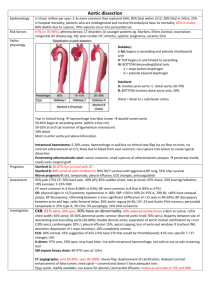
Acute Aortic Dissection
advertisement
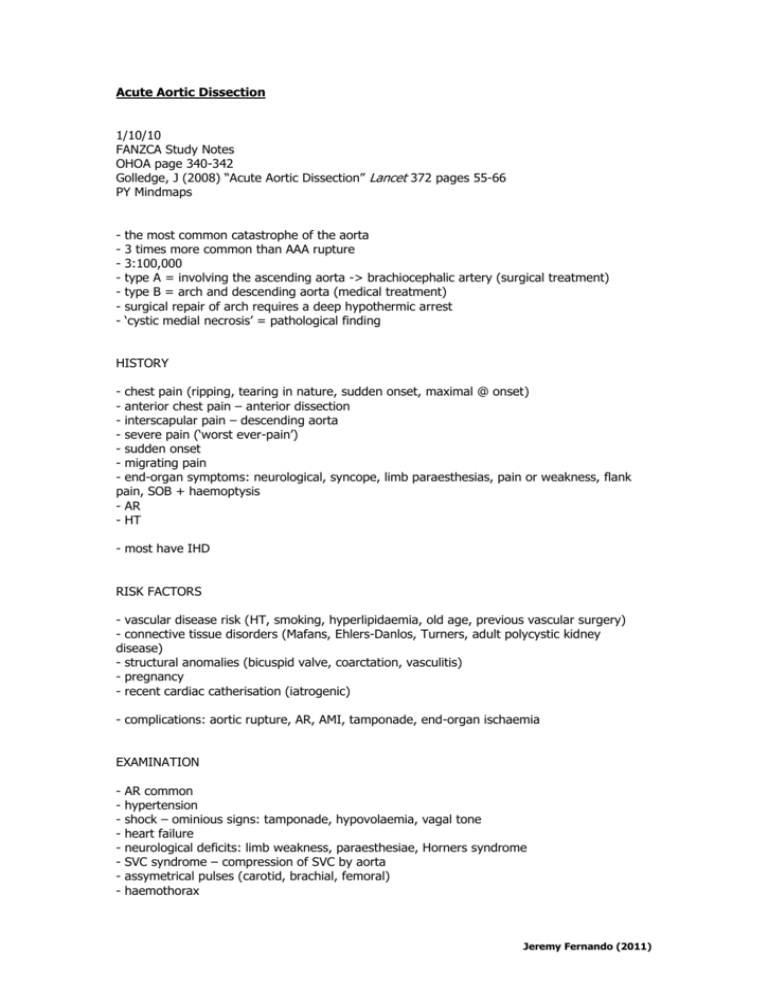
Acute Aortic Dissection 1/10/10 FANZCA Study Notes OHOA page 340-342 Golledge, J (2008) “Acute Aortic Dissection” Lancet 372 pages 55-66 PY Mindmaps - the most common catastrophe of the aorta 3 times more common than AAA rupture 3:100,000 type A = involving the ascending aorta -> brachiocephalic artery (surgical treatment) type B = arch and descending aorta (medical treatment) surgical repair of arch requires a deep hypothermic arrest ‘cystic medial necrosis’ = pathological finding HISTORY - chest pain (ripping, tearing in nature, sudden onset, maximal @ onset) - anterior chest pain – anterior dissection - interscapular pain – descending aorta - severe pain (‘worst ever-pain’) - sudden onset - migrating pain - end-organ symptoms: neurological, syncope, limb paraesthesias, pain or weakness, flank pain, SOB + haemoptysis - AR - HT - most have IHD RISK FACTORS - vascular disease risk (HT, smoking, hyperlipidaemia, old age, previous vascular surgery) - connective tissue disorders (Mafans, Ehlers-Danlos, Turners, adult polycystic kidney disease) - structural anomalies (bicuspid valve, coarctation, vasculitis) - pregnancy - recent cardiac catherisation (iatrogenic) - complications: aortic rupture, AR, AMI, tamponade, end-organ ischaemia EXAMINATION - AR common hypertension shock – ominious signs: tamponade, hypovolaemia, vagal tone heart failure neurological deficits: limb weakness, paraesthesiae, Horners syndrome SVC syndrome – compression of SVC by aorta assymetrical pulses (carotid, brachial, femoral) haemothorax Jeremy Fernando (2011) INVESTIGATIONS - leukocytosis - Cr elevation with renal artery involvement - TNT elevated if dissection causes myocardial ischaemia - D-dimer – if negative very unlikely - X-match - CXR: widened mediastinum (60%), abnormal aortic contour (50%), normal - ECG: normal, inferior ST elevation c/o right coronary dissection - work currently being done on biological markers (elastin fragments, d-dimer, smooth muscle myosin heavy-chain protein) - TTE: good for AR and tamponade - TOE: upper ascending aorta and arch not well visualised - CT aortogram - MRI CT vs TOE vs MRI vs Aortogram Advantages Disadvantages CT - easy availability in emergencies - high sensitivity and specificity - assess complications (ischaemic gut, tamponade, dissection or aorta) - easier to monitor vs MRI - quicker than MRI - remote location iodinated contrast can’t assess AR, LVF or coronaries radiation exposure TOE - bedside - can detect intimal flap, true and false lumen, AR, tamponade - can assess LV function - no contrast needed - semi-invasive may need anaesthesia/intubation may cause hypertension not widely available special expertise required oesophageal trauma doesn’t quantify distal complicat. MRI - - not readily available - inconvenient (> 30 min) - limited access and monitoring - limited applic. (claustrophobia, pacemakers) Aortography - detection of intimal flap and AR - assess LV function, tamponade, blocked coronaries) high sensitivity and specificity Gadolinium contrast better safety profile can detect AR no radiation exposure cardiac MRI could also be performed - not readily available invasive contrast load remote location CLASSIFICATION Stanford A – ascending aorta affected B – ascending aorta not affected De Bakey Jeremy Fernando (2011) 1 – entire aorta affected 2 – confined to the ascending aorta 3 – descending aorta affected distal to subclavian artery Svensson 1 2 3 4 5 – – – – – classic dissection with true and false lumen intramural haematoma or haemorrhage subtle dissection without haematoma atherosclerotic penetrating ulcer iatrogenic or traumatic dissection MANAGEMENT - emergency priorities: (1) control BP (2) control bleeding (3) fluid resuscitation - type A – surgery, type B – medical unless evidence of rupture, end-organ ischaemia, uncontrollable HT (?endoluminal repair) - O2 - wide bore IV access (Swan sheath) - invasive monitoring - warn blood bank (x-match 6U + need for other products) - control HR and BP (aim for P 60-80 and BP 100-120 SBP) - vasodilators (GTN, labetalol, hydralazine, SNP) - call cardiothoracic surgeon INTRAOPERATIVE - avoid hypertension on induction fast, full and forward dissection and clamps may interfere with arterial monitoring TXA2 femoral arterial cannulation used for bypass anticoagulate before bypass if aortic root involved then patient may need AVR with coronary artery reimplantation monitor BP after bypass closely may have dissected into other organs (monitor function) Circulatory Arrest - deep hypothermic arrest (DHA) required during arch surgery as it isn’t possible to perfuse cerebral vessels on bypass - safe duration = 45min @ 18 C - other ways of protecting brain; pack head with ice, thiopentone, methylprednisonlone mannitol, GTN (to prevent vasoconstriction) - POCD proportional to DHA time - once circulation arrested -> all infusion and pumps stopped - when warming do not set FAW to >10 C (prevents burns), start propofol and fix coagulopathy with products Jeremy Fernando (2011) POST-OPERATIVE CARE - standard care Jeremy Fernando (2011)