Cytokine Profiles In Peripheral Blood Of IBD Patients
advertisement
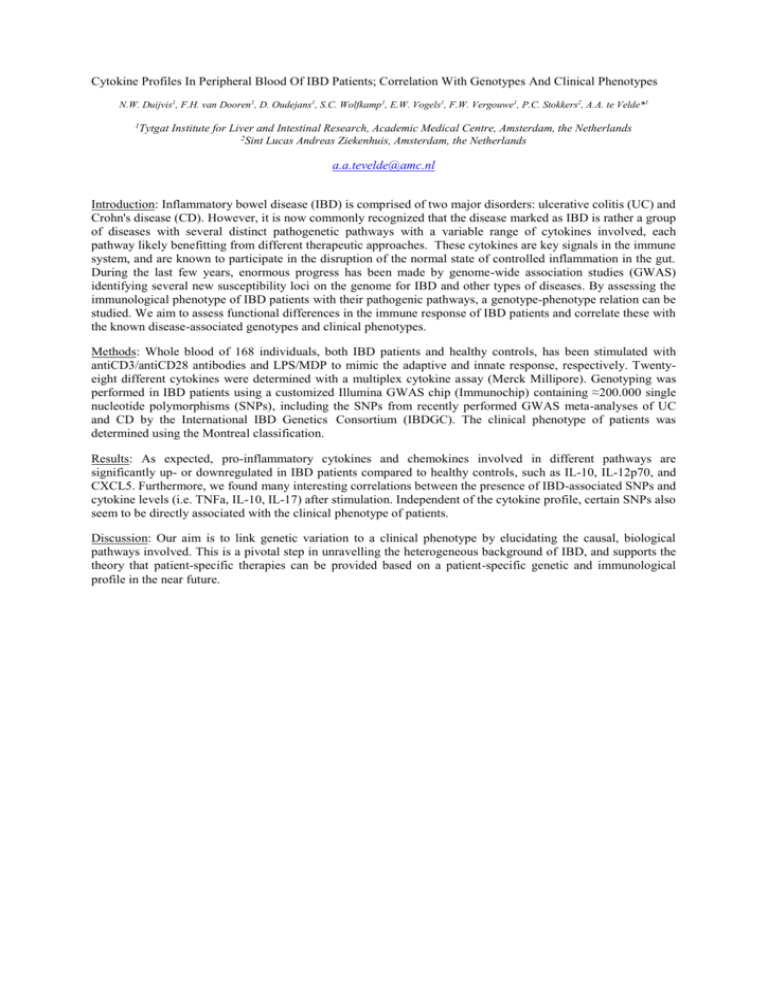
Cytokine Profiles In Peripheral Blood Of IBD Patients; Correlation With Genotypes And Clinical Phenotypes N.W. Duijvis1, F.H. van Dooren1, D. Oudejans1, S.C. Wolfkamp1, E.W. Vogels1, F.W. Vergouwe1, P.C. Stokkers2, A.A. te Velde*1 1Tytgat Institute for Liver and Intestinal Research, Academic Medical Centre, Amsterdam, the Netherlands 2Sint Lucas Andreas Ziekenhuis, Amsterdam, the Netherlands a.a.tevelde@amc.nl Introduction: Inflammatory bowel disease (IBD) is comprised of two major disorders: ulcerative colitis (UC) and Crohn's disease (CD). However, it is now commonly recognized that the disease marked as IBD is rather a group of diseases with several distinct pathogenetic pathways with a variable range of cytokines involved, each pathway likely benefitting from different therapeutic approaches. These cytokines are key signals in the immune system, and are known to participate in the disruption of the normal state of controlled inflammation in the gut. During the last few years, enormous progress has been made by genome-wide association studies (GWAS) identifying several new susceptibility loci on the genome for IBD and other types of diseases. By assessing the immunological phenotype of IBD patients with their pathogenic pathways, a genotype-phenotype relation can be studied. We aim to assess functional differences in the immune response of IBD patients and correlate these with the known disease-associated genotypes and clinical phenotypes. Methods: Whole blood of 168 individuals, both IBD patients and healthy controls, has been stimulated with antiCD3/antiCD28 antibodies and LPS/MDP to mimic the adaptive and innate response, respectively. Twentyeight different cytokines were determined with a multiplex cytokine assay (Merck Millipore). Genotyping was performed in IBD patients using a customized Illumina GWAS chip (Immunochip) containing ≈200.000 single nucleotide polymorphisms (SNPs), including the SNPs from recently performed GWAS meta-analyses of UC and CD by the International IBD Genetics Consortium (IBDGC). The clinical phenotype of patients was determined using the Montreal classification. Results: As expected, pro-inflammatory cytokines and chemokines involved in different pathways are significantly up- or downregulated in IBD patients compared to healthy controls, such as IL-10, IL-12p70, and CXCL5. Furthermore, we found many interesting correlations between the presence of IBD-associated SNPs and cytokine levels (i.e. TNFa, IL-10, IL-17) after stimulation. Independent of the cytokine profile, certain SNPs also seem to be directly associated with the clinical phenotype of patients. Discussion: Our aim is to link genetic variation to a clinical phenotype by elucidating the causal, biological pathways involved. This is a pivotal step in unravelling the heterogeneous background of IBD, and supports the theory that patient-specific therapies can be provided based on a patient-specific genetic and immunological profile in the near future.