Better Cancer Care, an Action Plan
advertisement
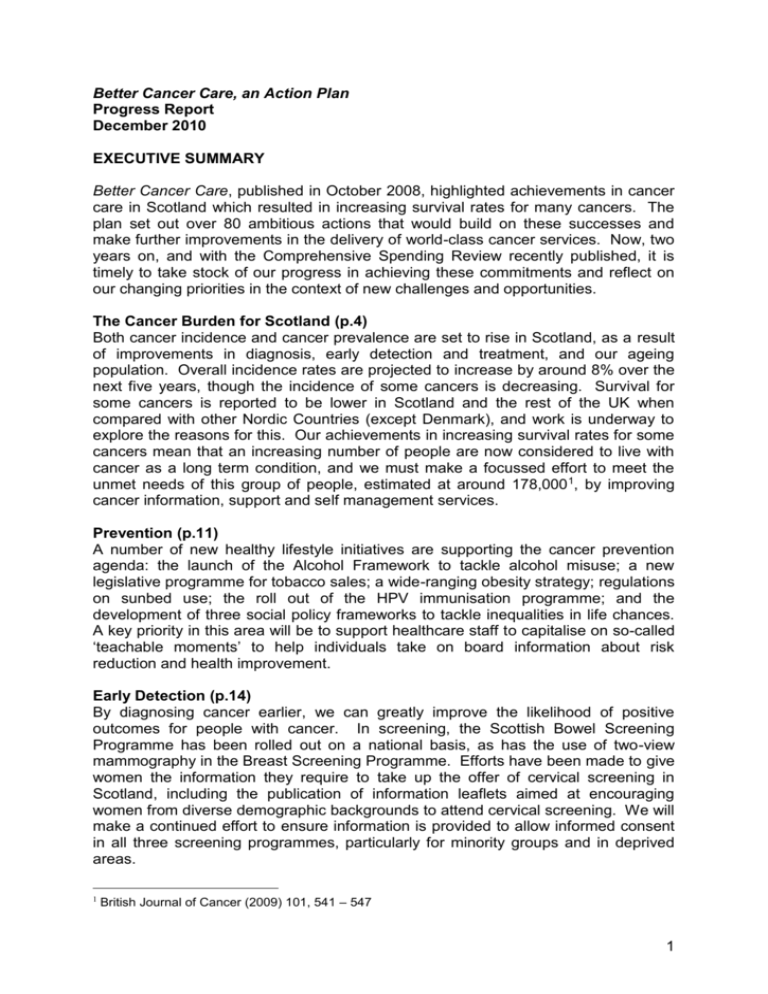
Better Cancer Care, an Action Plan Progress Report December 2010 EXECUTIVE SUMMARY Better Cancer Care, published in October 2008, highlighted achievements in cancer care in Scotland which resulted in increasing survival rates for many cancers. The plan set out over 80 ambitious actions that would build on these successes and make further improvements in the delivery of world-class cancer services. Now, two years on, and with the Comprehensive Spending Review recently published, it is timely to take stock of our progress in achieving these commitments and reflect on our changing priorities in the context of new challenges and opportunities. The Cancer Burden for Scotland (p.4) Both cancer incidence and cancer prevalence are set to rise in Scotland, as a result of improvements in diagnosis, early detection and treatment, and our ageing population. Overall incidence rates are projected to increase by around 8% over the next five years, though the incidence of some cancers is decreasing. Survival for some cancers is reported to be lower in Scotland and the rest of the UK when compared with other Nordic Countries (except Denmark), and work is underway to explore the reasons for this. Our achievements in increasing survival rates for some cancers mean that an increasing number of people are now considered to live with cancer as a long term condition, and we must make a focussed effort to meet the unmet needs of this group of people, estimated at around 178,000 1, by improving cancer information, support and self management services. Prevention (p.11) A number of new healthy lifestyle initiatives are supporting the cancer prevention agenda: the launch of the Alcohol Framework to tackle alcohol misuse; a new legislative programme for tobacco sales; a wide-ranging obesity strategy; regulations on sunbed use; the roll out of the HPV immunisation programme; and the development of three social policy frameworks to tackle inequalities in life chances. A key priority in this area will be to support healthcare staff to capitalise on so-called ‘teachable moments’ to help individuals take on board information about risk reduction and health improvement. Early Detection (p.14) By diagnosing cancer earlier, we can greatly improve the likelihood of positive outcomes for people with cancer. In screening, the Scottish Bowel Screening Programme has been rolled out on a national basis, as has the use of two-view mammography in the Breast Screening Programme. Efforts have been made to give women the information they require to take up the offer of cervical screening in Scotland, including the publication of information leaflets aimed at encouraging women from diverse demographic backgrounds to attend cervical screening. We will make a continued effort to ensure information is provided to allow informed consent in all three screening programmes, particularly for minority groups and in deprived areas. 1 British Journal of Cancer (2009) 101, 541 – 547 1 Genetic and Molecular Testing (p.16) Collaborative working in genetic services has been significantly strengthened, through, for example, the establishment of the Scottish Clinical Genetics Forum, a joint endocrine clinic in Glasgow, the Molecular Pathology Review Group, and closer links with the Scottish Genetic Research Network. The challenge now is to ensure the implementation of current, evidence-based follow up protocols for high risk individuals and ensure continued support for collaboration and research in a financially constrained environment. Referral and Diagnosis (p.18) To support GPs to make prompt and appropriate referrals, a Quick Reference Guide to the Scottish Referral Guidelines for Suspected Cancer was issued to all practices in Scotland, and all regions now have electronic patient referral systems. There is a risk that incidence rates will continue to rise if people are unaware of or ignore good health messages and warning signs and present late. One of the foremost priorities for SCT next year will be to facilitate a coordinated approach to promote greater awareness of the signs and symptoms of cancer amongst members of the public to encourage earlier presentation and rapid diagnosis. A second piece of awarenessraising work amongst medical professionals will complement this activity. Treatment (p.20) New and updated guidance has been produced on the management of people with a family history of cancer, the safe use of intrathecal chemotherapy and the safe use of vinca alkaloids. Guidance on access to new medicines has also been produced, following a Public Petition on the issue. The Chemotherapy ePrescribing and Administration System (CEPAS) is being rolled out across NHSScotland and the Chemotherapy Planning and Oncology Resource Tool (C-PORT) has been piloted and implementation is now being considered by the Regional Cancer Networks. The Scottish Radiotherapy Advisory Group will be focussing on future demand and capacity planning as well as undertaking a national procurement exercise for the replacement of radiotherapy equipment, both particularly important challenges in the current financial climate. A key priority for SCT in cancer treatment will be to look at how surgical oncology services can be developed to maximise clinical quality and efficiency. Acute oncology, including emergency and unplanned care for patients with the major cancers, will also be reviewed. Living with Cancer (p.23) We recognise that there is room for great improvement in providing equitable access to high quality, integrated and tailored information and support services across Scotland. The Living with Cancer Group has developed an action plan to address these issues, with increased focus on partnership working between healthcare, social care and voluntary sector providers, and giving the individual support to make decisions about their own care. Improving post-treatment outcomes for patients will also be achieved through NHSinform and the Self Management programme. Encouraging a culture shift to achieve coordinated and high-impact outcomes will be a significant challenge in the future. 2 Improving Quality of Cancer Care (p.26) A review of the cancer clinical audit resource across Scotland has been undertaken to underpin the cancer quality work programme, which includes the development of national quality performance indicators (QPIs). Work to identify QPIs for renal and prostate cancer is progressing well and QPI development for breast cancer is due to start in December 2010. The sequencing of the remaining tumour groups has also been agreed. Patient experiences are being captured to inform quality improvement and service redesign through the Better Together Programme. We have now exceeded the previous 62-day 95% waiting times target for five consecutive quarters and new waiting time targets which were published in Better Cancer Care, An Action Plan now include screened-positive patients. A new 31-day target has been introduced for all patients diagnosed with cancer (whatever their route of referral) from decision to treat to treatment. Further work is needed to ensure the sustainability of these activities and continue to support quality improvement with reduced human and financial resources. Delivery (p.29) To oversee delivery of the commitments in Better Cancer Care, the Scottish Cancer Taskforce was established and four subgroups tasked with implementing specific programmes of work. The challenge for SCT now is to provide strategic leadership whilst supporting NHSScotland to use its expertise to undertake delivery of high quality cancer services against a reduced financial background. The recently launched NHSScotland Healthcare Quality Strategy2 establishes a new context for measurable quality improvement in the provision of all health services, and this will frame the development of an efficiency and productivity programme for cancer services. SCT will need to encourage greater collaboration to overcome traditional boundaries. This will enable more flexible working and service sharing as well as strengthening the role of regional cancer networks and the relationship the networks have with central government. Looking ahead This report outlines some of the challenges for the cancer sector in Scotland and our future priorities have been identified. The next step for SCT is to look at what actions need to be taken to address these issues, define the consequences of not taking these actions, put measures in place to mitigate risks, and establish a robust system for evaluation of future work. We will also seek to strengthen routes of communication to key stakeholders to ensure ongoing engagement and partnership working. We recognise that there are a number of areas which require a greater focus, for example paediatric oncology, awareness raising, exploring service models for delivery of acute oncology, surgical oncology and an efficiency and productivity programme for cancer which will all contribute to ensuring the best use of resources for the benefit of patients. 2 NHSScotland Healthcare Quality Strategy, launched 10 May 2010: http://www.scotland.gov.uk/Topics/Health/NHS-Scotland/NHSQuality/Q/EditMode/on/ForceUpdate/on 3 THE CANCER BURDEN FOR SCOTLAND Cancer in Scotland (October 2010: Information Services Division) describes the characteristics of the cancer burden in Scotland and the following statistics and figures are taken from this report. (http://www.isdscotland.org/isd/servlet/FileBuffer?namedFile=Cancer_in_Scotland_s ummary_m.pdf&pContentDispositionType=inline) In 2008, just over 28,600 new cases of cancer were diagnosed in Scotland, excluding non-melanoma skin cancers. Non-melanoma skin cancers are very common, but usually have excellent survival. It can be difficult to ascertain all cases, and some cancer registries do not even attempt to collect information on these tumours. For this reason, they are often omitted from figures for all cancers combined. For males, the most common cancers are prostate, lung and colorectal cancers, accounting for around 53% of cancers in men (Figure 1). For females, the most common cancers are breast, lung and colorectal cancers, accounting for almost 56% of cancers in women (Figure 2). Figure 1: Ten most commonly diagnosed cancers in males, 2008 Other 20.6% Prostate 19.4% Kidney 3.3% Bladder 3.5% Trachea, bronchus and lung 17.9% Non-Hodgkin's lymphoma 3.6% Stomach 3.7% Malignant melanoma of skin 3.7% Oesophagus 4.0% Head and Neck 5.2% Colorectal 15.2% 4 Figure 2: Ten most commonly diagnosed cancers in females, 2008 Other 22.1% Breast 28.3% Head and Neck 2.1% Kidney 2.2% Pancreas 2.2% Non-Hodgkin's lymphoma 2.9% Corpus uteri 4.0% Trachea, bronchus and lung 15.8% Ovary 4.2% Malignant melanoma of skin 4.4% Colorectal 11.7% Lung cancer is still the most common cancer overall for males and females (almost 17% of all cancers), with around 4,800 cases diagnosed in 2008, compared to around 4,200 cases of breast cancer (almost 15%) and around 3,800 cases of colorectal cancer (just over 13%). Table 1 sets out the incidence for different tumour types for males and females in Scotland in 2008 and compares the changes in incidence rates since 1998. Key points to note include: The considerable increase in incidence of melanoma of the skin since 1998 in both males and females; The incidence rate of lung cancer has risen by approximately 16% in women while it has decreased by around 18% in men over the past 10 years; The incidence rate of kidney cancer has increased and it is now in the top ten cancers for both males and females. 5 Table 1: Most common cancers in Scotland in 2008 Rank, number, frequency in 2008, and estimated change in incidence rate since 1998 Males Rank ICD-10 site grouping 1 2 3 4 5 6 7 8 9 10 19.4% 17.9% 15.2% 5.2% 4.0% 3.7% 3.7% 3.6% 3.5% 3.3% 10 year % change1 +16.8 -18.3 -4.1 -7.3 +2.3 +68.4 -27.7 +6.6 -31.0 +15.8 <0.0001 <0.0001 0.0589 0.0334 0.5973 <0.0001 <0.0001 0.1563 <0.0001 0.0024 2,843 20.6% x x 13,790 100.0% -3.8 <0.0001 Number Frequency Number Frequency Prostate (C61) Trachea, bronchus and lung (C33-C34) Colorectal (C18-C20) Head and Neck (C00-C14, C30-C32) Oesophagus (C15) Malignant melanoma of skin (C43) Stomach (C16) Non-Hodgkin's lymphoma (C82-C85) Bladder (C67)2 Kidney (C64-C65) 2,673 2,462 2,097 715 546 515 512 490 485 452 Other malignant neoplasms All malignant neoplasms excluding non-melanoma skin cancer p-value Females 28.3% 15.8% 11.7% 4.4% 4.2% 4.0% 2.9% 2.2% 2.2% 2.1% 10 year % change1 +7.9 +16.3 -1.6 +71.3 -6.9 +23.1 +2.0 -5.4 +25.6 -5.9 <0.0001 <0.0001 0.4825 <0.0001 0.0612 <0.0001 0.6673 0.2845 0.0001 0.2602 3,280 22.1% x x 14,848 100.0% +3.9 <0.0001 Rank ICD-10 site grouping 1 2 3 4 5 6 7 8 9 10 Breast (C50) Trachea, bronchus and lung (C33-C34) Colorectal (C18-C20) Malignant melanoma of skin (C43) Ovary (C56) Corpus uteri (C54) Non-Hodgkin's lymphoma (C82-C85) Pancreas (C25) Kidney (C64-C65) Head and Neck (C00-C14, C30-C32) 4,206 2,348 1,744 649 618 597 436 333 323 314 Other malignant neoplasms All malignant neoplasms excluding non-melanoma skin cancer p-value The apparent fall in bladder cancer incidence in males is due to a change in classification and coding practice across cancer registries in Europe; around a quarter of bladder tumours are no longer coded as invasive bladder cancers. 6 New projections Information Services Division (ISD) has carried out further projections on the number of new cancer cases which can be expected in the coming years. Table 2 sets out the average number of new cases per annum for two time periods, together with the projected change. The high number of projected cases of prostate cancer may be due to recent changes in incidence, resulting from the introduction and increasing use of the prostate-specific antigen (PSA) test. Key points to note from table 2 include that the number of new cancer cases is expected to increase by approximately 8% every 5 years up to 2020. This is largely due to our ageing population, and does not take account of any future behavioural or lifestyle changes. Table 2: Average number of new cases per annum and projected number of new cases per annum, by tumour type All Cancer(excluding C44) Lung Kidney Stomach Melanoma of skin Leukaemia Colorectal Colon Rectum Brain & CNS Head & neck Bladder Oesophagus Hodgkins Non-Hodgkins Panceas Other Breast Corpus Uteri Cervix Ovarian Prostate Testis Actual 2003-2007 27352 4692 717 800 927 651 3513 2332 1180 382 1040 1610 832 141 916 634 3152 4004 518 285 623 2577 197 Projected 2013-2017 32256 4691 912 741 1350 811 4202 2748 1453 398 1288 1824 1030 156 1212 711 3690 4820 610 242 694 3805 221 % change 18 0 27 -7 46 25 20 18 23 4 24 13 24 11 32 12 17 20 18 -15 11 48 12 Cancer survival in Scotland Overall, around 2.4% of men and 3.2% of women in Scotland are living with cancer (2,352 and 3,186 per 100,000 population). These numbers are projected to rise because of increasing survival. Although survival following a diagnosis of cancer has increased over time in Scotland, the results of successive EUROCARE studies of cancer survival across Europe suggest that survival from major cancers, like breast and colorectal cancer, 7 has been lower in Scotland and the rest of the UK compared to all the Nordic countries (except Denmark (figure 3)). It is important to bear in mind that there are many possible explanations for survival differences, of which the quality of cancer services is only one. Other possible explanations for reported variation in survival include differences in data quality, differences in the characteristics of people developing cancer, and differences in tumour-related factors.3 Scotland and the rest of the UK have higher than average survival for some cancers suggesting that the survival differences observed are unlikely to be explained by differences in data quality alone. For the major cancers, analysis suggests that most of the excess risk of mortality in Scotland and the UK compared to the Nordic countries (except Denmark) occurs within a year of diagnosis (recent research suggests much of the excess risk of death occurs within a month, especially for the elderly). For patients who survive more than a year after diagnosis, survival at five years is less different from that reported by the Nordic countries (figure 4). One interpretation is that patients in the UK may be presenting, on average, with more advanced disease at the time of diagnosis. It remains unclear whether advanced disease in the UK might be due principally to delays in presentation, referral or diagnosis, or due to more rapidly progressive disease, or a combination of these and other influences. There is certainly evidence that some patients present a long time after developing relevant symptoms. Awareness of symptoms of some cancers appears to be low in Britain, particularly in men, younger people, and people from lower socio-economic status groups or ethnic minorities. Other influencing factors may include perceived barriers to seeking professional medical advice. There is some limited evidence that interventions aimed at individuals may increase cancer awareness, and that community interventions may promote awareness and early presentation. However, it is also important to consider potential unintended adverse consequences of any interventions, such as overburdening diagnostic services. Evidence that delays are associated with more advanced stage of disease or lower survival is not consistent and sometimes counter-intuitive. Presumably, this is explained by the fact that some patients with rapidly progressing disease are simply more likely to present quickly and to be fast-tracked by the NHS. Existing studies of the impact of delay on outcome have a number of limitations including variable ways of defining delays, different ways of measuring delays, failure to allow for the aggressiveness of tumours, failure to allow for emergency admissions, and failure to take account of lead-time bias (that is, prolongation of survival time simply due to allocation of an earlier date of diagnosis, irrespective of whether the date of death has been postponed). While it does seem that presentation with advanced disease may be inevitable for some patients, this should not be used to defend avoidable delays faced by other patients living with the anxiety that they may (or do) have cancer. 3 Black RJ, et al. Interpretation of population-based cancer survival data. In: Sankaranarayanan R. Black RJ, Parkin DM (eds). Cancer Survival in Developing Countries. IARC Scientific Publications No. 145. Lyon: International Agency for Research on Cancer, 1998. 8 Figure 3 - Breast cancer and colorectal cancer diagnosed 1995-99. Five year relative survival by country 90 80 70 % surviving 60 Denmark England Scotland Finland Norway Sweden 50 40 30 20 10 0 Breast Colorectal Source: EUROCARE-4 Study4 Figure 4 - Colorectal cancer diagnosed 1995-99. Five year relative survival vs survival conditional on surviving at least one year 80 70 60 % surviving 50 Denmark England Scotland Finland Norway Sweden 40 30 20 10 0 5-year Relative survival Conditional survival Source: EUROCARE-4 Study 4 Sant M, Allemani C, Santaquilani M, Knijn A, Marchesi F, Capocaccia R, and the EUROCARE Working Group. EUROCARE-4. Survival of cancer patients diagnosed in 1995-1999. Results and commentary. Eur J Cancer 2009; 45: 931–991. 9 Cancer Prevalence Advances in cancer diagnosis, new treatment techniques and advances in radiotherapy, surgery and chemotherapy all mean that cancer is now very often a long term condition. Many people survive and live with cancer and this brings with it a range of physical, social, emotional and often financial challenges. As a result, there is a need to plan carefully to provide high quality services to meet the needs of this group of patients. The British Journal of Cancer published cancer prevalence data in 2009, which quantified the number of people living with and beyond a cancer diagnosis in the four UK nations. For Scotland, this figure was 178,750, as at 31 December 2008.5 It is difficult to achieve a complete and accurate picture of cancer prevalence, due to the fact that some patients may be ‘lost-to-follow-up’ throughout the course of their lifetime. Furthermore, patients with inactive disease make no call on healthcare services and those who are considered cured are unlikely to make use of the support services provided for people living with cancer. Nevertheless, recognising these caveats, these data are a useful planning tool to allow us to gauge the scale of need for cancer support services. Summary of Key Points 5 Cancer is set to rise by approximately 8% every 5 years; Incidence rates in some tumour types are declining whereas others are rising; Survival for some cancers is reported to be lower in Scotland and the rest of the UK when compared with other Nordic Countries (except Denmark); Recent research has highlighted that there is poorer survival in the UK in the first month and first year after diagnosis, however, after the first year, survival in the UK is more similar to other countries; There is an urgent need to understand what the reasons are for this reduced survival in the UK during that first year. Possible reasons for this include data quality issues, tumour related reasons, different genetic and underlying health characteristics of the people getting cancer in different countries, and healthcare related factors. Advances in diagnosis and treatment and the ageing population mean that cancer prevalence is increasing and more people will live longer after their cancer diagnosis and treatment. British Journal of Cancer (2009) 101, 541 – 547 10 BETTER CANCER CARE PROGRESS REPORT 2010 PREVENTION (Actions 1-10) KEY AIMS Better Cancer Care outlined the healthy lifestyle choices that people can make to reduce their risk of getting cancer, for example, stopping smoking or not starting in the first place, reducing alcohol intake to recommended levels, undertaking more physical activity and maintaining a healthy weight and diet. The Scottish Government will continue to implement its wide-ranging programme of action to promote healthier behaviour. We also remain committed to reducing the known health inequalities that exist in our society by focussing on underlying causes, such as negative early years experiences, poverty, unemployment and poor physical and social environments. We also remain committed to reducing the impact of environmental issues on health. PROGRESS AND ACHIEVEMENTS AGAINST ACTIONS Healthy Lifestyle and Cancer Prevention Comprehensive action plans have been published and are being implemented to address the lifestyle factors known to increase individuals risk of getting cancer including: Scotland’s Future is Smoke-free: A Smoking Prevention Action Plan - our longer-term, strategic approach to smoking prevention has seen more people making ‘quit attempts’, and quit smoking, through our free stop-smoking services than any time in the past. Preventing Overweight and Obesity in Scotland: A Route Map Towards Healthy Weight set out four key areas in which action is likely to have the greatest effect on obesity prevention; reducing demand for and consumption of excessive amounts of high calorie foods and drinks; increasing opportunities for uptake of physical activity; establishing life-long healthy habits in children, including encouraging greater consumption of fruit and vegetables; and increasing the responsibility of organisations for the health and wellbeing of their employees. Scotland’s first Cooking Bus has been introduced and to June 2010, 7,679 children, 888 teachers and 328 community volunteers have benefitted from healthier cooking sessions on the bus. In addition the programme has distributed £85,000 of cooking equipment to schools and community food initiatives. `Changing Scotland’s Relationship with Alcohol: A Framework for Action` was launched in March 2009 and contained a comprehensive package of more than 40 measures to tackle the extent of alcohol misuse in Scotland. This approach identifies four areas where sustained action is needed: reduced alcohol consumption; supporting families and communities; positive public attitudes, positive choices; and improved treatment and support. We are making significant progress in implementing the framework and have invested nearly £100 million in prevention, treatment and support services over the last three years. The Alcohol etc (Scotland) Bill, which was introduced to the Scottish Parliament on 25 November 2009, set out the radical legislative measures set out in the framework. Amongst these measures was minimum unit pricing for alcohol, though this was not passed. The bill was passed by MSPs on 10 November 2010 and is a significant step in the battle against Scotland’s unhealthy relationship with alcohol. The Bill will: o Ban quantity discounts such as ‘three for two’ or ’25 per cent off when you buy six’ o Restrict alcohol promotions in off-sales 11 o o Introduce a Challenge 25 age verification scheme for all licensed premises Pave the way for the introduction of a social responsibility levy to ensure those who profit from the sale of alcohol also put something back into the community. Health Promoting Health Service: CEL (2008)14 described 6 actions to promote health in acute care settings, with the aim of ensuring that “every healthcare contact is a health improvement opportunity”. Given the proportionately greater use of acute services by patients from deprived communities, health promotion in acute care settings offers a major opportunity to improve health and reduce health inequalities across the majority of clinical diseases, including cancer. A workshop was held on the Health Promoting Health Service at the NHS Event in June 2010 and drawing on feedback received (as well as from awareness of similar initiatives happening in other parts of the UK); the intention is to produce further guidance on how to use the service to further promote health. The Health Improvement Social Marketing Strategy was launched, along with the 'Take Life On' campaign which covers physical activity, healthy eating, wellbeing and alcohol consumption. A new Chief Scientist Funding Committee (Experimental and Translational Medicine Research Committee) has been established which considers applications aiming to advance and transform scientific knowledge towards a practical clinical use or application and has funded several projects in the area of cancer prevention research. Human Papilloma Virus (HPV) The first two years of the HPV immunisation programme (including a catch up campaign for older girls) has been completed, and from this year the programme is now considered to be part of the routine childhood immunisation programme. The Chief Scientist’s Office has provided over £1 million to fund two large research projects linked to the HPV vaccination programme. Sunbed Legislation Scotland was the first UK country to introduce new legislation on sunbed use which came into force in December 2009. The regulations make it illegal for sunbed operators to allow under 18s to use sunbeds on their premises, to have unsupervised use of sunbeds, bans the sale or hire of sunbeds to under 18s and requires an operator to display a notice on their premises about the health risks of sunbed use. Operators are also now required under law to provide information to customers on the health risks each time they intend to use a sunbed. Occupational Health Occupational health is a reserved matter however, a study looking at the burden of occupational cancers has now been published and is being considered by the Scottish Government Public Health team. Equally Well The Equally Well implementation plan was published in December 2008 and is being jointly progressed with the Early Years Framework and Achieving our Potential. These three social policy frameworks set out the Scottish Government’s approach to tackling inequalities in life chances through targeted action, partnership working and early intervention. These frameworks were published jointly with the Convention of Scottish Local Authorities (COSLA) which has helped ensure that Community Planning Partnerships, which include NHS Boards, prioritise 12 action on the interlinked areas of health inequality, early years and poverty in their Single Outcome Agreements. The Ministerial Task Force reconvened in 2010 to review progress against the three social policies and published a review of the report in June 2010. It confirmed the need to continue to focus on the underlying causes of inequalities in order to deliver long term improvements in outcomes for people. The final report is available at: http://www.scotland.gov.uk/Topics/Health/health/Inequalities/inequalitiestaskforce/ewreview/Q/forceupdate/on. NHS Boards are contributing to reducing health inequalities through the Keep Well and Well North programme of anticipatory care. Community pharmacies offer one mechanism by which the programme of health checks can be delivered and have the flexibility of providing increased access for people. In 2010, an investment of £250k in seven NHS Board areas was made to test nurse and pharmacy led health checks in the Community Pharmacy setting. This has contributed to the delivery of nearly 85,000 Keep Well/Well North health checks to date to 45-64 year olds in the most deprived communities across Scotland. [Correct as of 10/11/10] FUTURE CHALLENGES / THE WAY FORWARD Scottish Government will continue to work to reduce the risks of cancer through a series of evidence-based measures, supported where necessary with legislation, that will tackle identifiable risks, for example: The Tobacco and Primary Medical Services (Scotland) Act 2010 proposes measures designed to stop children from starting to smoke in the first place and will include the introduction of a tobacco display ban. The new measures will be phased in over the next few years commencing in April 2011. To take forward the fundamental change needed to direct our policies around supporting people to achieve and then maintain a healthy weight, a Joint Obesity Group has been established, to oversee the implementation of the Route Map. This group is chaired by the Deputy First Minister (in that capacity) and met for the first time on 26 October. The Group will meet again in January to agree an action plan and key milestones to support delivery of the Route Map. The Action Plan will be published on our website in early 2011. We will continue to implement the Framework for Action on Alcohol and the Alcohol Bill which includes measures both to support those with existing alcohol problems and to prevent future problems arising. NHS Boards are on target to help almost 150,000 people to reduce their drinking by March 2011. Equally Well stressed the requirement for a cross-cutting approach, and health policies clearly have an important role to play in tackling the complexity of health inequalities. All of our major public health challenges – alcohol misuse, smoking, obesity, sexual health and mental health – contribute to health inequalities and the Scottish Government’s actions across all of these areas will therefore help to reduce health inequalities. Ministers have announced the intention to continue and extend the Keep Well/Well North programme from April 2012. A Keep Well Extension Board has been established to oversee the extension programme. An evaluation report of the community pharmacy approach for Keep Well and Well North will be available summer 2011. The report will assess if the approach has managed to reach people who might not make use of GP-based checks and will inform decisions about further use of community pharmacies from April 2012, when Keep Well is to be extended and mainstreamed across NHSScotland. Through the Health Promoting Health Service initiative, we will continue to develop opportunities to support and train healthcare staff to provide information on risk reduction and health improvement at appropriate ‘teachable moments’. 13 EARLY DETECTION (Actions 11-24) KEY AIMS Better Cancer Care recognised that early detection of cancer is crucial and the earlier it can be diagnosed, the better the chance of a positive outcome, for example, in enabling patients to receive high quality care, whether it be with curative or palliative intent. Through earlier detection we aim to continue to improve our overall survival rates for cancer. PROGRESS AND ACHIEVEMENTS AGAINST ACTIONS Screening The Scottish Government is committed to an evidence-based approach to screening, based on the advice of the UK National Screening Committee. Screening programmes for cervical and breast cancer have been established for many years. More recently screening for bowel cancer has been successfully implemented across Scotland. Recent developments in the area of screening include: NHS Health Scotland has published research on the uptake of cervical screening, which is available at: http://www.healthscotland.com/documents/3599.aspx. Following this, NHS Health Scotland and the Scottish Cervical Screening Programme have produced new leaflets providing women with information on the screening test. In August 2010, a variety of new leaflets that target specific groups of women were launched, including leaflets for women who have not attended before and for lesbian and bisexual women. The Scottish Breast Screening Programme staff have been involved in looking at the clinical pathway which women follow if they accept the invitation to go for screening. This included a series of breast screening unit visits and a practical course on improvement methodology. A report and evaluation has been completed and a resource developed for course participants who wish to use the methodology further in their own local units. The implementation of two view mammography was achieved with all screening centres offering two views by the April 2010 deadline. The Scottish Bowel Screening Programme is available in all NHS Boards in Scotland, following the roll out of the NHS Highland pilot in December 2009. Bowel screening is now a mandatory field included in the Keep Well checklist so that anyone eligible for bowel screening will be asked whether they have taken part, as part of their Keep Well check up. In order to increase take-up in more deprived communities, information on bowel screening is provided as part of the Keep Well project. Work is being taken forward involving the screening programmes, NHS Boards, cancer centres and regional networks to ensure timely access to diagnostics and treatment for patients with cancer. An issue that is often raised in ministerial correspondence is the question of testing for prostate cancer, using the prostate specific antigen (PSA) test. In 2009 all GPs were issued with the updated ‘Prostate Cancer Risk Management Pack’ to help primary care practitioners to provide guidance and advice to men who are interested in receiving a PSA test. 14 Ethnicity and medical recording In recognition of the need to address the information gap in relation to ethnicity and medical recording, the Scottish Government Chief Scientist Office has been involved in the ‘Making the Information Desert Bloom’ project, including a retrospective cohort study of five million people linking health and census databases. This will increase our understanding of how cancer affects different ethnic groups and inform our approach to assessing potential ethnic inequalities in cancer. FUTURE CHALLENGES / THE WAY FORWARD We recognise that there is still work to be done to ensure that people are aware of the screening programmes that are available to them. Data on uptake from NHS Information Services Division reveals that overall, bowel screening uptake is still below the target of 60%, while uptake in more deprived areas for the breast and bowel screening programmes is lower than in less deprived areas. A key priority for the delivery of effective screening programmes is, therefore, continued effort to increase informed uptake, particularly amongst minority groups and in deprived areas. A report on phase two of the ‘Making the Information Desert Bloom’ project, which included the cancer aspects of this work, will be published in late 2010 and phase three has now been funded. For cancer, this third phase includes use of primary care data to explore areas of possible inequalities in cancer outcomes. There continues to be a high level of interest in prostate screening, therefore a key challenge going forward will be to communicate a robust message on the balance of risks and benefits associated with PSA tests. 15 GENETIC AND MOLECULAR TESTING FOR CANCER (Actions 25-30) KEY AIMS Special arrangements are required for the identification, risk assessment and testing of individuals who carry inherited genes which predispose them to developing certain cancers. For this reason, one of the aims of Better Cancer Care was to continue to improve genetic services and molecular testing in NHSScotland, including those applicable to cancer. PROGRESS AND ACHIEVEMENTS AGAINST ACTIONS Good progress has been made against the relevant actions outlined in Better Cancer Care including: NHS genetic centres have been provided with resources that have allowed additional consultants, genetic counsellors and laboratory staff along with associated administrative staff to be employed. The additional funding following the Review of Genetics in Relation to Healthcare in Scotland (the ‘Calman’ Review) has enabled a number of initiatives to go ahead in cancer genetics across Scotland, resulting in faster access to genetic testing and consultations, and facilitating coordination between centres. Scottish Government has been working closely with NHS National Education Scotland (NHS NES) and other organisations to improve professional awareness of genetics. A Scottish Clinical Genetics Forum has been established, with a cancer genetics subgroup open to all those working in this field. This enables the different centres to discuss interpretation of management guidelines, and develop new guidance as knowledge increases, ensuring equity of access to services across Scotland. The subgroup has recently incorporated information about breast pathology into the testing guidelines, and is considering widening access to genetic testing for women affected by ovarian cancer, in collaboration with gynaecological oncologists and the laboratories, as the potential for targeted therapy for BRCA carriers nears (mutation of BRCA genes is linked to breast cancer). Increased access to robot technology in the laboratories has helped to reduce the reporting times for BRCA1/BRCA2 testing, with waiting times reduce to under 12 weeks (from over 6 months previously) and increased staffing in the clinical genetics centres has significantly reduced the waiting time for clinic appointments. Collaborative working has also increased, with further development of a joint genetics endocrine clinic in Glasgow, with support from the Dundee molecular laboratory; clinical psychology involvement in the genetics service in Edinburgh, providing support to women coping with difficult decisions surrounding genetic testing or risk reducing mastectomies; and development of an array of Comparative Genomic Hybridisation (CGH) testing of brain tumours between pathology departments and the Edinburgh molecular cytogenetics laboratory. The cancer genetics services are also closely linked to the Scottish Genetic Research Network, and provision of new staff to help with participation in studies is improving recruitment to collaborative cancer genetic studies as well as other types of genetic research across Scotland. Funding has been provided for projects run by the Genetic Interest Group to raise awareness amongst the general population of genetic services. A pilot is currently underway to involve GPs in Grampian and Tayside more closely in the genetic service. Once available the results of this will be reviewed and any positive findings acted upon. 16 Pump-priming funding has been provided for the establishment of ‘Gengage’ which is hosted by the University of Edinburgh. Gengage works to connect people who are involved in raising awareness about genetic conditions and draws together medicine, science and the broader public. A Molecular Pathology Review Group was established and has submitted a report with recommendations on future service provision, which are currently being taken forward by the Scottish Government Health Directorates. Under the auspices of Better Cancer Care, the Chief Scientist Office set up pilot studies in renal and colorectal cancer to examine the issues of relevance for national tissue collection (for cancer and other diseases). Progress has been monitored through a short life working group which is due to report its findings in late 2010. This will cover the issue of how rare or very small samples of tissue should be handled. FUTURE CHALLENGES / THE WAY FORWARD A key focus for this area of work will be to ensure that follow up protocols for high risk individuals remain up to date and evidence-based. The options outlined in the Molecular Pathology Review Group’s report are currently being financially assessed and the outcome will be reported in due course. The findings of the Short Life Working Group on National Tissue Collection will help inform the Chief Scientist Office’s recently established reporting structures for the larger national tissue collection initiative. As this issue also has broad implications for conditions other than cancer, it will be led and reported on via the Chief Scientist Office in the future. 17 REFERRAL AND DIAGNOSIS (Actions 31-39) KEY AIMS A key aim of Scottish Government and NHSScotland is to ensure the prompt and appropriate referral of all patients suspected of having cancer and subsequently, accurate and rapid diagnosis. This must involve encouraging people with symptoms to access services more quickly and effective coordination of care for patients across the boundaries between primary, secondary and tertiary care. PROGRESS AND ACHIEVEMENTS AGAINST ACTIONS Awareness A Scottish Cancer Taskforce (SCT) workshop involving health professionals from various disciplines was held early in 2010 to discuss the actions that can be taken to improve awareness of early cancer signs and symptoms with both members of the public and the clinical community. Full details of this workshop can be found at: http://www.scotland.gov.uk/Topics/Health/health/cancer/ScottishCancerTaskForce/sctworkshop. The SCT is now consolidating this information with a view to progressing a number of actions, including working with the voluntary sector to identify effective approaches to developing health promotion opportunities and working to support wider sharing of GP data and best practice on cancer diagnosis. Referral/Primary Care A Quick Reference Guide to the Scottish Referral Guidelines for Suspected Cancer was published in March 2009, based on the full 1997 guidelines. This easy to use, quick reference booklet was distributed to all GP practices in Scotland to improve symptom awareness. The guidance is available online for members of the public to view at: www.scotland.gov.uk/quickreferenceguide/suspectedcancer. All GPs in Scotland now have access to electronic means of patient referral. Electronic links between referral guidelines and referral systems have been established in all NHS Board areas in Scotland, to ensure that those patients who need to be referred to secondary care are referred appropriately, timeously and with all relevant supporting information. A list of Primary Care Leads for Cancer across all health boards has also been collated and all leads have been invited to join and contribute to the work of the Scottish Primary Care Cancer Group. In 2009-10, a total of £1,450,656 was paid to Scottish Health Boards under the Quality and Outcomes Framework (QOF) for Cancer. In addition, a revised Scottish Enhanced Services Programme (SESP) on cancer was developed and funding made available to Boards from 2009 onwards on an annual basis. Participating NHS Boards use the SESP funding to optimise the primary care of patients referred with the suspicion of cancer and the remedial action taken by their GP thereafter. This includes, where appropriate, the setting up of a register of such patients and a detailed care plan for Out of Hours services. Five Health Boards participated in the Cancer SESP last year. These were, NHS Ayrshire & Arran, NHS Dumfries & Galloway, NHS Forth Valley, NHS Highland and NHS Tayside. The total investment in this area of work amounted to £380k in 2009-10. Waiting times 18 ‘HEAT’ targets around access were developed to support the Scottish Government commitment to increase electronic referrals. An April 2010 audit showed the percentage of electronic referrals (received through the SCI Gateway electronic referral system) to be 94.2%. Cancer managers were surveyed in June 2010 to assess the degree of compliance with electronic submission for suspected cancer referrals, highlighting that NHS Boards have a variety of processes in place and are actively encouraging electronic referral. The Scottish Government’s Improvement and Support team continues to work with NHS Boards around the potential for redesigning referral and investigations pathways so that any pressure points in the patient pathway can be reduced. Regional cancer networks were asked to review high-level pathways in the course of a series of ‘Readiness Check’ on-site visits in autumn 2009, and a Cancer Managers’ Forum has also been established which facilitates the sharing of good practice in pathway work. Positron Emission Tomography Patients who need a PET/CT scan as part of their diagnosis or post treatment can now access this in one of four Scottish centres – Aberdeen, Dundee, Edinburgh and Glasgow. Evidence-based, tumour-specific protocols are in place to ensure that those who will benefit from such a scan are referred. As this is a nationwide service, patients can be offered a scan at any centre if this will speed up their diagnosis. Some of the PET/CT scanners are part-owned and utilised by the universities which allows Scotland to take part in national and international research studies that in time will yield results to help the management of other tumour types, and indeed, other conditions in the future. Regional Progress Across the north of Scotland, a ‘key alarm symptoms’ system has been developed with primary care colleagues to help to identify patients presenting with a suspicion of cancer. In addition, a series of Board-led reviews have been undertaken in the north to look at the provision of locally available diagnostic infrastructures for GP practices. This has included GP endoscopy and GP minor surgery. The Island Boards each link into tumour specific MDTs which helps to identify those patients requiring specialist treatment and where possible, those who can be treated locally. In SCAN, regional integrated diagnostic services for haematological malignancies have been fully developed. FUTURE CHALLENGES / THE WAY FORWARD Awareness raising of cancer symptoms in the general public and clinical community is an area that requires a further combined effort. This will involve exploring the findings from the National Awareness and Early Diagnosis Initiative (NAEDI) which is being taken forward in England to inform work in Scotland, and developing opportunities for collaboration between the Scottish Cancer Coalition and primary care specialists to maintain focus on this area. This is an area that the Scottish Cancer Taskforce will facilitate further work on. Work to explore the potential for redesigning referral and investigations pathways including the use of electronic links will continue with Scottish Government’s Improvement and Support team repeating a round of on-site visits in late 2010. While pro forma-based referrals have been adopted in many specialty and geographical areas, there has been no systematic evaluation of their relative benefits and risks. The Cancer Research Team at the University of Edinburgh Primary Care Division is currently undertaking an evaluation on this and SCT should consider the outcomes from this evaluation. The PET/CT service will be led and further developed by an operational group with representatives from across NHS Scotland. 19 TREATMENT (Actions 40-54) KEY AIMS Better Cancer Care set out our commitment to ensure our services to treat cancer are world-class and that NHS resources are spent in the best way possible to meet the needs of those diagnosed with cancer. PROGRESS AND ACHIEVEMENTS AGAINST ACTIONS Chemotherapy Chief Executive Letter, CEL 17 (2010) Introduction and Availability of Newly Licensed Medicines in the NHS in Scotland was published on 17 May 2010. This guidance provides a framework within which NHS Boards are expected to align their local policies and included within this, is the need for consistency of approach with regard to access to medicines prescribed as part of NHS services provided across clinical networks or for services provided at a regional or national level. NHS Boards have been asked to provide written assurance that substantive progress has been reached in the development of written policies on access to newly licensed medicines by 30 December 2010 and to confirm by 1 April 2011 that policies are in place. Following a national procurement process, the Chemotherapy ePrescribing and Administration System (CEPAS) is being rolled out across NHSScotland. This regionally networked system will support the safe and effective management of patients who either receive all of their care locally or receive some of their care in other Boards. WoSCAN is making good progress to roll out CEPAS across the region and is planning for ‘go live’ in the regional hub in December 2010 ahead of rolling out to 12 satellite chemotherapy units in 2011. SCAN is in the early stages of implementation. NoSCAN currently has stand-alone e-prescribing systems in all of its cancer centres, however, the costs of upgrading and networking NoSCAN’s existing product to the version being implemented in the other Regional Cancer Networks is being assessed. Work has been started to update the existing chemotherapy safety and quality standards with a view to publishing a CEL in 2011 as an update to HDL (2005) 29 Guidance for the Safe Use of Cytotoxic Chemotherapy. The Chemotherapy Advisory Group (CAG) is looking at ways to support the auditing of patients who have died within 30 days of treatment, with a view to determining whether the chemotherapy was appropriate. A national stock take against the recommendations made in the NCEPOD ‘For Better, For Worse’ publication has been undertaken and work is being taken forward by CAG and the Regional Cancer Networks to address the recommendations relevant for Scotland. This includes a piece of work to develop a Best Practice Statement to manage patients with neutropenic sepsis. The Chemotherapy Planning Oncology Resource Tool (C-PORT) has been piloted and an evaluation report is now with the Regional Cancer Networks for consideration of wider adoption according to regional and local priorities. The Scottish Government has created a ‘New Drugs and Technologies’ team, which produces new guidelines to ensure equity of access to newly Scottish Medicines Consortium-approved drugs and to make the process more transparent. Radiotherapy 20 The Scottish Radiotherapy Advisory Group has reviewed the predictions for the radiotherapy service requirements made in the Radiotherapy Activity Planning for Scotland 2011-2015 report and its September meeting focused on looking at how we can maximise centres’ capacity to meet the predicted, rising demand for services with a focus on potential efficiencies across the radiotherapy pathway. Issues around workforce planning and the feasibility of satellite centres were also discussed in workshops at this meeting and a report was presented to the group in November 2010, with recommendations on maximising capacity being accepted by the group. An action plan to detail implementation has been developed. The working arrangements between Scottish Radiotherapy Advisory Group and NHS QIS’ Scottish Health Technologies Group (SHTG) are working well with various topics having been scoped by SHTG in June 2010. SHTG is further examining the evidence base and this work will inform the ongoing National Review of Brachytherapy. In the north, High Dose Rate Brachytherapy has been installed in Aberdeen and Pulse Dose Rate is currently being developed in Dundee as part of a regional shift from Low Dose Rate treatment machines that were in need of replacement. Together, these machines will assure service continuity for the region. Arrangements have been put in place to allow data from the Scottish radiotherapy centres to be sent to the National Cancer Services Analysis Team (NATCANSAT). The collation and sharing of national data will allow benchmarking across Scotland and with England, more effective management of information, and the facilitation of sharing good practice, and should highlight any areas where centres could improve services to patients. Some centres have already started to do this, and others are making progress towards doing so in the near future. Surgery NHS Education for Scotland (NES) has undertaken a review of laparoscopic colorectal surgery and a Clinical Skills Board has been established in Dundee for all laparoscopic surgical techniques, including colorectal surgery. A training course has also been developed. Radical prostatectomy has been highlighted an as area requiring further scoping and this will be considered by the Prostate Cancer Quality Performance Indicator Development Group under the auspices of the National Cancer Quality Steering Group. Sentinel node biopsy is now available across the whole of Scotland, as a result of work undertaken by the RCAGs and their constituent NHS Boards. Research Through the work of the Chief Scientist Office-funded Scottish Cancer Research Network and Clinical Trials Units, over 28% of Scottish Cancer patients are now involved in clinical research. The NHS Research Scotland (NRS) Permissions Coordinating Centre has been established in Aberdeen, which aims to streamline the process for approving research and development proposals. This initiative standardises best practice and removes unnecessary duplication of the governance checks required by Health Boards involved in the same study. The median R&D approval time for multi-centre noncommercial research proposals has been reduced from 46 days prior to the setting up of NRS Permissions CC to the current figure of 16 days. The corresponding figure for commercial studies is a reduction from 21 days to 16 days. 21 FUTURE CHALLENGES / THE WAY FORWARD There will be a challenge to maintain CSO’s commitment to the Scottish cancer research community during a period of financial uncertainty and ensure that Scotland remains at the forefront of oncology research. More widely, we need to ensure that Scotland becomes a key destination for the administration of international cancer trials. Scottish Government’s Quality Division has given its commitment to develop a strategic approach to health technologies assessment. The workforce and financial implications of any new cancer technologies and treatments being introduced to NHSScotland should have the wider economic benefits assessed ahead of implementation. Developing acute oncology services requires a greater focus and service models will be explored within the next year to allow forward planning. Chemotherapy NHS Boards/Regional Cancer Networks will need to decide whether the evaluation of C-PORT fits with their local/regional priorities and, if the virtual tool is to be implemented, put plans in place for this. Managing future demand and escalating costs is a significant challenge for delivery of chemotherapy and one which NHS Boards and Regional Cancer Networks need to continue to focus their efforts in order to maintain safe delivery of services. A national dataset to monitor use of chemotherapy will be developed, the information to inform this audit will be made possible via CEPAS. Radiotherapy The outcomes of the radiotherapy demand and capacity planning work is likely to lead to a bid for additional linear accelerators and other equipment in the next Spending Review. A future challenge will be to support centres to maximise the efficiency and productivity of their current resources safely and this may require new ways of working, including shift some activity from the Central Belt area to free up capacity. This will be done in tandem with the safe and equitable introduction of any newer radiotherapy technologies to Scotland. The scenario planning tool, R-PORT, may need to be evaluated to establish if this will help radiotherapy services plan their capacity in the future. To deliver the national procurement of replacement radiotherapy equipment to time so that the contract is in place by March 2011 will require careful project planning. All radiotherapy centres are either already contributing or working towards contributing to the NATCANSAT dataset for radiotherapy. This will allow benchmarking to be undertaken both between centres delivering radiotherapy both in Scotland and also more widely across the UK. Surgery We know that surgery cures more cases of cancer than any other form of treatment and it is therefore an area that requires a greater focus in the future if surgical outcomes are to be improved upon. SCT will consider this issue in greater detail and will determine how this will be taken forward to maximise both clinical quality, efficiency and patient centred care. 22 LIVING WITH CANCER (Actions 55-65) KEY AIMS SCT’s Living with Cancer Group has been tasked with addressing the support needs of all people living with and beyond a cancer diagnosis. The focus is on improving outcomes post-treatment, while also recognising that good communication, information and support needs to be built in from the start of the pathway. This will require partnership working between healthcare, social care and the voluntary sector. The Living with Cancer Group’s vision for cancer care and support in Scotland is to ensure that ‘people are prepared for the consequences of the diagnosis and treatment of their cancer and are supported to live with it and manage it. Relevant services are empowered and supported to deliver effectively to meet social, physical, emotional, financial, sexual and spiritual, needs’. The group’s work takes a holistic approach and encourages joint working between the health care, social care and voluntary sectors. Wherever possible, the person living with cancer will be supported as the key decision-maker in their care and support. PROGRESS AND ACHIEVEMENTS AGAINST ACTIONS Living with Cancer Action Plan The Living with Cancer Group has a broad and complex remit and the group has taken great care to ensure that it has identified and prioritised areas where the greatest improvements can be made. A Living with Cancer Action Plan has been developed, based on the recommendations from the Group’s vision workshop and incorporating feedback from people directly affected by cancer. The group has identified workstreams to be progressed over the coming year and work is underway to plan and deliver actions that will improve outcomes for people living with cancer, beyond the treatment stage of their journey. Support and Advice A total of £1.6milion (£500k of this under the auspices of Better Cancer Care) has been provided to Macmillan Cancer Care to deliver a range of financial, benefits and employability advice and support initiatives, to ensure that cancer poverty is not a consequence of a cancer diagnosis and to support individuals returning to work during or after treatment. This work has resulted in a total of £6.7million of benefits being paid out to people with cancer as at end June 2010. This initiative includes the successful launch of the Tayside Macmillan Welfare Rights Partnership between Macmillan Cancer Support, NHS Tayside, three local authority partners and Maggie’s Centre to provide a specialist Welfare Rights Team for cancer patients and their families. NHS Grampian, NHS Highland and NHS Western Islands have progressed work around supportive care to patients in their local communities through, for example, nurse-led supportive cancer treatment and follow up services, particularly in prostate and colorectal cancers. In 2008, NHS Grampian opened a Urological Cancer Centre (UCAN) located at Aberdeen Royal Infirmary, which provides treatment advice and ongoing support to urological cancer patients. In NHS Greater Glasgow and Clyde, opportunities have been created for Macmillan Cancer Support representation at senior nursing meetings and a nurse-led long term conditions clinic has been established. A new Macmillan Information and 23 Support Centre opened at the Edinburgh Cancer Centre in December 2009 and the Edinburgh Cancer Centre is also working with Teenage Cancer Trust to develop enhanced services for children and young people living with cancer. Information and communication ‘NHS inform’, the new national health information service, was launched on 3 August 2010. Phase two includes a dedicated cancer zone and a National Strategy Manager and an Information Specialist have been appointed to lead this. They are working with Scotland’s NHS inform Advisory Group to develop cancer-specific information and support services and cancer information partnerships. The National Cancer Information and Support Steering Group’s workstreams have been established to integrate cancer information and support within NHS inform’s three key delivery channels: web, face to face and telephone. As part of its work to develop national quality performance indicators for cancer (QPIs), the National Cancer Quality Steering Group (NCQSG) is developing a set of generic person-centred QPIs which will apply to all tumour types, to ensure consistency and coordination in areas such as patient experience and communication. A set of QPIs for inter-professional communication has already been developed and the NCQSG is now in the process of implementing these. The Long Term Conditions Collaborative, University of Dundee School of Nursing and Midwifery and palliative care representatives, secured NES funding to pilot and evaluate Advanced Communication Skills Training for senior staff. Self Management Better Cancer Care recognised that cancer is increasingly being seen as a long term condition, as more people are surviving and living with the long term consequences of their diagnosis and treatment. Extensive work has been undertaken to raise awareness of self management in long-term conditions, including cancer. The Long Term Conditions Alliance for Scotland has distributed £4million of Scottish Government funding in two rounds of the Self Management Fund to fund 81 projects which aim to build capacity to support self management within the voluntary and community sectors. In addition, funding has been provided to support the use of the CARE measure in a pilot of the Health Inequalities Impact Assessment. Through the Access to Local Information to Support Self management (ALISS) programme, a draft National Health Literacy Framework has been produced and the ALISS "Engine" has been developed and prepared for trial in 2010/11. FUTURE CHALLENGES/THE WAY FORWARD The specific actions agreed by the Living with Cancer Group require further definition by project groups, to identify objectives, measurable outcomes and realistic timeframes. Once this has been achieved, a framework will be drawn up to communicate the Action Plan to partners in healthcare, social care, the voluntary sector and to people living with cancer. 24 This work will involve a significant cultural shift towards a greater emphasis on the individual’s role as the key decision-maker in their care, and towards more effective partnership working amongst healthcare, social care and the voluntary sector. Champions for change will be essential to garner engagement and support for this ambitious approach. Scottish Government will explore potential funding sources with the third sector to support delivery of this work. Economic uncertainty is a significant challenge for this area of work, as services will rightly seek to protect front-line services as much as possible. However, it also presents an opportunity to work in partnership with a wide range of providers to deliver patient centred solutions, within the framework of the NHSScotland Healthcare Quality Strategy. 25 IMPROVING QUALITY OF CARE FOR CANCER PATIENTS (Actions 67-73) KEY AIMS Better Health Better Care set out the basis for NHSScotland’s approach to quality improvement which more recently has been reinforced through the publication of the NHS Healthcare Quality Strategy. The work of the Scottish Government Health Directorates and the SCT needs to focus on how the key areas set out in the NHS Healthcare Quality Strategy will be achieved, these being that care is safe, effective and patient-centred. Timely access is also crucial for someone facing a potential cancer diagnosis (for example, to alleviate concerns and to improve the likelihood of a successful outcome) and this was recognised in Better Cancer Care, which also set out two new waiting times targets that will help to ensure timely access to diagnosis and treatment. PROGRESS AND ACHIEVEMENTS AGAINST ACTIONS National Cancer Quality Programme The National Cancer Quality Steering Group is now well established and has a comprehensive work programme to develop a series of highlevel quality performance indicators (QPIs) that will measure how good a service is and help to identify areas for improvement in the future. Scottish Government is funding a project manager for one year to support this work, based in the West of Scotland Cancer Network. Work is progressing to ensure that all tumour networks take part in national audit, however, this work has proved to be more resource intensive than originally anticipated which means that not all tumour networks will take part in national audits by the end of 2010. Work already undertaken by the National Cancer Quality Steering Group includes: aligning the work plans of NHS Quality Improvement Scotland, Information Services Division and Regional Cancer networks to achieve common goals developing a clear governance framework including how audit results will be published agreeing a sequence in which different tumour groups will have QPIs developed progressing development of tumour-specific QPIs for renal and prostate cancer, with indicators for breast cancer due to begin in late 2010 developing a set of national QPIs for inter-professional communication, as part of the work on generic indicators. Audit resource has been reviewed across NHSScotland and a further review of this resource will be undertaken in 2011. The review highlighted that in many NHS Board areas audit resource is utilised for both clinical audit and for tracking cancer patients to avoid breaches in waiting times. NHS Boards have subsequently been allocated additional resource to avoid these roles being combined, thereby freeing up audit staff to concentrate on improving audit which in turn will help to improve monitoring of outcomes and thereby improve patient care. Cancer Waiting Times A National Cancer Waiting Times Delivery Group has been established to oversee progress against the introduction of the two new cancer access targets. Excellent progress has been made to date and the targets are on schedule to be achieved by December 2011. The 62-day 26 urgent referral to treatment target is being extended to include patients referred via the screening programmes, as well as all patients referred urgently with a suspicion of cancer. The definitions for this target have been agreed and implemented and the first quarterly publication of performance against the new 62-day target (excluding screened positive patients) was made in June 2010 (for Quarter 1 2010). This indicated that the 95% target had been achieved. The data for Quarter 2 was published in September 2010 and showed that 96.6% of patients received treatment within 62 days of urgent referral with suspicion of cancer. Plans are in place to include data on screened positive patients which will be published for the first time in December 2010 (for Quarter 3 2010). Definitions have also been agreed and implemented for the introduction of the new 31-day target, which applies to all patients diagnosed with cancer (whatever their route of referral), from decision to treat to treatment. The first publication of validated 31-day performance was issued in September 2010 (Quarter 2 2010), showing an impressive 97.7% achievement of the target. Improvement work has been taken forward with national screening programmes, NHS Boards, cancer centres and regional networks to ensure timely access to diagnostics and treatment for patients with cancer and to achieve and sustain above target performance. Better Together Patient Experience Programme Better Together is continuing to support three cancer pilots in NHS Scotland (NHS Grampian, NHS Lothian and West of Scotland) to gather the experience of people living with cancer in order to improve experiences using the experience-based design methodology. Each pilot has assumed different foci in terms of both patient characteristics and cancer types. Work in neuro-oncology services in NHS Lothian has led to the development of a transition process from children’s services to adult services and age-appropriate clinics for teenagers and young adults. In WoSCAN, five focus groups, including black minority ethnic (BME) and lesbian, gay, bisexual and transgender (LGBT) community groups and a colorectal patient and carer group, were held to inform a national DVD project. A project examining access to colonoscopy is also underway at Inverclyde, and will be rolled out to Victoria and Gartnavel services. Within Aberdeen Royal Infirmary and Dr Gray’s Hospital in Elgin, a major piece of work was undertaken to survey patients and carers using chemotherapy day services, including staff and patient interviews at both sites. Patient and carer feedback was very positive about caring and compassionate services, providing a catalyst for improvement work. Nationally, two surveys have been conducted to gather the experience of people who have been in hospital and of people using GP services. These surveys will include, but are not confined, to people living with cancer. The GP results were published in July 2010 and the final inpatient results were published on 28 September 2010. A national report has been made available along with reports for individual hospitals and health boards. These include a summary of results for the whole of Scotland as well as relevant comparisons such as by type of hospital, for example, community hospitals. A number of topic reports will also be produced from the survey data. The first one is expected to be published in December 2010 and will address the experiences of people living with long term conditions, including people living with cancer. 27 The voluntary sector has a key role to play in supporting quality improvement and has a number of initiatives in place across the country to achieve this. Opportunities for sharing learning and good practice should be developed. eCASE The quality agenda is supported by efforts to refine systems for collecting and measuring cancer data. WoSCAN and NoSCAN have jointly invested in an IT project to improve the functionality and output of cancer data through eCASE. FUTURE CHALLENGES / THE WAY FORWARD In recognition of the new Quality Strategy, a key area of focus will be to ensure that quality improvement activities are aligned and consistent, with no duplication of effort at national, regional or local levels. Efforts will be made to ensure that good practice examples are shared widely. The National Cancer Quality Steering Group will continue to progress the programme of work to develop quality performance indicators, moving into the next set of tumour groups and evaluating the process used in renal and prostate cancers. The generic indicator programme will be agreed and developed. Further work will need to be undertaken to ensure sustainability of this programme. A further challenge is the development of a sustainable data repository for cancer audit data and the National Cancer Quality Steering Group will investigate this, including, for example, establishing eCase as the mainstream system for data collection. We recognise the need to widen the scope of the new cancer access targets to ensure that they are more inclusive and cover patients diagnosed with cancers other than the nine major cancer types currently used to assess NHS performance. Work to introduce these other cancer types has already started and will be further developed throughout 2011. In the Better Together Programme, work will be undertaken to explore ways to apply the findings of the Scottish Patient Experience programme and cancer pilots more widely within cancer services. The Better Together team will be focussing on supporting NHS Boards to carry out improvement activity in response to the 2010 survey results, and work towards a sustainable long-term approach to experience-based service improvement. 28 DELIVERY (Actions 78-82) KEY AIMS Better Cancer Care outlined over 80 commitments to drive improvements within cancer services across Scotland. It recognised that a strong focus on delivery would be necessary to achieve its intended outcomes. The Scottish Cancer Taskforce (SCT) was established in January 2009 to oversee the implementation of the actions set out in Better Cancer Care and agreed a workplan with its constituent subgroups to progress these actions. PROGRESS AND ACHIEVEMENTS AGAINST ACTIONS Scottish Cancer Taskforce (SCT) The SCT is chaired by Dr Aileen Keel, Deputy Chief Medical Officer, and has representation from NHS Board Chief Executives, NHS Board Directors of Nursing, Regional Cancer Networks, the Scottish Cancer Coalition and policy officials from Scottish Government Health Directorates. Each of the three regional cancer network clinical leads and the Chair of the Scottish Primary Care Cancer Group agreed to take forward specific areas of work and have supported the Deputy Chief Medical Officer in providing strong clinical leadership for the delivery of high quality cancer services. Good progress has been made by each of the sub groups reporting to SCT, and this is communicated via the action notes posted on the Better Cancer Care website and through the SCT’s bi-annual newsletter. Workforce A number of related wider strands of work have been undertaken, for example, the Reshaping the Medical Workforce Project and the four-tier model for radiotherapy. These will help to ensure that the staff groups required to meet the needs of cancer patients in the future will be sustained. As part of the ongoing work around the four-tier model within radiotherapy, funding was provided to NHS Education for Scotland (NES) to support the development of radiography advanced practitioner roles in NHS Scotland. A Force for Improvement: Workforce Framework was published in January 2009 which provided direction, support and cohesion for NHS Boards and their delivery partners in meeting the workforce challenges outlined in Better Health Better Care. While this is clearly not cancer specific, it will impact on the workforce needs required to deliver cancer services in the future. e-Health and Communication Technology A National Clinical Portal Programme has been established with the aim of providing healthcare professionals involved in a patient’s care with electronic access to essential pieces of clinical information. This will make clinical care safer by ensuring that relevant information is available when required for clinical decision making and to support more efficient working processes. Boards are currently working together in three regional consortia to determine their preferred portal solution and associated delivery and implementation processes. In SCAN, a telepresence pilot is being undertaken on behalf of NHS Scotland. This offers new possibilities for remote consultations, which 29 could help to ensure the sustainability of regional oncology services, and for enhancing cancer multidisciplinary meetings. Managed Clinical and Service Networks (MCNs / MSNs) A wide range of developments has been initiated via regional and national MCNs during 2009/10, focussing on improving access, quality and delivery of cancer care. For example, the West of Scotland MCN for colorectal cancer has developed a pathway identifying critical contact points and timescales, which supports planning and improvement in service delivery. In 2009, the National Delivery Plan for Children and Young People's Specialist Services made a commitment that cancer services for children and young people should be organised as only one of two pan-Scotland Managed Service Networks. The Managed Service Network for Children and Young People with Cancer (MSN CYPC) Implementation Group is working towards an April 2011 date for establishment of the MSN. Since 2006, there has been a national MCN, the Children and Teenagers Scottish Cancer Network (CATSCAN), whose priorities have included palliative care, survivorship, teenagers and transition, rehabilitation and education and training, and this will evolve into the Clinical Governance and Quality arm of the MSN. FUTURE CHALLENGES / THE WAY FORWARD In the current financial climate we need to ensure that the work of the SCT continues to act as a catalyst for service improvement and at the same time achieves best value. This will require the development of a structured, realistic work plan which will give a clear direction for NHSScotland and supporting services. We will seek to strengthen the role of the regional cancer networks and encourage collaboration between the regions on a national basis, including flexible working across the Scottish Government Health Departments, the Regional Cancer Networks, NHS Boards and the third sector. The need for financial consolidation presents an opportunity to develop more streamlined approaches to service sharing, particularly in the north of Scotland. We recognise that the continued projected increase in cancer and corresponding increase in prevalence does present real challenges for delivering cancer services in the future. The SCT will analyse the progress to date in delivering Better Cancer Care, as outlined in this report, and identify the gaps and areas which need further consideration and action. The next step will be to undertake a prioritisation exercise and agree these with service providers and users. In all of this, we will ensure that the work of the SCT remains aligned with the aims of the NHS Healthcare Quality Strategy. 30