ag is presented again, will not respond to it. Require a second co-stimulatory signal—CD28 on T cells binding to B7 on APC
4.
Same thing occurs with B cells, it recognizes an entire Ag and requires a co-stimulatory signal that is delivered by T helper cells. Look for this in reading.
VII. Immunopathology
A.
Autoimmunity—loss of self-tolerance –will attack some organ or part of body. Different targets determine what autoimmune disease it is, e.g. lupus or rheumatoid arthritis.
B.
Immunodeficiency—there is something wrong with the immune system, the individual cannot respond properly. The most common inherited form is a deficiency of IgA. IgA is associated with mucosal secretions, and individuals with this, cannot respond to GI and respiratory infections. Another common immunodeficiency that is acquired is A.I.D.S., in which individuals lose T helper cells.
C.
Hypersensitivity-the immune system responds, but in a stronger, inappropriate manner. E.g., Allergies, asthma, reaction to poison ivy
D.
Blood transfusion reactions & graft rejections—you are given an individual foreign material (trying to save his/her life) and he/she is responding to it.
VIII. Lymphoid Tissues
MOD#77
Friday, May 09, 2003, 11 AM
Dr. Simecka
Rachel Eason for Erica Ayoub
Page 7 of 10
A.
Primary—refer to immune system development
1.
Hematopoietic tissues
2.
Bone marrow a.
B cell development in adults (liver in fetus) b.
Myeloid cell development c.
T progenitor cells migrate to thymus
3.
Thymus a.
T cell development b.
Removal of self-reactive T cells c.
Reduced activity with aging (elderly not respond to vaccinations well and have not as good response to viral infections)
B.
Secondary—infrastructure where develop immune response to an infection or
Ag
1.
Provide the microenvironment
2.
Lymph nodes
3.
Spleens—for Ag that are blood-borne. If removed or lost, an individual is more susceptible to blood borne infections. (was on a board exam)
4.
Mucosal associated lymphoid tissues (MALT)—along mucosal surfaces, largest site of immune system (would cover ¾ of a tennis court) a.
Peyer’s patches b.
BALT
IX. Two major lineages
A.
Myeloid cells
1.
Monocytes and macrophages
2.
Neutrophils (PMNs)
3.
Mast cells-allergies and parasites, other inflammatory responses
4.
Basophils- allergies and parasites?
5.
Eosinophils-allergies and parasites
B.
Lymphocytes
1.
T cells [T cell receptor (TCR), CD3] a.
TH cells (CD4) b.
CTL (cytotoxic T lymphocytes (CD8)
2.
B cells [surface immunoglobulin (slg)]
3.
NK cells (Fc receptor, no TCR or slg)
C.
Other cells
1.
Interdigitating dendritic cells- potent Ag presenting cells to T cells— both myeloid and lymphoid derived populations
2.
Langerhan’s cells—skin a.
pick up Ag in skin and bring to lymph nodes to T cells b.
maturation to APC during migration
MOD#77
Friday, May 09, 2003, 11 AM
Dr. Simecka
Rachel Eason for Erica Ayoub
Page 8 of 10
3.
Follicular dendritic cells-germinal centers
***Captures immune complexes and presents antigen to B cells, not T cells. Called dendritic cells due to morphology, not function. Unlike langerhan’s and interdigitating dendritic cells, which present to T cells.
MOD#77
Friday, May 09, 2003, 11 AM
Dr. Simecka
Rachel Eason for Erica Ayoub
Page 9 of 10
MOD#77
Friday, May 09, 2003, 11 AM
Dr. Simecka
Rachel Eason for Erica Ayoub
Page 10 of 10