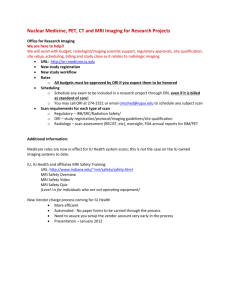
Medical Imaging- Comp Exam
advertisement

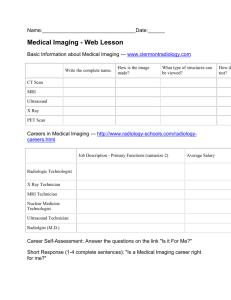
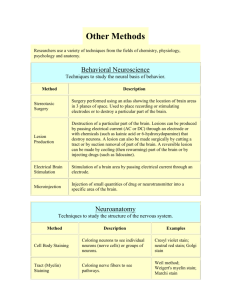
Medical Imaging- Comp Exam Medical Imaging 1 Introduction Medical imaging can be used to make a diagnosis, follow the progression, and assist in medical interventions Some techniques either measure the anatomical structures or the function (physiology) of the system, and some methods do both Methods to obtain anatomical info: US, X-ray, Computerized Tomography (CAT/ CT scan), and Magnetic Resonance (MRI) Methods to obtain physiological info: positron emission tomography (PET), single photon emission computerized tomography (SPECT), and functional MRI. Image Basics Pixel= picture element Grayscale image- 0=black and the larger values indicate lighter shades o The more Bits the detail in the image is improved, and this means the larger the file; need a compromise between image resolution and file size Spatial Resolution o Another way to improve the resolution is to increase the # of pixels per space; again compromise b/n # of pixels vs. file size Color= light traveling in given wavelengths that can be detected by the human eye (400-700 nm) o Hue= actual color of the object o Saturation= purity of light (i.e. light that is all one wavelength is very pure and fully saturated) o Intensity= relative lightness or darkness of an image Medical Imaging 2: Image Processing Noise Reduction Noise= differences in pixel values that are not related to the anatomy or physiology of the subject; noise is BAD Filters= applied to an image to reduce noise Registration Def.= process of bringing two or more images into spatial correlation (“matching”) Intermodal Registration= comparing 2 images taken with 2 different techniques (i.e. CT scan and fMRI done on the same pt.) Intramodal Registration= longitudinal monitoring of a disease; images taken of the same person with the same techniques but at different times. Doppler Imaging Based on the principles of ultrasound The detector measures the frequency shift caused by a moving reflector Vascular Doppler the moving reflector is the blood cells in the vessels They can measure blood velocity (blood flow) and produce maps of vasculature Preferred Doppler angle ranges from 30*-60*; <30*= refraction and critical angle interactions and >60*= small errors in angle can results in large errors in velocity Safety- at high intensities biological effects are caused by thermal and mechanical mechanisms o Can causes heat deposition at the bone-soft tissue interface o Mechanical- cavitation can occur along with creating free radicals Magnetic Resonance Imaging Uses magnetic fields to create images When protons are placed in the field, they can receive and then transmit electromagnetic energy Protons in the magnetic field absorb energy and they release or reradiate this energy and return to equilibrium (ground state) Relaxation= return of the nuclei to their resting state= May be T1 or T2 Bone is DARK in an MRI but white in an X-ray or CT scan Different tissues have different relaxation times MRI is a sensitive test for detection of diseases because it is sensitive to water: more water in tissue= more intense MRI signal o The exact pathology is more difficult to determine Instrumentation o Tube= bore of the magnet o Strength of the magnet is measured in Tesla; another measure commonly used is the Gauss (1 tesla= 10000 gauss) o Currently used magnet strengths for MRI’s are 0.5 tesla to 2.0 tesla; Earth’s magnetic field= 0.5 gauss Magnets o Resistive magnets: many coils wrapped around the bore through which an electric current is passed, electricity turned off= magnetic field dies o Permanent magnet: magnetic field is ALWAYS there and at full strength o Superconducting magnets: most COMMONLY used, coils made with electric wire (which is bathed in liquid helium) through which a current passes Risks: o Really NONE, doesn’t use radiation or contrast so NO tissue damage o Contraindications: pregnant, anything metal, pacemakers or metal valves, joint replacement or internal clips GOOD anatomic resolution and can be used for making 3D images from various angles BAD: machines are slow and expensive TECNIQUE of CHOICE for imaging SOFT TISSUE Functional Magnetic Resonance Imaging By looking at blood flow, functional changes in the tissue can be detected o Based on a major assumption that tissue that is more active will have more blood flow; not been proven to be true in all situations Most frequently used in the brain; more blood flow to an area is assumed to mean positive neural action 1st a traditional MRI image is produced, then the area of higher blood flow is highlighted and overlaid on traditional MRI image Limitations w/fMRI: o Blood flow= more active; not proven o Time limitation of the scan; blood flow may be increasing to one part of the brain during the beginning of the scan, but flow may be increased to another part of the brain by the end of the scan o Certain parts of the brain are more difficult to image; i.e. cerebellum CONTRAST RADIOLOGY Uses X-rays and a contrast dye to enhance images of certain tissues allows structures to be seen that aren’t normally visible with X-rays Oral Contrast medias are to highlight the GI tract o Patient asked to fast for several hours before procedure, patient drinks chalky thick drink (~48 ounces) o Barium sulfate is the most common oral agent used, tends to precipitate when in solution and in body- acid/base balance must be exactly correct and mixed with no ions (ions increase aggregation) IV contrast media and procedures Intravenous pyelography (great job illustrating detail within renal system) o Examines the function of the kidneys by measuring the rate of elimination of the media from the kidneys Angiography o Contrast media injected into the artery o The vessels and the organ (or tumor) it supplies is illustrated o GOLD STANDARD for vessel examination Histology Def.= the analysis of the anatomy of cells and tissues using microscopic techniques General methods o Obtain the tissue by needle biopsy or more commonly incision biopsy o Needle biopsy especially difficult b/c the cells have lost their normal arrangement within the tissue o Smears- sample that are physically smeared across the slide; typically done with blood o Tissue preservation and preparation Must be a fixative—a chemical that stops the degradation of the tissue that would normally occur Fixatives cross link the molecules in the tissue so they don’t come apart Microtome- special instrument used to cut tissue Stains—bring out different features of a sample H & E stain- most common; stains the nuclei blue-purple and the cytoplasm of the cell pink Masson’s Trichrome- collagen and other fibrous molecules deep blue and stains the cell red Mallory’s Trichrome- collagen and extracellular matrix proteins deep blue and other cells red and orange; used for staining keratin Weigert’s elastic- specifically stains the elastic extracellular matrix proteins like elastin Silver Stains- great for showing neurons; also used to search for fungi Wright’s stain- used for blood cells stained red or pink, nuclei is blue or purple and cytoplasm of cells is blue or gray PAS (periodic acid-Schiff stain)- important for identifying mucopolysaccarides (glycogen); blue nuclei of cells and pink collagen Fontana-Masson or Schmorl’s method- to stain melanin Metachromasia- cellular cytoplasm red and the nuclei and extracellular matrix blue X-rays most common type of medical imaging X-ray production X-ray imaging o Absorbed, reflected, refracted, penetrated o X-rays rely on photons that are transmitted o Most soft tissue looks the same b/c of the large amounts of water o Bones- high absorption, white o Air- very low absorption, black o Soft tissues- similar shades of grey o Best used for examining tissues with extremely different atomic characteristics and density o Method of choice for identifying bone fractures Risks of X-rays o Total risk is small but higher than many of the other imaging techniques o Avoided in pregnant women Computed Tomography (CT) Based on the same principles as x-rays; series of x-rays from different angles WORSE spatial resolution than x-rays BETTER contrast resolution so that certain types of tissue can be distinguished 3-D image Current CT scanners work at very high speeds; less than 30 seconds for a complete scan of the abdomen-> important because this can allow the pt. to hold breath and decrease the noise of the image The thickness of the slice can be altered on a CT scan Multiplanar- stack of CT images, displayed in sagital and coronal planes Precautions: o Very low risk to patient o Don’t use on pregnant women Ischemic stroke appears dark vs. hemorrhagic stroke appears white Nuclear Diagnostics A.K.A. scintography or radionuclide imaging Gamma Counters- imaging machines; DETECTS radiation, does not emit radiation Radiation is produced by trace amounts of radioactive material that are usually injected into the patients For Nuclear medicine it is important to use elements with short lifetimes; otherwise the pt. would have lingering radioactivity in their bodies Stable element- number of protons and the number of neutrons are equal Isotope- # of neutrons does not equal number of protons o Some isotopes have a stable nucleus (the imbalance of protons and neutrons is not enough to cause the nucleus to change) Decay- when a nucleus is in an excited state an is returning to its more stable state Radionucleotide Production o Cyclotron- machine where stable elements are bombarded with charged beams o Inside the machine the charged particles are accelerated to high energies o They hit target materials and produce nuclear reactions *****LOOK UP NUCLEAR DIAGNOSTICS TO UNDERSTAND MORE CLEARLY** Ultrasound Imaging uses high frequency sound waves to form images sound waves are emitted by a handheld transducer, or probe, and the returning wave, reflected from the interfaces b/n different tissues in the body, is detected and used to form an image Sound Waves o A vibration passing through material o Wavelength- distance b/n peaks o Frequency- how fast the wave moves over time o Amplitude- height of the wave o Resolution and attenuation of the US beam depend on the wavelength and frequency o Wavelength determines the resolution along the direction of the beam o High frequency wavelengths provide superior resolution and more image detail than low frequency beams o Low frequency beams have less attenuation with depth; thus they have greater penetration than high frequency beams o Thick body parts- 3.5 to 5 MHz is used o Small body parts that are close to surface- 7.5 to 10 MHz use o Attenuation can be measured to determine wave absorption 2 MHZ beam has ~twice the attenuation of 1 MHz beam Image processing o May result in the LEAST clear images o Signal-to-noise ratio: ability to detect small changes in the tissue o Formation of shadows- NOISE o Extremely difficult to get good US images on obese/overweight people Most common use- viewing the fetus of a pregnant woman US is thought to be the safest technique for pregnancy Echocardiographs- specific type of US used to diagnose problems with the heart o Size, shape, and movement of the heart wall during contraction o Can identify abnormal heart valves o 1-D M-Mode- uses 1 beam of US and is the most common type to view the left ventricle o 2-D- produces a broader picture of the heart