Get this release in Word format
advertisement
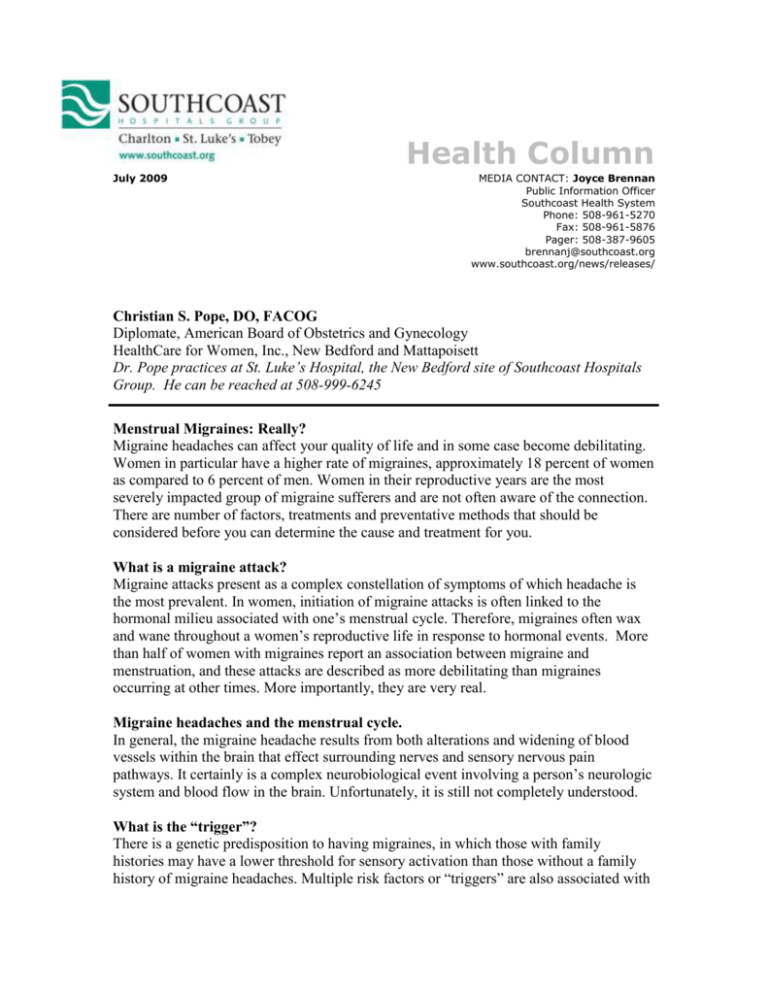
Health Column July 2009 MEDIA CONTACT: Joyce Brennan Public Information Officer Southcoast Health System Phone: 508-961-5270 Fax: 508-961-5876 Pager: 508-387-9605 brennanj@southcoast.org www.southcoast.org/news/releases/ Christian S. Pope, DO, FACOG Diplomate, American Board of Obstetrics and Gynecology HealthCare for Women, Inc., New Bedford and Mattapoisett Dr. Pope practices at St. Luke’s Hospital, the New Bedford site of Southcoast Hospitals Group. He can be reached at 508-999-6245 Menstrual Migraines: Really? Migraine headaches can affect your quality of life and in some case become debilitating. Women in particular have a higher rate of migraines, approximately 18 percent of women as compared to 6 percent of men. Women in their reproductive years are the most severely impacted group of migraine sufferers and are not often aware of the connection. There are number of factors, treatments and preventative methods that should be considered before you can determine the cause and treatment for you. What is a migraine attack? Migraine attacks present as a complex constellation of symptoms of which headache is the most prevalent. In women, initiation of migraine attacks is often linked to the hormonal milieu associated with one’s menstrual cycle. Therefore, migraines often wax and wane throughout a women’s reproductive life in response to hormonal events. More than half of women with migraines report an association between migraine and menstruation, and these attacks are described as more debilitating than migraines occurring at other times. More importantly, they are very real. Migraine headaches and the menstrual cycle. In general, the migraine headache results from both alterations and widening of blood vessels within the brain that effect surrounding nerves and sensory nervous pain pathways. It certainly is a complex neurobiological event involving a person’s neurologic system and blood flow in the brain. Unfortunately, it is still not completely understood. What is the “trigger”? There is a genetic predisposition to having migraines, in which those with family histories may have a lower threshold for sensory activation than those without a family history of migraine headaches. Multiple risk factors or “triggers” are also associated with migraine attacks: alcohol consumption, excessive stress, dietary changes, change in sleeping patterns, and hormonal change due to menstruation. Menstrual migraines affect 12 million women and are defined as occurring two days before and/or three days after the start of menstruation. Migraines associated with menstruation do not occur at any other time during the menstrual cycle, and women must experience attacks in two out of three cycles. Symptoms are described as a one-sided headache, pulsating quality,moderate to severe intensity and aggravation with physical activity. In addition, sufferers may experience nausea, but usually not light and sound sensitivity. Why do I have wacked out hormones? There is a diminished secretion of ovarian hormones during the premenstrual phase, including a decline in progesterone and estrogen levels. It is thought that the consistent ebb and flow in the hormonal milieu during the reproductive cycle functions as a trigger in provoking migraines. Studies have shown that an abrupt drop in estrogen levels following a period of sustained high levels with trigger migraines. This drop occurs right before menses begins. Other hormonal changes associated with the menstrual cycle are increases in prostaglandin levels, magnesium deficiency, and drops in serotonin levels. What? Wacked out hormones? No, just kidding, this is considered a normal fluctuation in hormone levels. Does anything help? There is no standard quick fix. It depends on the patient. Treatment should be tailored to the individual woman’s needs and severity. A combination of patient education and behavior modification with pharmacologic therapies usually works well. Many women try non-medical treatment to manage their migraines before they begin drug therapy. Such therapies include behavior modifications such as relaxation strategies and training, as well as physical therapies like acupuncture, yoga, osteopathic cranio-sacral manipulation, massage, Rolfing, and increased in regular exercise. Quitting smoking and not consuming excessive alcohol are also recommended. Keep a headache diary. A headache diary can be an excellent and effective tool in tracking symptoms, severity and frequency of migraine attacks. Triggers can usually be found based on analysis of the headache diaries and should be avoided as much as possible. Make sure you share this diary with your physician. What medications work? There are two ways to treat migraine headaches: acute therapy, of which there are classes of medications to abolish a headache right away; and preventive therapy, of which there are several options. The three classes of medications that treat a menstrual migraine effectively are nonsteroidal anti-inflammatory drugs (NSAIDS), Triptans, and Ergots. As a general guideline, if at least 80 percent relief from headache pain is not achieved after taking pain relievers such as ibuprofen, acetaminophen or Advil, for a period of 4-6 hours, or if treatment needs to be used continuously for more than two days, you should contact your physician as prescription treatment may be suggested. A quick note, taking pain relievers for an extended period of time can lead to other serious side effects such as liver damage and stomach ulcers, therefore their use should not be long-term. Naproxen sodium is the first line NSAID treatment for the treatment of migraine and usually does the trick. Preventative medications Preventative medications used include b-blockers, calcium channel blockers, tricyclic antidepressants, anticonvulsants, NSAIDS, hormonal therapy (hormonal and oral contraceptives, estrogen topical patches and gels) and rarely GnRH agonists. Short-term prevention is effective in women with predictable menstrual cycles. Perimenstrual treatment such as Naproxen or Frovatriptan with monthly regimens can work. Estrogen treatment has also proven to be effective to try to prevent the sudden drop in estrogen levels that accompanies the onset of menses and the prevailing headache. All such medications carry potential risks that must be considered and the benefits of alternative therapies should be reviewed together with your physician prior to starting treatment. Treatment can help restore your quality of life Migraine is a common, complex and bewildering malady, affecting nearly 28 million Americans and often associated with substantial disability. Menstruation often is a significant trigger of migraine in women and causes major disruption in women’s quality of life. Multiple treatment options are now available for both acute and prevention of migraine that help restore the function and quality of life in women with menstrual migraine. Menstrual migraines, yes really. # # #

![[Plan Logo] [INSERT DATE] Dear Plan Member: Migraines can be](http://s3.studylib.net/store/data/007204786_1-1e3272ccd311201e3ba31cbff3397a69-300x300.png)