Overlevelsen hos ældre patienter ≥ 80 år efter isoleret CABG
advertisement
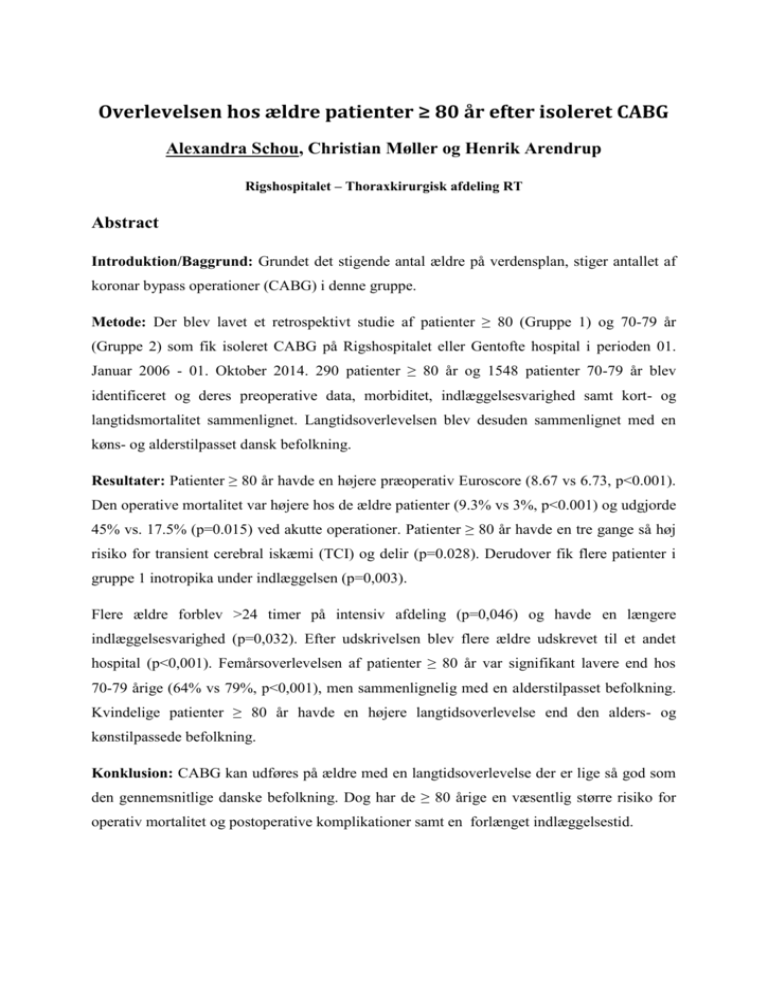
Overlevelsen hos ældre patienter ≥ 80 år efter isoleret CABG Alexandra Schou, Christian Møller og Henrik Arendrup Rigshospitalet – Thoraxkirurgisk afdeling RT Abstract Introduktion/Baggrund: Grundet det stigende antal ældre på verdensplan, stiger antallet af koronar bypass operationer (CABG) i denne gruppe. Metode: Der blev lavet et retrospektivt studie af patienter ≥ 80 (Gruppe 1) og 70-79 år (Gruppe 2) som fik isoleret CABG på Rigshospitalet eller Gentofte hospital i perioden 01. Januar 2006 - 01. Oktober 2014. 290 patienter ≥ 80 år og 1548 patienter 70-79 år blev identificeret og deres preoperative data, morbiditet, indlæggelsesvarighed samt kort- og langtidsmortalitet sammenlignet. Langtidsoverlevelsen blev desuden sammenlignet med en køns- og alderstilpasset dansk befolkning. Resultater: Patienter ≥ 80 år havde en højere præoperativ Euroscore (8.67 vs 6.73, p<0.001). Den operative mortalitet var højere hos de ældre patienter (9.3% vs 3%, p<0.001) og udgjorde 45% vs. 17.5% (p=0.015) ved akutte operationer. Patienter ≥ 80 år havde en tre gange så høj risiko for transient cerebral iskæmi (TCI) og delir (p=0.028). Derudover fik flere patienter i gruppe 1 inotropika under indlæggelsen (p=0,003). Flere ældre forblev >24 timer på intensiv afdeling (p=0,046) og havde en længere indlæggelsesvarighed (p=0,032). Efter udskrivelsen blev flere ældre udskrevet til et andet hospital (p<0,001). Femårsoverlevelsen af patienter ≥ 80 år var signifikant lavere end hos 70-79 årige (64% vs 79%, p<0,001), men sammenlignelig med en alderstilpasset befolkning. Kvindelige patienter ≥ 80 år havde en højere langtidsoverlevelse end den alders- og kønstilpassede befolkning. Konklusion: CABG kan udføres på ældre med en langtidsoverlevelse der er lige så god som den gennemsnitlige danske befolkning. Dog har de ≥ 80 årige en væsentlig større risiko for operativ mortalitet og postoperative komplikationer samt en forlænget indlæggelsestid. Aortic Aneurysms and Trans-apical Endovascular Repair in High Risk Heart Transplant Recipient Khalil Ahmad¹, Kim Terp¹, Vibeke Hjortdal¹ ¹Department of Cardiothoracic and Vascular Surgery & Institute of Clinical Medicine Aarhus University Hospital, Aarhus, Denmark Correspondence to: Khalil Ahmad, MD., Department of Cardiothoracic and Vascular Surgery, Aarhus University Hospital, Brendstrupgårdsvej 100, DK-8200 Aarhus N, Denmark. khahma@rm.dk Ph. + 45 78453064 Fax: +45 78453075 Abstract: Aortic aneurysms cause major morbidities and mortalities. Operative intervention in ascending aneurysms is the treatment of choice although there is the risk of major complications because of technical difficulties, late diagnoses, severely affected hemodynamic condition and organs mal perfusion. Improved survival of heart transplant (HTx) recipients, acceptance of older donors with comorbidities and advances in HTx give rise to new pathological challenges in the cardiovascular field,. Only a few articles have been reported about cardiac and aorta surgery in HTx recipients. We report first trans-apical endovascular ascending aorta repair (EVAR) in a 26-year-old high risk HTx recipient, with mediastinitis and lack of femoral access. She had an uneventful operative and post operative EVAR course. Keywords: Aneurysm, endovascular, Aorta, EVAR Introduction: Aneurysms are caused by atherosclerosis, hypertension, connective tissue disorders ̽¹, and infections.̽². Pseudoaneurysms are formed after rupture of local aortic wall either as a result of trauma or surgical intervention often in suture lines or after puncture. Fifty percent of thoracal aneurysms are caused by atherosclerosis where 45% is seen in ascending 2 aorta, 10% in arcus, 35% in descending aorta and 10% are thoracoabdominal¹. Conventional treatment of ascending aortic aneurysm or dissection is open repair but some patients are too high risk for this approach and may benefit form a less invasive alternative with endovascular aortic repair (1). Anatomical complexities make EVAR difficult resulting in serious complications such as myocardial infarction, paraplegia or paresis, renal failure, stent related complications such as occlusion of the coronary artery, tamponade, distal migration and left ventricular pseudo aneurysms. Case Report: A 26-year-old woman with no previous co-morbidity or risk factors developed uncontrollable idiopathic ventricular fibrillations forth post partum day. She was on cardiopulmonary support (CPS) for a week. Two days after CPS wean, she suffered new events of life-threatening ventricular tachycardia and reinstituted mechanical circulation. Gastrointestinal bleeding was controlled by coiling of colon arteries. After three weeks on CPS, the patient underwent heart transplantation. Post operative period was complicated by mediastinitis, sternum infection, groin wound infection, sepsis, renal failure, pneumonia and respiratory insufficiency. She was treated by multiple surgical interventions for mediastinitis, groin infection, and sudden femoral artery bleeding. After four months, she recovered and was discharged from the hospital. Fifteen months later control CT scan revealed a 45 mm succulent aneurysm close to the right pulmonary artery and superior vena cava (fig.1). The patient was stented in superior vena cava. The aneurysm rapidly enlarged. Due to comorbidities and anatomy open repair approach was considered high risk and the heart team chose using an ascending CMD device. We performed detailed imaging analysis, reviewed CT scans using 3-dimensional imaging software. Aortic branch vessel diameter measurements were obtained at multiple landmarks and length measurements were taken from the highest coronary to the origin of brachiocephalic artery along 3 paths at the greater curvature, central 3 line of flow and the lesser curvature. Ascending CMD-device and endograft made by William Cook Europe (fig 2.) Transfemoral and common carotid artery approach was not possible. We performed the procedure in Hybrid operating room in general anesthesia with transesophageal echocardiography and cardiac perfusion team on stand by to go on CPS using axillary/subclavion approach if necessary. Aortagraphy performed through right brachial artery. We made a small left anterior thoracotomy, followed by pericardiotomy, to expose the left ventricular apex. Heparin was administered. Pursestring sutures were placed on the apex. Left ventricular apex was punctured between 2 horizontal 4-0 prolene using a 14 gauge needle.(fig.3) Afterwards, a guidewire was advanced through the asending aorta and into the arcus aorta under echocardiographic and fluorscopic guidance. Rapid ventricular pacing was performed to minimize pulsatility and movement of the endografts during deployment. Stent graft with 38 ± 1 mm in diameter and 67 ± 2 mm in diameter as determined by preoperative computed tomographic (CT) angiography were then advanced into the ascending aorta over the guidewire and deployed under fluoroscopic and echocardiographic guidance. The apical sutures were secured to achieve hemostasis and finally mini thoracotomy incision was closed. Completion angiogram through right brachial artery was performed to assess coronary and brachiocephalic vessel patency and to rule out endoleak. The procedure was uneventful and the patient was extubated on table.in OP without any complications and she was discharged from hospital on the second. post operative day. CT scans. at 3 month and 9 month reveal no progression.(Fig.4) Discussion: Vascular disease is a problem in heart transplant candidates and recipients. The prevalence is 6% prior to HTx and 12% post transplant (1). Male gender, IHD, corticosteroid use, smoking and improved hemodynamics and ejection fraction post HTx are possible risk factors in the development of vascular disease (2). However, our patient had no history of 4 smoking, hypertension, hypercholesterolemia, or coronary artery disease, and was a young female, Prevalence of post HTx abdominal aortic aneurysms is 2-10% with a rupture rate during follow up of 11-38%, mean aneurysmal expansion rates ranged from 0.78+/- 0,41 cm/yr.(2). Standard treatment of ascending aortic aneurysm is open repair but some patients bear high risks due to comorbidities, anatomical challenges, or multiple previous interventions. Although there has been great innovations in operative techniques, procedural strategies and intensive care management over the last decades, the mortality rate still remains high(3). EVAR is an alternative approach for high risk patients. It has been widely adopted for treatment of descending aortic pathologies whereas its role in treating aortic arch and ascending aortic pathologies remains undefined and limited(4). Generally worldwide experience has been limited by multiple factors including anatomic constraints of the proximal aorta, the lack of devices specifically designed for the ascending aorta and the lack of disease specific stent graft technologies(4). Currently available systems are primarily designed for the descending and abdominal aorta. Vallabhajosyula et al reported a transapical approach to seal the leak in two cases of aortic pseudoaneurysm with zero 30 days mortality and no coronary artery or stent graft related complications. Several studies have reported safety and effectiveness of EVAR of the descending aorta but the role of EVAR for treating ascending aorta pathology is less well known. The size, shape, hemodynamic forces, proximity to other vital structures make ascending aorta challenging and difficult to EVAR. Currently available stent grafts do not fully address the unique features of ascending aortic anatomy (5). The ascending aorta is typically broader in diameter than the descending aorta and because it is a curved structure, there is a significant difference in length along the greater and lesser curves. 5 Conclusion: Endovascular repair of ascending aorta is technically possible and can be performed in selected high risk patients included heart transplant recipient with good result. The ascending aortic endografts are inadequately designed and until improved technology is available only the patients at highest or prohibitive risks should undergo EVAR. Better results may be achieved with an improved design of ascending aorta specific devices and delivery systems. There is a need for further research and experience regarding this topic Acknowledgements: The authors thank William Cook Europe for drawing and providing the ascending-CMD-device. Disclosure: The authors declare no sources of funding or conflicts of interest in the manufacture and distribution of the device. ¹ Vibeke E. Hjortdal et all. Thorax Kirurgi 2, Fadl´s Forlag 2008 ̽¹e.g. marfans syndrome, Ehler-Danlos, morbus Erdheim ̽² mycotic aneurysms References: 1. Takayama H. et al. Characteristics of extracoronary vascular disease in heart tranplant recipient. J. Card Surg. 2008 2. Dasari T et al. Abdominal aortic aneurysms (AAA) post heart transplantation: a systematic review of literature. Ann Transplant. 2011 3. Koyu tanaka et al. Hybrid Treatment for Type A Acute Aortic Dissection with Multiorgan Malperfusion. Ann Thorac Surg 2012 4. Prashanth Vallabhahosyula et al. Endovascular repair of the ascending aorta in patients at high risk for open repair. J Thoracic and cardiovasc surg 2014 5. Eric E. Roselli et al. Endovascular stent grafting for ascending aorta repair in high risk patients. J Thoracic and cardiovasc surg 2015 6 Predicting new-onset of postoperative atrial fibrillation in patients undergoing cardiac surgery using semi-automatic reading of perioperative ECGs. Gu J a,b,c, Graff C d, Melgaard J d, Lundbye-Christensen S e, Schmidt EB b, Torp-Pedersen C b, Thorsteinsson K a,b, Andreasen JJ a,b a Department of Cardiothoracic Surgery, Aalborg University Hospital, 9100 Aalborg, Denmark; b Department of Clinical Medicine, Aalborg University, 9100 Aalborg, Denmark ; c Department of Cardiovascular Surgery, Heart Centre of General Hospital, Ningxia Medical University, 750004 Yinchuan, Ningxia, PR China; d Department of Health Science and Technology, Aalborg University, 9100 Aalborg, Denmark ; e Unit of Clinical Biostatistics and Bioinformatics, Aalborg University Hospital, 9100 Aalborg, Denmark; Abstract Background: Postoperative new onset atrial fibrillation (POAF) is the most common arrhythmia after cardiac surgery. The aim of study was to evaluate if semi-automatic readings of perioperative ECGs is of anyvalue in predicting POAF after cardiac surgery. Methods: This is a retrospective observational study. A total of 100 patients who underwent cardiac surgery at our institution between January 1,2010 and December 31, 2014 were included. POAF was defined as new onset atrial fibrillation requiring treatment, documented by electrocardiography (ECG) or continuous ECG monitoring. A semi-automatic machine capable of reading different parameters of digitalized ECG’s was used to read both lead 7 specific (P/QRS/T amplitudes/intervals) and global measurements (P-duration/QRSduration/PR-interval/QT/Heart Rate/hypertrophy). Results: We divided the patients into two groups: 50 consecutive patients with POAF and 50 patients who did not develop POAF (NOPOAF). There were 72% and 66% males in the POAF and NOPOAF group, respectively. The median age was 69,8±9.56 years and 65,5±10,34 years in each group. The types of operation in each group included coronary artery bypass grafting (CABG) (70%,58%) and valve surgery (30%,42%), respectively. The only measurements which consistently showed a difference between POAF and NOPOAF were: P-duration, PR-interval, QRS-duration and left atrial enlargement (LAE). POAF versus NOPOAF (milliseconds & z-score): P-duration (127 vs 120 & 1.92 vs 1.26, p=<0.05), PRinterval (198 vs 179 & 1.67 vs 1.28, p=<0.05), QRS-duration (127 vs 115 & 3.96 vs 2.62, p=<0.05), LAE (28 subjects versus 9 subjects, p<0.05). Their z-scores are meaning that the means of the 50 patients would be standard deviations from the mean of a normal healthy population. All other measurements did not indicate a difference between the two groups. Conclusion: Semi-automatic readings of digitalized perioperative ECGs showed differences regarding the P-duration, PR-interval, QRS-duration and signs of LAE between patients who develop and patients who do not develop POAF following cardiac surgery with higher values in the POAF group. These results indicate that POAF may be linked to slow propagation during depolarization. It may occur if the heart is hypertrophied or if there is slow conduction through the specialized conduction system. Prediction of POAF should focus on assessing delayed propagation in the atria, possibly a combination of ECHO and ECG. 8 Longevity and admission to nursing home according to age after isolated coronary artery bypass surgery: A nationwide cohort study Kristinn Thorsteinsson 1,2, Jan Jesper Andreasen 1,2, Rikke Nørmark Mortensen3, Kristian Kragholm4, Christian Torp-Pedersen3,5 , Gunnar Gislason 6, Lars Køber7, Kirsten Fonager 5,8 1 Department of Cardiothoracic Surgery, Aalborg University Hospital, Aalborg, Denmark 2 Department of Clinical Medicine, Aalborg University, Aalborg, Denmark 3 Department of Clinical Epidemiology, Aalborg University Hospital, Aalborg, Denmark 4 Department of Anesthesiology and Intensive Care Medicine, Aalborg University Hospital, Aalborg, Denmark 5 Department of Health Science and Technology, Faculty of Medicine, Aalborg University, Aalborg, Denmark 6 Department of Cardiology, Copenhagen University Hospital, Gentofte, Denmark 7 Department of Cardiology, Copenhagen University Hospital, Rigshospitalet, Copenhagen, Denmark 8 Department of Social Medicine, Aalborg University Hospital, Aalborg, Denmark E-mail Kristinn.Thorsteinsson@rn.dk Background: Data on nursing home admission in patients >80 years of age after isolated coronary artery bypass grafting (CABG) are scarce. The purpose of this study was to evaluate longevity and admission to nursing home according to age in a nationwide CABG cohort. 9 Methods: All patients who underwent isolated CABG in1996-2012 in Denmark were included. Patients were identified through nationwide administrative registers. The cumulative incidence of admission to a nursing home was estimated. A cause specific Coxregression model was constructed to identify predictors for living in a nursing home one year after CABG. Kaplan-Meier estimates were used for survival analysis. Results: A total of 38,487 patients were included (1,455 >80 years). Median age was 65.4 ± 9.5 years. Males comprised 80%. 30-day mortality was 2.8%, increasing with age (1.2% in patients < 60 years and 7.6% in patients >80 years. Mortality at 1 year was 2.2% and 13.9% among patients with an age <60 and >80 years, respectively. Proportion of patients admitted to a nursing homes at 1, 5 and 10 years after surgery was e.g. 0.1%, 0.2% and 0.9% (<60 years), 1.5%, 7.7% and 17% (>80 years), respectively. Main predictors for living in a nursing home one year after surgery were: age >80 years (HR 16.70, 95% CI 6.94-40.20), female sex (HR 1.66, 95% CI 1.11-2.5), Heart failure (HR 1.59, 95% CI 1.03-2.40), previous myocardial infarction (HR 2.07, 95% CI 1.33-3.20), previous stroke (HR 2.21, 95% CI 1.42-3.40), stroke < days after surgery ( HR 11.00, 95% CI 6.81-17.80). Neither urgent nor emergent surgeries were significant predictors for living in a nursery home 1 year after surgery. Conclusion: Elderly patients are able to stay in their homes for many years after CABG. The risk of nursing home admission is small and is dependent on the patient’s preoperative comorbidities. Jeg har vedhæftet nogle af kurverne og figurerne jeg kommer til med at bruge i artiklen Overlevelse efter 1 år 10 11 Cummulative incidens Plejehjem efter 1 år Cummulative incidens plejehjem med followup i op til 17 år. Mean followup tid 10 år 12 Patient journey for 1 år post op (farverne skal ændres ) 13 Patient journey for 10 år post op 14 Fixation of Sternal Fracture Using Absorbable Plating System, Three years follow up Khalil Ahmad¹, Niels Katballe¹, Hans Pilegaard¹ Department of Cardiothoracic and Vascular Surgery & Institute of Clinical Medicine Aarhus University Hospital, Aarhus, Denmark Correspondence to: Khalil Ahmad, MD., Department of Cardiothoracic and Vascular Surgery, Aarhus University Hospital, Brendstrupgårdsvej 100, DK-8200 Aarhus N, Denmark. khahma@rm.dk Ph. + 45 78453064 Fax: +45 78453075 Abstract: Sternal fractures occur due to severe chest wall trauma in a small number of patients. They are often conservatively treated. The surgical intervention, although controversial, is indicated in case of deformity, severe pain, and ventilatory complications(1). We report the first case where absorbable plate has been used to fix a traumatic fracture in a 42-years-old female. After 3 years, the patient is still free of symptoms and CT scanning reveals intact sternal bone structure. Keywords: Sternum, Fracture, Fixation, Lactosorb, 15 Introduction: Sternal fractures which account for approximately 3% to 8% of all recorded fractures(1,2,3), occur in patients facing major blunt anterior chest trauma, quite often due to car accidents, or direct high energy trauma to the front of chest. An indirect trauma from flexion compression of the spine or head injuries, can result in severe unstable fractures of the sternum or multiple thoracic compression fractures The lateral plain chest radiographs can reveal unstable fractures¹. The diagnoses of sternal fractures (specially small lineal fractures) can be difficult in anterioposterior chest x-rays, Computed tomography (CT) is more accurate to make the diagnosis and describe the morphology of the sternal fractures. CT scan may reveal associated intrathoracic injuries such as myocardial contusion, cardiac rupture, aortic dissection, pulmonary contusion, flail chest, rib and columna fractures. Usually sternal fractures are treated conservatively. Surgical correction should be considered in case of deformity, loss of sternal continuity, overlap, mobility of sternum, and presence of intractable pain(3) Case report: A 42-year-old woman was referred to our department after she had slipped from a 5 meter high ladder falling direct on her anterior chest. She had severe pain and deformity of the sternum. CT scanning revealed a displaced 4th transverse ridge fracture of corpus sternum where the upper fragment slipped behind the lower part without any ribs or vertebral column injuries(fig.1 and 2). The fracture was fixed by using an absorbable plate - Lactosorb® (42mm x 42mm large, 10 x 10 hole, 1,14 mm thick, fixed by 6 Lactosorb screws 11 mm long and 2 mm width). We performed a short midline longitudinal incision over the sternum and cleaned the site from hematoma to expose healthy bone without shortening sternum. We used two bone reduction forceps placed within the surrounding intercostal spaces to assist manual reduction of the fracture. The heated lactosorb plate was shortened longitudinally and contoured manually to the underlying sternum and secured using 3 self drilling, self-tapping 16 lactosorb screws on each side(Fig. 4a & 4b). A hot plate is soft but becomes hard in a few seconds when cooled at room temperature. We chose six (11 mm x 2 mm ) lactosorb screws as that was the thickness of the sternum measured on CT. We drilled with hand drill using adjustable stop bone tap. The tap was set to 11 mm to avoid deeper insertion. The wound was irrigated, a handy-vac drainage system was placed and incision was closed. The plate was only 1.14 mm thick and therefore was not visible or palpable under the skin. The handy-vac drainage system was removed 1.st post operative day. The patient was discharged from the hospital the 2nd post operative day and returned to her work as physiotherapist after 3 weeks. CT –scan 3 years later revealed complete healing of the fracture (Fig 3a & 3b). Discussion: Operative fixation of the sternal fractures was first described by Mckim in 1943(3). He used a Kirschner wire. Several surgical techniques have been described during the past seven decades such as wires, nylon bands, Mersilene tape and locking plates. The most common stabilisation method is to use locking plates. In Ergene G. et al studies indications for surgery were severe pain, dislocation with overlapping of sternal edges and thoracic wall instability(1). No major intra-or postoperative complication has been reported in the studies(2). Only a few articles have been published about surgical fixation of the sternum(3). A minority of sternal fractures require steosynthesis. Lactosorb is a resorbable poly-L-lactic acid/polyglycolic acid copolymer, which provides desirable strength, comparable to that of titanium plating and it retains approximately 70% of its strength at eight weeks(4). Kessler KJ et al used Lactosorb plates for rotator cuff repair in 45 patients with excellent postoperative result. Lactosorb plate maintained its strength during the healing period of the repair(5). Pat Ricalde et al compared the strength of 6 different resorbable plating systems using an in vitro model before and after heating them. Lactosorb performed the best with regard to the force required to cause a clinically significant displacement of 1 to 2 mm. He estimated the resorption time to be less 17 than 1 year(6) Riitta Suuronen et.al performed mandibular osteotomies in sheep, and fixed them either with bioabsorbable poly-L-lactide or metallic dynamic compression plates. During the follow up period of about 6 months, radiolographical, histological and microradiographical examinations at 6, 12, 24 weeks were performed. It has been shown that bony union with callus formation was accomplished by 6 weeks without any sign of plate failure. Lactosorb has a predictable resorption within 12-18 months(7), It has a low incidence of inflammatory and allergic reactions. Primarily, lactosorb has been used in maxillofacial surgery. Our department has used it to fix sternum after osteotomy² in more than 150 pectus carinatum repair with excellent result. We experienced no operative or post operative complications. There has been no mortality, intensive admissions, plate failure, infection, pseudoarthroses or chronic pain.. The hospital stay was about 2-3 days. Mollaoglu N et al investigated the early tissue response to titanium and LactoSorb screws and found that both materials can be used safely. The biodegradation of LactoSorb screws was not completed by the end of day 60. LactoSorb and titanium miniplates and screws are well tolerated and induced bone formation without causing adverse tissue response(8,9) Transverse metal plating systems may be dangerous when rapid sternal entry is required. By using resorbable plates instead of metallic systems one may reduce operations time, shorten hospital stay, sickness leave, provide better cosmetic results and avoid a second operation for removal of the implanted system, which may cause additional pain, discomfort and further complications. Conclusion: Absorbable plates may be considered in fixation of traumatic sternal fractures as they have low incidence of failure, inflammation, and allergic reactions They promote osteogenesis, and reduce the operation time, We report surgical fixation of a traumatic transverse sternal fracture using absorbable plate with an uneventful course. Sternal fixation with absorbable plates may require further investigation. 18 Acknowledgements: The authors thank prof. Vibeke Hjortdal, associate prof Thomas D. Christensen for editorial and advisory assistance and Ninna Madsen for providing 3-D CT scan. Disclosure: The authors declare no sources of funding or conflicts of interest in the manufacture and distribution of the device. ¹a break in continuity of bone caused by high force ² a surgical cut in bone to repair a deformity References: 1: Ergene G1 et al. Sternal fixation with nonspecific plate. Ann Thorac Cardiovasc Surg. 2013;19(5) 2: Chou SS et al. Use of SternaLock plating system in acute treatment of unstable traumatic sternal fractures.Ann Thorac Surg. 2011 Feb;91(2):597-9. 3: Stefan Schulz-Drost et al. Surgical fixation of sternal fractures: locked plate fixation by low-profile titanium plates—surgical safety through depth limited drilling Int orthop. 2014, jan 38(1); 135-139 4: Chou SS1 et al. Use of SternaLock plating system in acute treatment of unstable traumatic sternal fractures. Ann Thorac Surg. 2011 Feb;91(2) 5: Kessler KJ et al. LactoSorb plates for rotator cuff repair. Arthroscopy. 2002 Mar;18(3):279-83. 6: Pat Ricalde et al. Strength Analysis of 6 Resorbable Implant Systems: Does Heating Affect the Stress-Strain Curve? J Oral Maxillofac Surg 66:2493-2497, 2008 7: Riitta Suuronen et al. Comparison of absorbable self-reinforced multilayer poly-1-lactide and metallic plates for the fixation of mandibular body osteotomies: An experimental study in sheep. J Craniofac Surg, 23 (2012), Volume 50, Issue 3, Pages 209-317 (March 1992) 8.Mollaoglu N1, et al. The early tissue response to titanium and LactoSorb screws.Dent Traumatol. 2003 Jun;19(3) 9: Wiltfang J1, et al. Biodegradable miniplates (LactoSorb): long-term results in infant minipigs and clinical results. J Craniofac Surg. 2000 May;11(3) 19 A Novel Device for Accurate Chest Tube Insertion – A Randomized Controlled Trial Abstract Background: It is recommended that the tip of the chest tube is positioned apically in pneumothorax and basally for fluids. However, targeted positioning of a chest tube to a specific part of the pleural cavity can be a challenge. Methods: A new medical device (KatGuide) was developed for optimizing accurate large bore chest tube positioning. The primary endpoint of this study was to compare the KatGuide method with the conventional method for chest tube insertion regarding targeted positioning of the chest tube. Patients with pneumothorax, hemothorax, hydrothorax, chylothorax or empyema were randomised for chest tube insertion (28 French) by the KatGuide method or conventional surgical thoracostomy (forceps method). Results: A total of 109 patients were enrolled (KatGuide n=49; conventional n=60). In the KatGuide-group 41 (84%) were optimally positioned versus 32 (53%) in the conventional group (p=0.001). Experienced surgeons (>50 chest tube insertions) inserted 39 chest tubes. In the KatGuide group 15/17 (88%) were optimally positioned versus 11/22 (50%) in the conventional group (p=0.02). In patients with factors impeding insertion (n=25) 92% were well placed in the KatGuide group versus 54% in the conventional group (p=0.05). In the KatGuide group 2 chest tubes (4%) were misplaced versus 11 (18%) in the conventional group (p=0.04). Conclusions: A novel chest tube insertion device significantly improves the position of the chest tube. (ClinicalTrial.gov – Trial Registration Number: NCT01522885) Corresponding author: Niels Katballe. Department of Cardiothoracic and Vascular Surgery, Aarhus University Hospital, Brendstrupgaardsvej 100, DK - 8200 Aarhus N, Denmark. Tel: +45 61683931; e-mail: katballe@dadlnet.dk 20 21