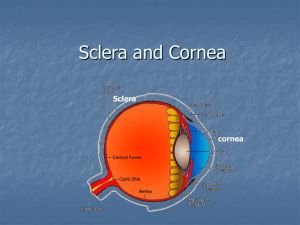
Sclera
advertisement

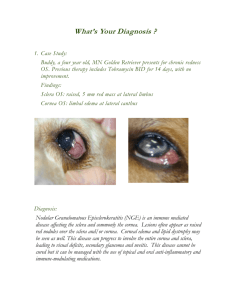
Sclera Function The sclera maintains the shape of the major portion of the eyeball and provides an attachment for the extraocular muscles which move the eye. As a part of the tough fibrous tunic, the sclera also serves as a protective function for the more delicate inner contents of the eye. Anatomy General o The scleral forms the posterior 5/6 of the fibrous tunic, extending from the limbus to the optic nerve. o It is made of a dense collagenous connective tissue. o It is covered by Tenon’s Capsule, also known as the Fascia of Tenon. This is a tough, fibroelastic layer between the sclera and soft, fatty tissue of the orbit. It extends from the limbus to the optic nerve, attaching to the extraocular muscles. It serves as insulation for the sclera and fatty tissue. Since Tenon’s capsule is not firmly attached to sclera, some movement still occurs. With ennucleation, when the eye is extracted and replaced with a prosthetisis, Tenon’s capsule is left in place so that the eye can have normal movements. Thickness o Thickest at posterior pole (1mm) o Thinnest where the extraocular muscles attach (0.3mm) With the muscle, the thickness is 0.6mm. Foramina o Anterior Foramen This is a potential space since it is filled in by the cornea. o Posterior Foramen This is the opening through which the optic nerve passes. It is the larger of the two foramina. It is funnel shaped in cross section. Dimension Anterior- 1.5-2.0mm Posterior- 3.0-3.5mm The anterior scleral foramen axis is generally horizontal. The posterior scleral foramen axis is generally vertical. Lamina Cribosa These are fibers traversing the posterior scleral foramen. The retinal axons pass through this. Because it is covered with tissue, it is difficult to see with direct ophthalmoscopy. It is the weakest spot of sclera. It can bulge posteriorally with increased IOP. This is a characteristic sign of glaucoma. Sulci o o Because of the different curvatures of the cornea and scleral in the fibrous tunic, an external sulcus occurs at the corneoscleral junction. This is the external scleral sulcus. The indentation is not observable on a patient because it is filled with conjunctival tissue. On the corresponding inner surface at the corneoscleral junction, the tissues are scooped out to form the internal scleral sulcus. The contents include the trabecular meshwork and scleral spur. Trabecular meshwork This is the area of the eye through which the aqueous humor drains. Scleral spur This is an area of denser scleral tissue. The posterior margin of the internal scleral sulcus projects forward into the interior of the eye, forming the scleral spur. It forms a ring around the eye and serves as the point of attachment of the ciliary body. This means that it is very secure and does not move. It is a gonioscopy landmark. Pectinate fibers (Iris Processes)- bridge iris to the meshwork. o Layers o Episclera This is the most external layer of the sclera. It is composed of loose connective tissue. Compared to the cornea, the collagen bundles are smaller and more widely and irregularly spaced, therefore looser. The deeper layers get tighter and merge into the sclera proper. Tenon’s capsule covers this and is loosely connected to it. The episclera is highly vascular, especially near EOM attachment. Ciliary injection o When the blood vessels in the anterior episclera become inflamed and enlarged, redness will be seen all around the eye. o To differentiate between conjunctiva and episclera inflammation, rub the conjunctiva with cotton swabs while looking through slit lamp. If the vessels move, they are in the conjunctiva. o Sclera Proper, aka Substantia Propria This is the thickest portion of the sclera, consisting of 65% water. This area is a dense, irregular connective tissue. The size of the bundles of collagen larger is more variable, generally 10 microns thick and 100-400 microns wide. Since some intertwining occurs, the lamellar arrangement is lost, causing some opacification. The fibers are arranged concentrically around the posterior foramen, the optic nerve. They are convex in shape. There is some viscoelasticity and stretch present due to the looping arrangement. This is to withstand tension of where muscles pull. There are less fibroblasts here in comparison to the cornea. Melanocytes are also present in the sclera. These are derived from the pigment cells from the layer below the sclera obtained during development. Although there is a small chance that this could indicate a melanoma, it is generally not a problem. People of darker complexion generally have more localized areas of melanocytes. o Lamina Fusca This is the thinnest and innermost layer of the sclera. It is modified stromal tissue with smaller bundles that branch more. It is very darkly pigmented due to the numerous melanocytes. It blends with the uvea due to the color. This layer of the sclera is separated from the external surface of the choroid by a potential space, called the perichoroidal space. This space allows the passage of nerves and arteries. Histology o Cleaved off the epithelium and endothelium when they end at the limbus, only the stroma of the cornea continues into the sclera. Here the collagen fibers of the cornea become the collagen fibers of the sclera, but major differences earlier described distinguish the two. Emissaria o A number of channels called intrascleral canals or emissaria exists in the sclera for the passage of nerves and blood vessels into the interior of the globe. These emissaria are broken down into anterior, middle, and posterior emissaria. o Anterior Emissaria The anterior emissaria are located near the limbus. The venous branches contain the intrascleral venous plexus that drains to the episcleral venous plexus. This can be seen with the slit lamp. The arteriol branches contain the anterior ciliary arteries that supply blood to the ciliary body and superficial marginal plexus. o Middle Emissaria The middle emissaria are located 4mm behind the equator, one in each quadrant. These contain the vortex veins. This is the major drainage out of the eye. o Posterior Emissaria The posterior emissaria are located at the back of the eye around the optic nerve. They carry the long posterior ciliary arteries and nerves which run towards front of eye and slip in between sclera and choroid, as well as the short posterior ciliary arteries and nerves. Blood Supply o Because of the collagen structure of the sclera, it is relatively avascular. o Principal blood supply Anterior ciliary arteries Short posterior ciliary arteries Episclera Choroid Nerve o The posterior sclera is supplied by short posterior ciliary nerves which pierce the sclera around the optic nerve. o The anterior sclera receives branches from the ciliary plexus in the area of the limbus. Pathology Episcleritis General o There are two types: Simple and Nodular Simple is more common and shorter duration Nodular is elevated and more localized. It is slightly more likely to have etiology with projected course. Lasts 3-4 weeks. o Occurs often in young adults, late teens to early 40s. o Females affected twice as often as men o Rapid onset (within hours to one day) o 90% misdiagnosed o Redness in bulbar more than palpebral conjunctiva. Profile o Young female with sudden onset of an irritable eye o May occur in one or both eyes o History of recurrent episodes is common o Nodular type is more localized with edematous nodule over affected area Etiology o Idiopathic- 70% or greater Recurrence within 2-5 years is likely. o Collagen-vascular disease (i.e., SLE) o Gout o HZO o Syphilis o Lyme Disease o Crohn’s Disease Critical Signs o Sectorial redness of one or both eyes. Localized. Corkscrew injection o Tenderness over the injected area or nodule(s) o Nodule(s) can be moved without pain o Cornea is unaffected as is vision. Dellen possible o Anterior chamber is dark and quiet. o 1/3 bilateral o Mild, moderate, or severe o No papillae/ follicles o No history of infection o No discharge Work-UP/ Laboratory Testing o History: ask about skin rashes (HSV, HZO), venereal disease (rare), pain in the big toe (gout), recent viral illness, recent camping trips (Lyme disease), ongoing medical problems, and medications. Also IBS, ECM (Erythema chronic migrans) o Rule out scleritis by viewing episcleritis in natural light. Scleritis causes a bluish hue of the sclera. Episcleritis is bright red. o Instill 2.5% epinephrine and re-examine vascular pattern in 10 -15 minutes. Episcleral vessels will blanch. o High suspicion of underlying etiology: order ANA to rule out SLE, RF to rule out RA, ESR to rule out underlying inflammatory disorder, uric acid levels to rule out gout, RPR and FTA-ABS to rule out syphilis. Treatment o Most cases last from 10-21 days o Nodular can last up to 2 months o Mild cases: topical vasoconstrictors/ antihistamines, qid x10-21 days. Oral aspirin or NSAID can be used as prescription on the bottle for 7-10days. o Alternative therapies: topical NSAIDs (Ocufen/Acular) qid x10-14 days have been successful. Good if caused by prostaglandins o Moderate/ severe cases: topical steroids q1-2 hours until redness disappears, then reduce to 3-4 times a day. Oral aspirin/ NSAIDs can also be used to help speed recovery. Moderate: vexol Severe: Lotemax/ Pred Forte o Topical steroids require weekly IOP checks o Patient education of possible recurrences overy next 3-4 years. o No need to lab test until recurrent. Scleritis Four Types o Diffuse- 45% o Severe boring pain (#1 most prominent feature)- suicide pain. More than physical findings Pain radiates to forehead, brow, jaw, and can wake patient up at night. Onset is gradual, unlike episcleritis 50% bilateral with unilateral cases changing to bilateral in 5 years. Tearing, photophoibia, recurrent episodes are common Scleras has bluish hue in natural light Vascular pattern of sclera is distorted, especially at the limbus Nodular- 45% o Same as anterior diffuse with a nodule Single or multiple nodules that are non-moveable and very painful Nodules recur at the same site Nodules at the limbus cause rapid increased IOP Associated rheumatoid nodules at elbows in 1/3 of causes Worse in morning Necrotizing- 5% o This is the worst. There is a high morbidity and mortality of the eye and body. Blind/ dead within 5 years due to vascular disorder Same as anterior diffuse with Most severe form of inflammation- almost always associated with systemic disease. Unilateral or more commonly bilateral If uveitis is associated with scleritis, there is a high incidence of inflammatory disease at or behind equatorial region of the globe Areas of necrotic scleral tissue, necrotized tissue may exude from the area Blindness, death, and perforation are all high Doesn’t look so bad Blood vessels so inflamed that they are shutting down. Obliterated vasculitis. Flame hemorrhage under nails and necrosis around nail. Scleromalacia Perforans This is visually very dramatic Patients with necrosis of the sclera without pain or ocular inflammation. Almost all have long standing rheumatoid arthritis or rheumatoid disease Changes due to arteriolar occlusive changes which result in death/ sequestration of the affected scleral tissue. <1% perforate, so no death, LOV, etc. Etiology o 70% Induced, 30% Idiopathic o C = Connective tissue Disease (RA, SLE, PA, AS)- This is the main reason o I = Infection Disease (HZ, HS, Syphilis, Lyme Disease) o G = Granulomatous Disease (Sarcoidosis, Wegener’s) o M = Metabolic Disease (Thyroid, DM, Gout) o Accidental (Trauma, Surgery) Work-Up/ Laboratory Testing o History: previous episodes, existing etiologies from above o Examine sclera in natural light (blue hue) o Slit lamp examination to rule out uveitis, areas of involvement o DFE: rule out posterior segment inflammation o Bp, pulse, check hands, wrists, elbows, respiratory o Laboratory evaluation of CBC, ESR, uric acid, RPR, FTA-ABS, RF, ANA, FBS o Other lab testing: CXR, sacroiliac x-rays, Bscan ultrasonography to rule out posterior scleritis. Treatment o For pain/ Inflammation: Oral NSAID (Rx Ibuprofen 400-600mg po qid x1 week, Indomethacin 25mg po tid x 1 week) flurobrofen 100mg bid Only rx oral steroids if NSAIDs do not work. o Steroids- recommended for severe scleritis or necrotizing, or if no response to NSAID. (Prednisolone 60-100mg po qd) with antacid or H2 blocker. o Immunosuppressive therapy (cyclophosphamide). Useful in patients with associated systemic vasculitis o Surgery- indicated when secondary to local problem (FB, parasite) o Scleromalacia perfornas- no treatment- referral to rheumatology to evaluate ongoing systemic disease Special Items o Protective lenses for patients secondary to possible perforation from scleral thinning. o Decreased pain is a sign that the treatment is working. o Topical steroids usually do not help. If used, help in reducing the associated episcleritis o Sobconjunctival steroids (injection) contraindicated because of possible thinning and perforation at the injection site. Posterior Scleritis General o Difficult to diagnose, because unable to view the posterior sclera. o Suspicion for the disease is high if pain or discomfort outweighs the clinical findings o Can be an extension of anterior scleritis Clinical Presentations o Very few signs unless anterior sclera involved o May account for unexplained retinal detachments, disc edema, macular edema, retinal hemorrhages, angle closure glaucoma Complications o These occur late in the disease or when very acute inflammation occurs. o Occur most frequently with posterior scleritis and necrotizing scleritis withinflammation o Includes Decreased VA Due to macular/ ONH destruction (even with PH) Uveitis Glaucoma Cataracts Retinal detachments/ hemes Optic nerve swelling Proptosis Choroidal folds Positive APD Monocular color loss Treatment/ management o Same as anterior scleritis o Suspect underlying systemic etiology Thinning (Ectasia) General o This is a softening and bulging of the sclera, almost like a hernia Staphylomas o Posterior Staphyloma Most common of the staphylomas Usually due to posterior uveitis, high myopia (increased axial length = different areas of the eye have different degrees of myopia) o Anterior Staphyloma Due to anterior inflammation such as pars planitis, trauma o Intercalating Staphyloma Bulging from the sides, usually around the limbal area Due to inflammation o Total Staphyloma Total bulging of the eyes (Buophthalmos) and is commonly seen in congenital glaucoma due to increased IOP). Treatment/ Management: None Degenerative Changes Age-Related/ Senile Hyaline Plaques o Composed of calcium sulfate o A translucent area of sclera with yellowish borders and a conjunctival covering. The center of the plaque is blackish-purple and oval-shaped. o A normal, age-related change o No pain, vascularization o Flat with SLE. o Treatment: None Pigmentation Abnormalities Blue Sclera/ “Robin’s Egg Blue” o Hx: frequent fractures or breaks in weight bearing bones o Hallmark of “osteogenesis imperfect” (and other collagen disorders). This is a defect in the development stage of the sclera. o Result is a thinning of the sclera with the uvea showing through (hence, the blue color). o A white ring (“Saturn’s Ring”) can present around the limbus because it is in direct contrast to the adjacent thinning sclera o Choroidal tumors can cause a localized black area Intrascleral Nerve Loops/ “Loops of Axenfeld” o “Purple dots” which are usually located superior (raise the upper lid and have the patient look down) o The purple dots represent where the nerve and vein leave the uveal tract and take the uveal pigment with them. o Common and not pathological o Loop of LCN = Loop of Axenfeld For some reason, a loop exists in long ciliary nerve Anterior to EOM insertion Pigment cells associated with it. Can be painful.