CHAPTER 21: WATER, ELECTROLYTE, AND ACID
advertisement

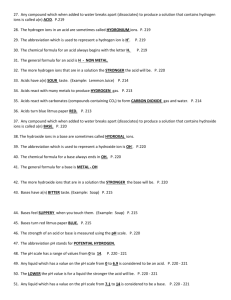
CHAPTER 21: WATER, ELECTROLYTE, AND ACID-BASE BALANCE OBJECTIVES: 1. Define the term inorganic compound and list the major classes of substances in humans that are inorganic. 2. Discuss the characteristics of water. 3. Explain what happens to a salt when it is placed in water and discuss the significance of this event in the human body. 4. Describe what happens to an acid and base when they are placed in water, and discuss the significance of these products in the human body. 5. Illustrate the pH scale, denoting acid, neutral, and basic (alkaline) pH values. Also denote the relationship between [H+] to [OH-] at each of the above pH's, and show approximately where on that scale the following substances would fall: acetic acid, distilled water, blood and ammonia. 6. Name the value of physiological pH. 7. Define the term buffer, and explain how the carbonic acid buffering system works in humans. 8. Explain what is meant by the terms water balance and electrolyte balance, and discuss the significance of each in human cells. 9. Distinguish between extracellular and intracellular fluid compartments in terms of location, and fluid composition. 10. Explain how fluid moves from one fluid compartment to another. 11. Explain how water enters and leaves the human body and discuss regulation of this process. 12. Explain how electrolytes enter and leave the human body and discuss the regulation of this process. 13. List the major sources of hydrogen ions in the body. 14. Distinguish between strong and weak acids and bases. 15. Compare and contrast the three major acid-base buffering systems that maintain pH in humans. 16. Discuss how the respiratory center is involved in maintaining the acid-base balance. 17. Discuss the important function of the kidneys in maintaining pH homeostasis in the human body. I. INTRODUCTION Throughout this course we have stressed the importance of homeostasis, or the tendency of our body to maintain a stable internal environment. Water and electrolytes are also included in this delicate balance or state or equilibrium, whereby their intake must equal their output. In order to maintain stable levels of water and electrolytes, the body must utilize mechanisms that ensure that lost water and electrolytes will be replaced while excreting any excesses. II. Review from Chapter 2: Chemistry A. Inorganic compounds are small compounds that do not contain the atoms C and H; The most important ones in humans include carbon dioxide (CO2) water, salts, acids & bases. 1. 2. CO2 is a waste product of cellular respiration . Water is a polar molecule that demonstrates hydrogen bonding and therefore it possesses very unique characteristics. a. Water is an excellent solvent (universal). o Many solutes are dissolved in our body's water. o Many ionic compounds (i.e. NaCl) dissociate or break apart in water. b. Water participates in many chemical reactions. o Dehydration (synthesis) is when water is removed from adjacent atoms (of molecules) to form a bond between them. o Hydrolysis (degradation) is when water is used to break bonds between molecules. c. Water is an excellent temperature buffer. o absorbs and releases heat very slowly d. Water provides an excellent cooling mechanism. o requires a lot of heat to change from a liquid to a gas; o high heat of vaporization. e. Water serves as a lubricant o mucus; o internal organs; o joints. f. Water is the most abundant component in cells. II. Review from Chapter 2: Chemistry A. Inorganic compounds 3. Salts: See Fig 2.9, page 46. a. Salts dissociate (ionize) into ions when dissolved in water. o an anion is formed and o a cation is formed. o Example = NaCl in water. H2O Na+ + Cl- NaCl b. 4. These ions are referred to as electrolytes (charged particles). o Electrolytes must be maintained within a very narrow range in our blood and tissues (i.e. homeostasis); o Needed for muscle contraction, nerve impulses, etc.; o Examples include Na+, K+, Cl-, Ca+, PO4-; HCO3-, etc. Acids/Bases a. Acids dissociate (ionize) in water into: o a hydrogen cation, H+, and o an anion. o Example = HCl (hydrochloric acid). H2O H+ + Cl- HCl b. Bases dissociate (ionize) in water into: o a hydroxyl anion, OH-, and o a cation. o Example = NaOH (sodium hydroxide). H2O NaOH Na+ + OH-. II. Review from Chapter 2: Chemistry A. Inorganic compounds 4. Acids/Bases (continued) c. pH Scale: o See Fig 2.10, page 47. The relative concentrations of hydrogen ions and hydroxyl ions determine the pH in our blood, fluids, and tissues; pH in body = [H+] + [OH-] . pH = -log[H+]; pH Scale ranges from 0 to 14: o o o 0 ---------------------------7---------------------------14 acid [H ] > [OH-] + o d. neutral [H+] = [OH-] basic [H+] < [OH-] Physiologic pH = 7.4 Buffering Systems Definition: Buffers are compounds added to solutions to prevent abrupt change in pH. o usually weak acids; o function by donating H+ when needed and by accepting H+ when in excess; o very important in biological systems! o Example = the carbonic acid (H2CO3) buffering system. when pH is rising H2CO3 HCO3when pH is falling carbonic acid (H+ donor) o H+ + bicarbonate ion (H+ acceptor) hydrogen ion Physiologic pH = 7.4. 1. pH < 7.4 = acidosis; lethal below 7.0; 2. pH > 7.4 = alkalosis; lethal above 7.8. III. DISTRIBUTION OF BODY FLUIDS: A. Water composes the majority of a human’s body weight: 1. 2. B. Males = 63% water; Females = 52% water. Two Major Fluid Compartments: 1. Intracellular Fluid Compartment (ICF) = fluid within cells. a. comprises about 63% of total water 2. Extracellular Fluid Compartment (ECF) = fluid outside of cells: a. in interstitial spaces (interstitial fluid); b. in blood vessels (plasma); c. in lymphatic vessels (lymph). d. comprises about 37% of total water. See Figures 21.1 and 21.2 on page 809 to better understand the division of these compartments and the fluid in each. C. D. Body Fluid Composition: Also see Fig 21.3, page 810. BODY FLUID EXTRACELLULAR FLUID INTRACELLULAR FLUID High Concentration Na+, Cl-, HCO3-; plasma contains a high fraction of proteins. K+, PO4-, Mg++ ; SO3-; negatively charged proteins Low Concentration K+, Ca++, Mg++ ,PO4-, SO3- Na+, Cl-, HCO3- Movement of Fluid Between Compartments: 1. 2. See Fig 21.4, page 811. Hydrostatic pressure and Osmotic pressure regulate fluid movement. a. Hydrostatic Pressure drives fluid out of plasma and drives fluid into lymphatic vessels; b. Osmotic pressure causes the return of fluid to plasma and regulates movement into and out of cells. Sodium ion concentrations are especially important in fluid movement regulation (i.e. water follows sodium through cell membranes). IV. WATER BALANCE A. B. C. Water intake 1. varies from person to person; 2. Majority comes from consumption of liquid or moist foods: See Fig 21.5a, page 811. 3. Dehydration synthesis produces some water. Regulation of water intake: See Table 21.1, page 812. 1. The body loses less than 1% of its water. 2. An increase in the osmotic pressure of ECF due to water loss stimulates osmoreceptors in the thirst center (in hypothalamus). 3. Hypothalamic activity triggers thirst and the person seeks water. 4. Drinking fluids distends the stomach whose stretch receptors send nerve impulses that inhibit the thirst center. 5. Water is absorbed into ECF through walls of stomach and small intestine. 6. Osmotic pressure of ECF increases back to normal. Water Output Water output occurs in a variety of ways: 1. excretion in: a. urine; b. feces; c. skin. 2. evaporation from: a. skin (sweating); b. lungs (expiration). See Fig 21.5b, page 811. Urine production regulates water output through a variety of mechanisms (see below). IV. WATER BALANCE D. 20): Regulation of Water Output: (Review Renin-Angiotensin System in Chapter See Table 21.2, page 813. 1. In dehydration: a. ECF becomes more concentrated (i.e. increase in osmotic pressure). b. Osmoreceptors in hypothalamus detect this increase in osmotic pressure. c. Hypothalamus triggers posterior pituitary to release antidiuretic hormone (ADH). d. ADH targets distal convoluted tubules and collecting ducts in nephrons to increase their water reabsorption (i.e. back into the blood). e. Urine output decreases, returning osmotic pressure of ECF to normal. 2. In water excess: a. ECF becomes less concentrated (i.e. decrease in osmotic pressure). b. Osmoreceptors in hypothalamus detect this decrease. c. Hypothalamus instructs posterior pituitary to decrease its release of ADH. d. Renal tubules decrease their water reabsorption. e. Urine output increases returning osmotic pressure of ECF to normal. See Clinical Application 21.1 pages 814 & 815: Water Balance Disorders. V. ELECTROLYTE BALANCE Electrolyte balance exists when the intake of electrolytes from various sources equals the output of all electrolytes: See Figure 21.6, page 813. A. B. C. Electrolyte Intake 1. Important electrolytes needed for cellular function (which ones are these?) are primarily obtained from food; 2. Some may be obtained from water and other beverages. 3. Some are byproducts of metabolic reactions. Regulation of Electrolyte Intake 1. Electrolytes are usually obtained in sufficient quantities in response to hunger and thirst; 2. Salt Craving may occur in severe electrolyte deficiency (rare!). Electrolyte Output 1. Most due to kidney function and urine output (see below); 2. sweating; 3. defecation. V. ELECTROLYTE BALANCE D. Regulation of Electrolyte Output 1. The kidney plays a major role in maintenance of electrolyte concentrations. Recall calcium homeostasis from Chapter 6, and the renin-angiotensin system discussed in Chapter 20 to name just a few. 2. The concentrations of some positively charged ions are particularly important: These are vital for: a. nerve impulse transmission b. muscle fiber contraction c. maintenance of Resting Membrane Potential (RMP). d. Regulation of Na+: o aldosterone (secreted by what gland?) increases sodium reabsorption in kidney tubules. e. Regulation of K+: o aldosterone also causes secretion (excretion) of excess K+ into the urine. See Fig 21.7, page 816. f. Regulation of Ca++: See Fig 21.8, page 816. o calcitonin (what gland?) decreases calcium levels by targeting: 1. Distal kidney tubules to secrete excess Ca++ into urine 2. Inhibiting osteoclast activity. o parathyroid hormone (PTH by what glands?) increases calcium levels by targeting: 1. 2. Kidney tubules to reabsorb Ca++ back into blood & Activating osteoclasts to resorb bone matrix. See Clinical Application 21.2 on page 818 concerning Sodium and Potassium Imbalances. VI. ACID-BASE BALANCE Review pages 4 & 5 of this outline. A. B. Sources of Hydrogen ions (H+): See Fig 21.9 on page 818. 1. Aerobic respiration of glucose: a. carbon dioxide (CO2) produced reacts with water to form carbonic acid (H2CO3); b. H2CO3 dissociates releasing H+ and bicarbonate (HCO3-) ions. 2. Anaerobic respiration of glucose: a. Lactic acid production. 3. Fatty Acid Oxidation: a. Acidic ketone bodies. 4. Sulfur containing amino acid a. H2SO4 5. Hydrolysis of phosphoproteins a. H3PO4 Strengths of Acids and Bases: 1. A strong acid or base will completely dissociate in water: a. Hydrochloric acid; b. Sodium hydroxide. 2. A weak acid or base does not tend to dissociate: a. Carbonic acid; b. Bicarbonate ions. VI. ACID-BASE BALANCE C. Regulation of Hydrogen Ion Concentration: Regulation of hydrogen ion concentration typically involves the elimination of H+ by either acid-buffer systems, respiratory excretion of CO2, or the renal excretion of hydrogen ions. 1. Acid-buffer systems (Chemical Buffer System – found in blood) a. H+ + HCO3-; H+ + HCO3-. When pH is rising: H2CO3 When pH is falling: H2CO3 b. Phosphate buffer system: H2PO4When pH is rising: H2PO4When pH is falling: H2PO4- c. H+ + HCO3- Bicarbonate buffer system: H2CO3 H+ + HPO4-H+ + HPO4--; H+ + HPO4--. Protein buffer systems involves plasma proteins (i.e. albumin) and certain proteins in cells (i.e. hemoglobin in red blood cells). involves carboxyl end of protein: -COOH COO- + H+; involves amino end of proteins: -NH2 + H+ NH3+. See Table 21.3, page 820 to summarize these three buffer systems. VI. ACID-BASE BALANCE C. Regulation of Hydrogen Ion Concentration: 2. Respiratory Excretion of CO2 (Physiologic Buffer System) See Fig 21.10, page 821. Recall from chapter 19 that the respiratory center is located in two specific locations in the brain stem. See Fig 19.28, page 753. a. Rhythmicity area = medulla: o b. composed of dorsal respiratory group which controls the basic rhythm of breathing; o ventral respiratory group which controls forceful breathing. Pneumotaxic area = pons: o c. Chemical Regulation: See Fig 19.30, page 755. o o o d. controls rate of breathing. Chemoreceptors in carotid & aortic bodies of some arteries are sensitive to low levels of oxygen & high levels of CO2; affect chemosensitive areas of respiratory center and breathing rate increases. Effector Sites: 1. diaphragm/intercostals 2. smooth muscle of terminal bronchioles In tissues, CO2 is produced by cellular respiration. o o o This CO2 combines with H2O to form H2CO3 (Carbonic acid) which then dissociates under the influence of carbonic anhydrase to release H+ and bicarbonate ion (HCO3-): CO2 + H2O o o H2CO3 H+ + HCO3-; HCO3- is transported in blood back to lungs; Reaction is reversed in lungs & CO2 is expelled during expiration. VI. ACID-BASE BALANCE C. Regulation of Hydrogen Ion Concentration: 3. Renal Excretion of Hydrogen Ions: (Physiologic Buffer System) See Fig 21.11, page 824. a. b. c. The kidney tubules secrete excess hydrogen ions into the urine to regulate pH; Phosphates buffer hydrogen ions in urine; Ammonia produced by renal cells helps transport hydrogen ions to the outside of the body: NH3 + H+ 4. VII. Chemical Buffers vs. Physiological Buffers: See Fig 21.12, page 824. a. Chemical Buffers act quickly; b. Physiological buffers require minutes to several days to begin to resist pH changes. OTHERS A. B. C. D. E. F. G. VIII. NH4+ See introduction on page 808 concerning deadly heat waves. Diabetes Insipidus. See purple box on page 812. Diuretics. See purple box on page 813. Hyper/Hypocalcemia. See purple box on page 817. Sodium & Potassium Imbalances. See Clinical Application 21.2 on page 818. Effect of alkalosis and acidosis on neurons. See purple box on page 820. Acid-Base Imbalances. See Clinical Application 21.3 on pages 822-823. Clinical Terms Related to Water, Electrolyte and Acid-Base Balance. See page 824. Chapter 21: Water, Electrolyte and Acid-Base Balance I. Introduction A. Balance suggests a state of equilibrium. B. Levels of water and electrolytes in the body remain relatively stable at all times. C. Water balance and electrolyte balance are interdependent because electrolytes are dissolved in the water of body fluids. D. Anything that alters the concentrations of electrolytes will alter the concentration of the water by adding solutes to it or by removing solutes from it. II. Distribution of Body Fluids A. Introduction 1. Body fluids occur in compartments of different volumes that contain fluids of varying compositions. 2. The movement of water and electrolytes between compartments is regulated to stabilize their distribution and the composition of body fluids. B. Fluid Compartments 1. The body of an average adult female is about 52% water by weight, and that of an average male is about 63% water. 2. The differences of water content between the sexes are due to the fact that females generally have more adipose tissue, which has little water. 3. The two major fluid compartments of the body are intracellular and extracellular. 4. The intracellular compartment includes all the water and electrolytes that cell membranes enclose. 5. Intracellular fluid represents about 63% by volume of total body water. 6. The extracellular fluid compartment includes all the fluid outside the cells. 7. Transcellular fluid is cerebrospinal fluid, aqueous and vitreous humors of the eyes, synovial fluids, serous fluids, and secretions of exocrine glands. 8. The fluids of the extracellular compartment constitute about 37% by volume of the total body water. C. Body Fluid Composition 1. Extracellular fluids have high concentrations of sodium, chloride, calcium and bicarbonate ions and lesser concentrations of potassium, magnesium, phosphate, and sulfate ions. 2. The blood plasma fraction of extracellular fluid contains considerably more protein than interstitial fluid or lymph. 3. Intracellular fluid has high concentrations of potassium, phosphate, and magnesium ions and lesser concentrations of sodium, chloride, and bicarbonate ions. 4. Intracellular fluid has a higher concentration of protein than plasma. D. Movement of Fluid Between Compartments 1. The two major factors that influence the movement of water and electrolytes from one fluid compartment to another are hydrostatic pressure and osmotic pressure. 2. Any net fluid movement that occurs between cells and interstitial fluid is most likely due to changes in osmotic pressure because hydrostatic pressure within the cells and surrounding interstitial fluid is ordinarily equal and remains stable. 3. Osmotic pressure is due to the presence of impermeant solutes on one side of a cell membrane. 4. A decrease in extracellular sodium ion concentration causes a net movement of water from the extracellular compartment into the intracellular compartment by osmosis. 5. An increase in extracellular sodium ion concentration causes cells to shrink as they lose water. III. Water Balance A. Introduction 1. Water balance exists when water intake equals water output. 2. Maintenance of the internal environment depends on thirst centers in the brain and the kidneys’ ability to vary water output. B. Water Intake 1. Most water is obtained through beverages. 2. Water is also obtained through food and metabolic reactions. 3. Water of metabolism is water generated in chemical reactions in the body. C. Regulation of Water Intake 1. The primary regulator of water intake is thirst. 2. The feeling of thirst derives from the osmotic pressure of extracellular fluids and a thirst center. 3. The thirst center is located in the hypothalamus. 4. Osmoreceptors detect osmotic pressure changes in extracellular fluids. 5. The thirst mechanism is usually triggered when the total body water decreases by as little as 1%. 6. The thirst mechanism is inhibited by the act of drinking water and the resulting distension of the stomach. D. Water Output 1. Water leaves the body through the urine, feces, sweat, and breathing. 2. Most water is lost through urine. 3. The primary means of regulating water output is control of urine production. E. Regulation of Water Output 1. The distal convoluted tubules and collecting ducts regulate the volume of water excreted in the urine. 2. When ADH is present, the linings of the renal tubules become more permeable to water. 3. Osmoreceptors in the hypothalamus are stimulated by the increased osmotic pressure of blood. 4. When osmotic pressure of body fluids increases, the hypothalamus signals the posterior pituitary to release ADH. 5. ADH causes the distal convoluted tubules and collecting ducts to become more permeable to water. 6. If a person drinks too much water, ADH release is inhibited so the distal convoluted tubules and collecting ducts become more impermeable to water and urine output increases. IV. Electrolyte Balance A. Electrolyte Intake 1. The electrolytes of greatest importance to cellular function release sodium, potassium, calcium, magnesium, chloride, sulfate, phosphate, bicarbonate, and hydrogen ions. 2. Electrolytes are primarily obtained by food but they may also be obtained by fluids and metabolic reactions. B. Regulation of Electrolyte Intake 1. A person normally obtains sufficient electrolytes by responding to hunger and thirst. 2. A severe electrolyte craving may cause a salt craving. C. Electrolyte Output 1. The body loses electrolytes through sweat, feces, and urine. 2. The greatest electrolyte output occurs as a result of kidney function and urine production. D. Regulation of Electrolyte Output 1. The concentrations of sodium, potassium, and calcium are particularly important. 2. Potassium ions are important for maintaining the resting potential of nerve and cardiac muscle cells. 3. Sodium ions concentrations are primarily regulated by the hormone aldosterone and the kidneys. 4. Besides sodium, aldosterone also regulates potassium ions. 5. A rising potassium level triggers aldosterone aldosterone secretion. 6. Parathyroid hormone regulates calcium concentrations by increasing the activity of osteoclasts when calcium levels are too low. 7. Negatively charges ions are controlled by the regulatory mechanisms that control positively charged ions. V. Acid-Base Balance A. Introduction 1. Acids are electrolytes that release hydrogen ions in water. 2. Bases are substances that combine with hydrogen ions. 3. Regulation of hydrogen ion concentration is very important because slight changes in hydrogen ion concentration can later the rate of enzyme controlled metabolic reactions, shift the distribution of other ions, or modify hormone actions. B. Sources of Hydrogen Ions 1. The major metabolic sources of hydrogen ions are aerobic respiration of glucose, anaerobic respiration of glucose, incomplete oxidation of fatty acids, oxidation of amino acids containing sulfur, and breakdown of phosphoproteins and nucleic acids. 2. The acids resulting from metabolism vary in strength. C. Strengths of Acids and Bases 1. Strong acids are those that ionize more completely. 2. Weak acids are those that ionize less completely. 3. Examples of strong acid are hydrochloric acids. 4. Examples of weak acids are carbonic acids. 5. Strong bases dissociate to release more hydroxyl ions or its equivalent than do weak bases. 6. An example of a strong base is sodium hydroxide. D. Regulation of Hydrogen Ion Concentration 1. Introduction a. The maintenance of acid-base balance usually entails elimination of acid. b. Acids are eliminated by the following three ways: acid-base buffer systems, respiratory excretion of carbon dioxide, and renal excretion of hydrogen ions. 2. Acid-Base Buffer Systems a. Acid-base buffer systems occur in all body fluids and involve chemicals that combine with acids or bases when they are in excess. b. Buffers are substances that stabilize the pH of a solution, despite the addition of an acid of a base. c. Chemical components of a buffer system can combine with strong acids to convert them to weak bases. d. The three most important buffer systems in the body are bicarbonate buffer system, phosphate buffer system, and protein buffer system. e. The bicarbonate buffer system is present in both intracellular and extracellular fluids. f. In the bicarbonate buffer system, the bicarbonate ion is the weak base and carbonic acid is the weak acid. g. In the presence of excess hydrogen ions, bicarbonate ions combine with hydrogen ions to form carbonic acid. h. If conditions are basic, carbonic acid dissociates to release a bicarbonate ion and hydrogen ion. i. The phosphate buffer system is in both intracellular and extracellular fluids. j. In the phosphate buffer system, monohydrogen phosphate is the weak base and dihydrogen phosphate is the weak acid. k. In the presence of excess hydrogen ions, monohydrogen phosphate combines with hydrogen ions to form dihydrogen phosphate. l. The protein acid-base buffer system consists of plasma proteins. m. If the hydrogen ion concentration drops, a carboxyl group of an amino acid can become ionized releasing a hydrogen ion. n. In the presence of excess hydrogen ions, the COO- portions of the protein molecules can accept hydrogen ions. o. In the presence of excess hydroxyl ions, the NH3+ groups within proteins give up hydrogen ions and become NH2 groups again. p. Hemoglobin is an important protein that buffers hydrogen ions. 3. Respiratory Excretion of Carbon Dioxide a. The respiratory center helps regulate hydrogen ion concentrations is body fluids by controlling the rate and depth of breathing. b. If body cells increase their production of carbon dioxide, carbonic acid production increases. c. An increase of carbon dioxide and subsequently hydrogen ions in cerebrospinal fluid stimulates chemosensitive areas within the respiratory center. d. When the respiratory center increases rate and depth of breathing, the lungs excrete move carbon dioxide. 4. Renal Excretion of Hydrogen Ions a. Nephrons help regulate hydrogen ion concentration by excreting hydrogen ions in the urine. b. The tubular secretion of hydrogen ions is linked to tubular reabsorption of bicarbonate ions. c. A diet high in proteins may trigger excess acid formation. d. Phosphate ions buffer hydrogen ions in urine. e. Ammonia produced by renal cells help transport hydrogen ions to the outside of the body. f. The body’s first line of defense against shifts in pH is chemical buffer systems. g. The secondary defenses against shifts in pH are physiological buffer systems such as respiratory and renal mechanisms. Chapter 21: Water, Electrolyte and Acid-Base Balance I. Introduction A. Balance suggests _______________________________________________________ ________________________________________________________________________ B. Levels of water and electrolytes in the body remain ____________________________ at all times. C. Water balance and electrolyte balance are ____________________________ because ________________________________________________________________________ D. Anything that alters the concentrations of electrolytes will alter __________________ ________________________________________________________________________ II. Distribution of Body Fluids A. Introduction 1. Body fluids occur in compartments of different _________________________ __________________________________________________________________ 2. The movement of water and electrolytes between compartments is regulated to __________________________________________________________________ B. Fluid Compartments 1. The body of an average adult female is about _____________ water by weight, and that of an average male is about ________________________________ water. 2. The differences of water content between the sexes is due to _______________ __________________________________________________________________ 3. The two major fluid compartments of the body are _______________________ __________________________________________________________________ 4. The intracellular compartment includes________________________________ __________________________________________________________________ 5. Intracellular fluid represents about __________ by volume of total body water. 6. The extracellular fluid compartment includes ___________________________ __________________________________________________________________ 7. Transcellular fluid is ______________________________________________ __________________________________________________________________ 8. The fluids of the extracellular compartment constitute about _______________ by volume of the total body water. C. Body Fluid Composition 1. Extracellular fluids have high concentrations of _________________________ ___________________________________________ and lesser concentrations of __________________________________________________________________ 2. The blood plasma fraction of extracellular fluid contains __________________ _____________________________________________ than interstitial or lymph. 3. Intracellular fluid has high concentrations of ___________________________ _______________________ and lesser concentrations of ___________________ __________________________________________________________________ 4. Intracellular fluid has a higher concentration of ______________ than plasma. D. Movement of Fluid Between Compartments 1. The two major factors that influence the movement of water and electrolytes from one fluid compartment to another are _______________________________ __________________________________________________________________ 2. Any net fluid movement that occurs between cells and interstitial fluid is most likely due to_________________________________________________ because __________________________________________________________________ 3. Osmotic pressure is due to __________________________________________ __________________________________________________________________ 4. A decrease in extracellular sodium ion concentration causes _______________ __________________________________________________________________ 5. An increase in extracellular sodium ion concentration causes ______________ __________________________________________________________________ III. Water Balance A. Introduction 1. Water balance exists when __________________________________________ 2. Maintenance of the internal environment depends on _____________________ __________________________________________________________________ B. Water Intake 1. Most water is obtained through ______________________________________ 2. Water is also obtained through ______________________________________ 3. Water of metabolism is ____________________________________________ C. Regulation of Water Intake 1. The primary regulator of water intake is _______________________________ 2. The feeling of thirst derives from ____________________________________ __________________________________________________________________ 3. The thirst center is located __________________________________________ 4. Osmoreceptors detect ______________________________________________ __________________________________________________________________ 5. The thirst mechanism is usually triggered when _________________________ __________________________________________________________________ 6. The thirst mechanism is inhibited by __________________________________ __________________________________________________________________ D. Water Output 1. Water leaves the body through ______________________________________ __________________________________________________________________ 2. Most water is lost through __________________________________________ 3. The primary means of regulating water output is ________________________ __________________________________________________________________ E. Regulation of Water Output 1. The _____________________________________________________ regulate the volume of water excreted in the urine. 2. When ADH is present, the lining of the renal tubules _____________________ __________________________________________________________________ 3. Osmoreceptors in the hypothalamus are stimulated by ____________________ __________________________________________________________________ 4. When osmotic pressure of body fluids increases, the hypothalamus signals the __________________________ to release ______________________________ 5. ADH causes _____________________________________________________ __________________________________________________________________ 6. If a person drinks too much water,__________________ release is inhibited so __________________________________________________________________ IV. Electrolyte Balance A. Electrolyte Intake 1. The electrolytes of greatest importance to cellular function release __________ __________________________________________________________________ 2. Electrolytes are primarily obtained by ______________________________ but they may also be obtained by __________________________________________ B. Regulation of Electrolyte Intake 1. A person normally obtains sufficient electrolytes by _____________________ __________________________________________________________________ 2. A severe electrolyte craving may cause ________________________________ C. Electrolyte Output 1. The body loses electrolytes through __________________________________ __________________________________________________________________ 2. The greatest electrolyte output occurs as a result of ______________________ __________________________________________________________________ D. Regulation of Electrolyte Output 1. The concentrations of ___________________________________________ are particularly important. 2. Potassium ions are important for _____________________________________ __________________________________________________________________ 3. Sodium ions concentration are primarily regulated by ____________________ __________________________________________________________________ 4. Besides sodium, aldosterone also regulates _____________________________ 5. A rising potassium level triggers aldosterone ___________________________ 6. Parathyroid hormone regulates calcium concentrations by _________________ __________________________________________________________________ 7. Negatively charges ions are controlled by ______________________________ __________________________________________________________________ V. Acid-Base Balance A. Introduction 1. Acids are _______________________________________________________ 2. Bases are _______________________________________________________ 3. Regulation of hydrogen ion concentration is very important because _________ __________________________________________________________________ B. Sources of Hydrogen Ions 1. The major metabolic sources of hydrogen ions are _______________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ 2. The acids resulting from metabolism vary in ___________________________ C. Strengths of Acids and Bases 1. Strong acids are those that __________________________________________ 2. Weak acids are those that ___________________________________________ 3. Examples of strong acid are _________________________________________ 4. Examples of weak acids are _________________________________________ 5. Strong bases dissociate to __________________________________________ 6. An example of a strong base is ______________________________________ D. Regulation of Hydrogen Ion Concentration 1. Introduction a. The maintenance of acid-base balance usually entails _______________ ____________________________________________________________ b. Acids are eliminated by the following three ways: _________________ ____________________________________________________________ 2. Acid-Base Buffer Systems a. Acid-base buffer systems occur in ___________________________ and involve chemicals that__________________________________________ b. Buffers are ________________________________________________ ____________________________________________________________ c. Chemical components of a buffer system can combine with __________ ___________________ to convert them to ________________________ d. The three most important buffer systems in the body are ____________ ____________________________________________________________ e. The bicarbonate buffer system is present in _______________________ ____________________________________________________________ f. In the bicarbonate buffer system, _________________ is the weak base and ___________________________________________ is the weak acid. g. In the presence of excess hydrogen ions, bicarbonate ions ___________ ____________________________________________________________ h. If conditions are basic, carbonic acid ____________________________ ____________________________________________________________ i. The phosphate buffer system is in ______________________________ ____________________________________________________________ j. In the phosphate buffer system, __________________ is the weak base and ___________________________________________ is the weak acid. k. In the presence of excess hydrogen ions, monohydrogen phosphate ___ ____________________________________________________________ l. The protein acid-base buffer system consists of ____________________ ____________________________________________________________ m. If the hydrogen ion concentration drops, a _____________ of an amino acid can become ______________________________________ releasing ____________________________________________________________ n. In the presence of excess hydrogen ions, the ______________________ __________________________________________ accept hydrogen ions. o. In the presence of excess hydroxyl ions, the ________________ within proteins give up ___________________________________ and becomes ____________________________________________________________ p. ________________ is an important protein that buffers hydrogen ions. 3. Respiratory Excretion of Carbon Dioxide a. The respiratory center helps regulate hydrogen ion concentrations in body fluids by ________________________________________________ ____________________________________________________________ b. If body cells increase their production of carbon dioxide,____________ ___________________________________________production increases. c. An increase of carbon dioxide and subsequently hydrogen ions in cerebrospinal fluid stimulates ____________________________________ ____________________________________________________________ d. When the respiratory center increases rate and depth of breathing, the lungs excrete _________________________________________________ 4. Renal Excretion of Hydrogen Ions a. Nephrons help regulate hydrogen ion concentration by _____________ ____________________________________________________________ b. The tubular secretion of hydrogen ions is linked to _________________ ____________________________________________________________ c. A diet high in proteins may trigger _____________________________ ____________________________________________________________ d. _____________________________ ions buffer hydrogen ions in urine. e. Ammonia produced by renal cells help transport __________________ ____________________________________________________________ f. The body’s first line of defense against shifts in pH are _____________ ____________________________________________________________ g. The secondary defenses against shifts in pH are ___________________ ____________________________________________________________