Chapter 4 Human Tissues
advertisement
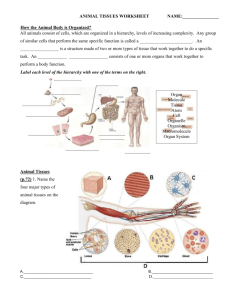
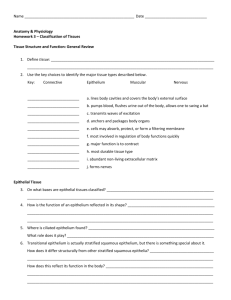
Chapter 4: Tissues Human tissues are collections of cells and cell products that Four types of tissues: Epithelial, Connective, Muscular, Nervous I. Epithelial • "covering" and “lining” • form glands Characteristics of Epithelial Tissue: • cellularity: formed of closely joined cells – in sheets • polarity – 2 different surfaces Apical (exposed) Basal (attached) surface of cells • attachment – attached to connective tissue via basal lamina (basement membrane). • avascular – • regeneration- Functions of Epithelial Tissue: 1.) Provide physical protection 2.) Control Permeability (absorption/secretion) 3.) Sensation 4.) Produce secretions Glandular epithelium Specializations of Epithelial Cells Microvilli: extensions of cell membrane on the apical surface Cilia: hair like structures which beat Maintaining the Integrity of Epithelia 1.) intercellular connections 2.) attachment to basal lamina 3.) epithelial maintenance & repair 1. Intercellular Connections: anchor cell membranes cell adhesion molecules (CAMs) intercellular cement: glycosaminoglycans – hyaluronan 1 Cell Junctions – specialized areas in cell membrane a. Tight (occluding) junctions: impermeable Lining of intestinal tract – lumen b. Gap junctions: cells held together by connexons (channel proteins) c. Desmosomes (macula adherens): in areas subject to mechanical stress Held with CAMs and proteoglycans 2. Attachment to basal lamina Two layers: 1.) lamina lucida 2.) lamina densa 3. Epithelial Maintenance and Repair • cells often only live for days and die/shed • stem cells (germinative cells) deep and have rapid mitotic rate • damaged cells quickly replaced Classified by the number of layers and the shape of cells (Table 4-1 pg. 113) A. Layers: simple: stratified: B. Shape of Cells: squamous: cuboidal: columnar: 1. Simple Squamous: one layer -good for -found in the linings of -also known as mesothelium and endothelium 2. Stratified Squamous: -most widespread -functions: -found in areas subject to friction: mouth, vagina, anus 2 3. Simple Cuboidal: one layer -have large spherical central nucleus -found in glands: thyroid & nephron 4. Transitional: - stretches & recoils without damage - appearance changes as it stretches -found in urinary bladder 5. Simple Columnar: - function for absorption, secretion, protection -found in lining of 6. Psuedostratified Ciliated Columnar: -looks striated but it isn’t - cilia function for? -found in Glandular Epithelium Exocrine vs. Endocrine Glands Endocrine glands: secrete directly into blood Secretions termed: Examples: Exocrine glands: secrete through ducts Examples: modes of secretion (Figure 4-6 pg. 119) 1.) Merocrine: exocytosis of secretions Salivary glands secrete (mucin) or mucus Merocrine sweat glands 2.) Apocrine: apical portion of cell shed with secretions Mammary glands 3.) Holocrine: entire cell ruptures to release secretions Sebaceous glands Types of secretions: 1.) serous glands 3 2.) mucous glands glands can be simple or compound in structure II. Connective Functions: 1. binds 2. framework for 3. protects 4. storage sites for & together & supports structure cells 5. forms rigid skeletal framework of body 6. limits ROM 7. transports fights (defense of body) Connective tissue consists of few cells with a lot of intercellular matrix (ground substance) Classification of Connective Tissues 1.) Connective tissue proper 2.) Fluid connective tissues 3.) Supporting connective tissues 1.) Connective Tissue Proper • contains fibers, ground substance & cells Cells associated with connective tissue proper 1. fibroblast: Secreted hyaluronan and protein fibers Important for tissue growth & repair 2. macrophages: phagocytes: 3. adipocytes: store fat 4. mesenchymal cells: stem cells 5. melanocytes: produce melanin 6. mast cells: release histamine & heparin 7. lymphocytes: WBC 8. microphages: neutrophils and eosinophils 4 Connective Tissue Fibers A. Collagenous: most abundant – “white fibers” Inelastic Strong B. Reticular: short, thin C. Elastic: Types of Connective Tissue Proper: 1. Loose Connective Tissues – “packing peanuts” Areolar, Adipose, Reticular A. Areolar: most abundant •consists mostly of collagenous fibers •large spaces between cells: •unorganized fiber arrangement •functions: 1.attach skin 2. fill spaces 3. surround & support B. Adipose Tissue: •functions: • cells do not undergo mitosis throughout life • white vs. brown fat Brown fat very metabolically active • visceral vs. subcutaneous fat: Subcutaneous fat found below skin Visceral found in abdomen (belly fat) Waist: hip ratio < 1 ideal (better: <.95 men, < .8 women) C. Reticular Connective Tissue: •similar to loose connective tissue, contains ground substance in network of interlacing fibers •make up the inner framework in 5 2. Dense Connective Tissues – Connective tissues proper, tightly packed with high numbers of collagen or elastic fibers A. Dense Regular Connective Tissue: • tightly packed bundles of collagenous fibers • many fibroblasts 1. tendons 2. ligaments 3. fascia 4. aponeuroses B. Dense Irregular Connective Tissue: •fibers oriented randomly: •found in: 1. dermis 2. fibrous coverings: (perichondrium), (periosteum), & (perineurium) 3. capsules of many organs C. Elastic Connective Tissue: •contains more elastic than collagenous fibers •good for •found in walls of 2. Fluid Connective Tissues – A. Blood: watery mix of dissolved proteins contains formed elements (cells) and plasma Formed elements: RBC, WBC, platelets B. Lymph: fluid contains protein, lymphocytes, fats Similar to interstitial fluid Circulates via lymphatics 3.) Supporting Connective Tissues: Support soft tissues & body weight Cartilage • Gel-type ground substance • For shock absorption and protection 6 Bone • Calcified (made rigid by calcium salts, minerals) • For weight support A. Cartilage •numerous collagen fibers in a firm matrix contains: 1.) Proteoglycans derived from chondroitin sulfates 2.) Ground substance proteins 3.) Chondrocytes (cartilage cells) surrounded by lacunae (chambers) •fibers/matrix formed by cells: -chondroblast: -chondrocytes •avascular: due to secretion of antiangiogenesis factor - surrounded by perichondrium Outer fibrous layer Inner cellular layer Cartilage growth (both stop in adults) 1.) interstitial growth: chondrocyte undergoes mitosis growth from within cartilage mainly during embryonic development - adolescence 2.) appositional growth: new layers of cartilage added to surface -does not occur in adults Types of cartilage 1. Hyaline: -most abundant -provides support & reduces friction -precursor to bone (fetal skeleton), costal cartilage -also found in 2. Fibrocartilage (fibrous) -collagen fibers in thick bundles -slightly compressible -found in regions that -intervertebral discs, knee joint: menisci and pubic symphysis 7 3. Elastic -contains collagen but -found in 8. Bone or osseous tissue: • strong mineralized matrix Calcium & phosphate salts Resist shattering •osteoblast: • osteocyte: Inside lacunae Lacunae interconnected with canaliculi • 2 differences between bone and cartilage: 1. bone well supplied by 2. canaliculi • surrounded by periosteum Membranes: physical barriers that line Consist of: an epithelium supported by 1.) mucous membranes: secrete mucus (sticky) Found in 2.) serous membranes: line ventral body cavities Visceral Parietal 3.) cutaneous membrane: skin 4.) synovial membranes Fasciae: provides strength, stability, route for blood & lymph vessels 1.) superficial (hypodermis): areolar & adipose tissue 2). deep: dense irregular connective 3.) subserous fascia: areolar tissue 8 III. Muscular (Figure 4-18 page 136) •specialized for • contains actin & myosin: proteins which produce all body movements •3 types of muscle tissue: all made up of myosin, actin, collagen All contract 1. skeletal: largest cells & striated Found Appearance: long multinucleated Specializations: myosatellite cells (satellite cells) – stem cells for skeletal muscle 2. cardiac: striated Cardiocyte – cardiac muscle cell Found Appearance: Specializations: intercalated discs 3. smooth (visceral): nonstriated Found Appearance: IV. Nervous (neural) Tissue (Figure 4-19 pg. 137) – Specialized for conducting electrical impulses – Rapidly senses internal or external environment – Processes information and controls responses – Forms the brain, spinal cord, nerves •Two types of cells: neurons & supporting cells (neuroglia) Neurons: conduct nerve impulses - 3 parts: dendrite, cell body & axon Cell body contains organelles -amitotic -need continuous supply of? Neuroglia cells: 9 Tissue Response to Injury: (pg. 139) Tissues respond to injuries to maintain homeostasis Cells restore homeostasis via: 1. 2. 1. Inflammatory Response (inflammation) immediately after injury area is isolated while damaged cells and microorganisms are cleaned up • infection: presence of pathogens •Inflammation: short term (acute) inflammation has 4 symptoms: 1. 2. 3. 4. •what causes this? 1. initial injury causes release of chemicals (histamine, heparin, prostaglandins, bradykini) from neutrophils, macrophages, mast cells -these chemicals cause vasodilation of blood vessels which increases blood flow to injured area = heat, redness -histamine increases permeability – makes blood vessels “leaky” = swelling -swelling puts pressure on nerve endings = pain -why is this good? 1. helps dilute toxins & remove wastes 2. brings oxygen & nutrients 3. brings phagocytes 4. increases temperature 5. brings antibodies -necrosis: tissue/cell death lysosomes: release enzymes to destroy injured cells and surrounding area – produces debris, fluid, dead/dying cells known as pus abcess: accumulation of pus in enclosed tissue space 10 2. stasis: "standing" -slowdown of blood flow Repair: 2 major ways: 1. regeneration: 2. fibrosis: scar tissue Read the text pages 138, 140 on aging, tissue structure & cancer. Also read Applications Manual page 40 - Tissue Structure and Disease. Inflammatory Conditions: Arthritis Asthma Colitis: TX: Ice therapy: Non-steroidal anti-inflammatory drugs (NSAIDs – such as aspirin, ibuprofen or naproxen) Corticosteroids (such as prednisone) Note: C-reactive protein (hs-CRP) assay: measures levels of C-reactive protein Increases during acute inflammation 11