Ex. I Determination of Malingering in Disability Evaluations (2)
advertisement
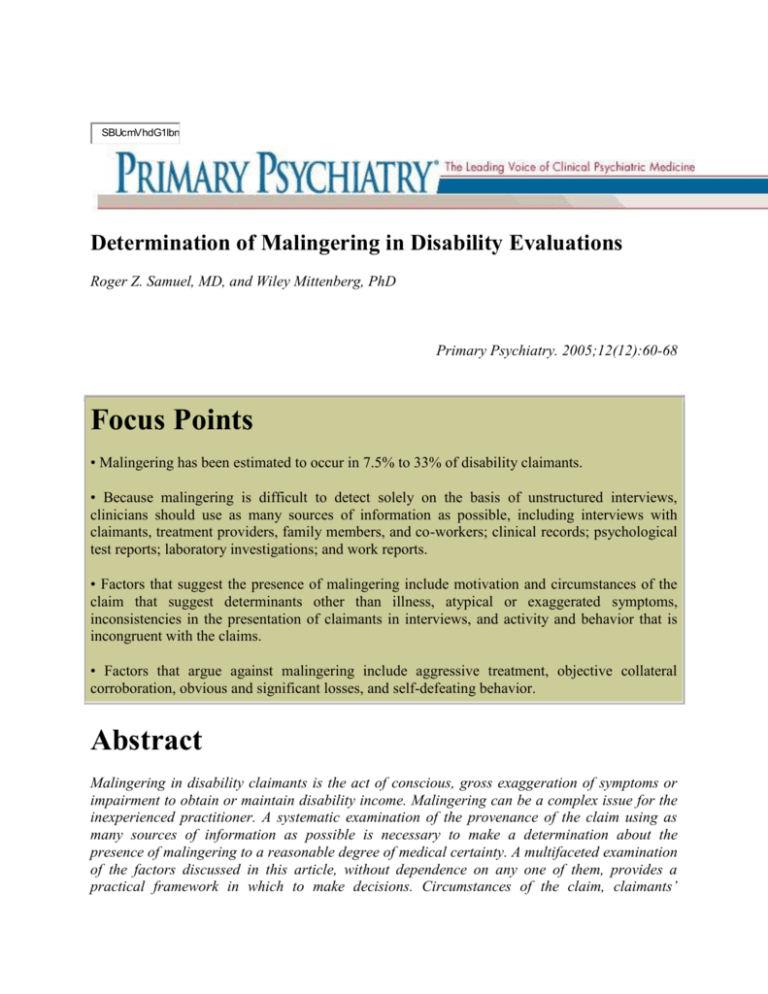
SBUcmVhdG1lbn Determination of Malingering in Disability Evaluations Roger Z. Samuel, MD, and Wiley Mittenberg, PhD Primary Psychiatry. 2005;12(12):60-68 Focus Points • Malingering has been estimated to occur in 7.5% to 33% of disability claimants. • Because malingering is difficult to detect solely on the basis of unstructured interviews, clinicians should use as many sources of information as possible, including interviews with claimants, treatment providers, family members, and co-workers; clinical records; psychological test reports; laboratory investigations; and work reports. • Factors that suggest the presence of malingering include motivation and circumstances of the claim that suggest determinants other than illness, atypical or exaggerated symptoms, inconsistencies in the presentation of claimants in interviews, and activity and behavior that is incongruent with the claims. • Factors that argue against malingering include aggressive treatment, objective collateral corroboration, obvious and significant losses, and self-defeating behavior. Abstract Malingering in disability claimants is the act of conscious, gross exaggeration of symptoms or impairment to obtain or maintain disability income. Malingering can be a complex issue for the inexperienced practitioner. A systematic examination of the provenance of the claim using as many sources of information as possible is necessary to make a determination about the presence of malingering to a reasonable degree of medical certainty. A multifaceted examination of the factors discussed in this article, without dependence on any one of them, provides a practical framework in which to make decisions. Circumstances of the claim, claimants’ symptoms, and behavior in and out of the interview situation, need to be investigated in detail to elucidate the presence or absence of malingering. Psychologic tests are useful adjunctive measures that can help determine malingering. Introduction One of the most demanding conditions to assess is malingering, especially in civil disability cases. Assessment of malingering is frequently requested by referral sources. Malingering has been present in a myriad of forms throughout the ages. One of the original uses of the term was in reference to the deliberate evasion of military duties.1 In the field of psychiatry, malingering is often an issue in criminal situations. There is published work on the detection of malingering in such cases. However, less work is published on the clinical determination of malingering of psychiatric disability in civil cases. The detection of malingering involves research documenting the ability of various indicators to be sensitive to persons known to be malingering. The determination of malingering refers to how the findings are compiled and integrated to arrive at a conclusion that an individual is “more likely than not” malingering. This article provides a practical approach to the determination of malingering in disability evaluations from both a psychologic testing perspective and a clinical perspective. These evaluations can occur in the context of long-term disability insurance, social services disability insurance, workers compensation, or personal injury. The issues are likely the same regardless of the nature of the financial incentive. Definition Malingering is defined in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition-Text Revision (DSM-IV-TR)2 as the intentional production of false or grossly exaggerated physical or psychological symptoms, motivated by external incentives such as avoiding work or military duty; obtaining drugs or financial compensation; or evading criminal prosecution. The DSM-IV-TR further suggests that malingering should be strongly suspected with any combination of the following: Medicolegal context of presentation (as in disability evaluations), marked discrepancies between claims and objective findings, lack of cooperation with evaluations or treatment, or presence of antisocial personality disorder. Antisocial personality disorder is not usually found in disability claimants, especially those with private disability policies, most likely because claimants need good employment capabilities and histories in order to get jobs in which they are eligible for such policies. However, the other three factors usually occur. Although this definition has been criticized by certain authorities in the field,3 it is a useful starting point in the process of identifying malingering in disability claimants. The crux of this definition is that it is the conscious production of false or exaggerated symptoms, or exaggeration of the impact of psychiatric symptoms or conditions on an individual’s functioning. Slick and colleagues4 proposed research diagnostic criteria for malingering cognitive dysfunction that combine information from the psychiatric interview with psychologic test results. The diagnostic criteria are probabilistic, and similar to National Institute of Neurological Disorders or American Academy of Neurology diagnostic criteria for other conditions. The criteria may also be informative in disorders that can be associated with cognitive complaints such as chronic pain.5 Rogers3 has suggested that the DSM-IV-TR criteria are minimalistic and difficult to apply. His argument is that the requirement for determining internal versus external motivation creates a false dichotomy between factitious disorders and malingering, and that in clinical practice overlap often occurs between these conditions. He further argues that the DSM-IV-TR criteria: Do not specify the psychological or behavioral parameters that suggest voluntariness of symptom production or that assist in differentiating pursuit of the sick role (a psychological conclusion) from pursuit of financial or other external goals (a behavioral conclusion).3 Rogers conceptualized exaggeration of symptoms by claimants as adaptive behavior. Claimants with a genuine, significant disability who exaggerate the severity of their reported symptoms during an evaluation can be considered as uttering a plea for help. Claimants with mild symptoms who know that these symptoms do not constitute a compensable disability, and who grossly exaggerate their symptoms in order to obtain compensation can be considered to be malingering. Two models that Rogers proposed for detecting malingering are the Threshold Model for Consideration of Malingering and the Clinical Decision Model for Establishing Malingering. The Threshold Model suggests that malingering should be suspected when psychologic or physical symptoms are accompanied by one or more specific criteria. The first criterion is suspicion of voluntary control of symptoms as demonstrated by one or more indicators, which include bizarre or absurd symptomatology, atypical symptomatic fluctuation consistent with external incentives, or unusual symptomatic response to treatment that cannot otherwise be explained (eg, paradoxical response to medication). Criteria also include atypical presentation in the presence of environmental incentives (eg, disability claim, tort action, obtaining drugs, shelter); atypical presentation in the presence of noxious environmental condition (eg, prosecution, military duty, undesirable work); complaints grossly in excess of clinical findings; and substantial noncompliance with evaluation or treatment. According to the Clinical Decision Model for Establishing Malingering, specific criteria must be present. Psychologic or physical symptoms must clearly be under voluntary control as manifested by one or more indicators, which include patient acknowledgment of voluntary control of deceit, gross symptom production that is inconsistent for physiologic and anatomic mechanisms, direct observation of illness production, discovery of paraphernalia or substances explaining the production of physical symptoms, and confirmatory laboratory testing (eg, absence of electroencephalograph abnormalities during an observed “seizure”). Other criteria include clinical certainty that illness production occurs in response to pursuit of financial gain, shelter, or drugs, or avoidance of work, military duty, prosecution, or legal consequences; another disorder, if present, cannot explain the current symptoms; and evidence of desire to assume the sick role, if present, cannot explain the totality of current symptoms. One problem with Rogers’ Clinical Decision Model is that the first criterion is almost never obtained in psychiatric disability evaluations or is very difficult to obtain. Both Rogers’ Threshold Model and the DSM-IV-TR indicators are intended for screening purposes. Psychiatric disorders are notoriously easy to malinger as they are defined by subjective complaints in the absence of objective tests to validate diagnoses. Treaters accept complaints because their role is to help individuals who are often reluctant to acknowledge the presence of a psychiatric disorder and to undergo treatment. The subjective truth is often accepted as the truth in psychotherapy, and therapists assess their patients with this notion in mind. A mental disorder to consider in the differential diagnosis of malingering is factitious disorder, which is described by the DSM-IV-TR criteria as being the “intentional production of physical signs or symptoms” in order to assume the sick role. According to this definition, there is an intrapsychic need rather than external incentive. The requirement for finding internalized motivation may create difficulties in clinical practice. Rogers3 quotes Fenichel as writing that secondary gain cannot be the sole criterion for assumption of the sick role, since external or secondary gains are inherent in all illness. Fenichel proposes that the following features suggest motivation for the sick role: strong masochistic needs; sickness that allows inappropriate regression and avoidance of adult (especially sexual) responsibilities; illness that symbolizes anger at or conflict with authority figures; psychiatric or medical care that fulfills massive dependency needs; or illness that symbolizes attempts at mastery of past trauma (eg, repetition, compulsion). According to the DSM-IV-TR, external incentives negate the factitious disorder diagnosis and suggest malingering. Epidemiology In a 1961 report about 50 individuals that they were unfit to work after head injury, Miller6 revealed an inverse relationship between degree of disability and severity of injury as well as an absolute failure to respond to therapy until compensation issues were settled. After settlement, 48 individuals were able to resume work. Base rates of malingering and symptom exaggeration were estimated by Mittenberg and colleagues,7 who reported from a survey of the American Board of Clinical Neuropsychology membership that 30% of disability cases involved probable malingering and symptom exaggeration. This was estimated to be the base rate for malingering and symptom exaggeration. A quantitative review of 11 empirical studies of mild head injury found similar base rates using objective diagnostic measures.8 Rosenfeld and colleagues9 found that the base rate for malingering in neuropsychologic examinations in the clinical context is much lower than the rate set by Mittenberg and colleagues.7 They estimated a 15% base rate of malingering and neuropsychologic examination in clinical contexts. Base rates of malingering in forensic context are difficult to accurately determine as claimants who have prevailed in litigation tend not to admit that they faked or exaggerated symptoms or complaints. Public opinion surveys suggest that purposeful misrepresentation of compensation claims is viewed as acceptable by the general population.10,11 Various studies have suggested that base rates can vary from 7.5% to 33%.12-15 Clinical Determination of Malingering Studies have shown that clinicians lack efficacy in detecting malingering or simulation solely on the basis of unstructured interviews. Psychiatrists ddetect approximately 50% of lies in interviews, which is no better than that which would be discovered by chance.16-18 While lying or simulation are not to be directly equated with malingering, these studies do inform that clinicians cannot distinguish between genuine, fake, or exaggerated complaints on the basis of demeanor. Although certain investigators are testing functional magnetic resonance imaging use in the detection of lying, thess works are still in the preliminary stages and are not available in clinical practice. Therefore, it is imperative that as many sources of data as possible should be utilized. Malingering has to be characterized as an entity similar to a syndrome in clinical practice (ie, an aggregate of features associated with and constituting a picture of a condition). It can range from very mild and subtle presentations to flagrant cases. There is no litmus test for malingering. No single item, test, or fact (including psychologic tests) rules in or rules out malingering (other than perhaps the direct admission of the claimant or cognitive test performance that is significantly less accurate than would occur by chance). As with all forensic evaluations, malingering must be suspected in all disability claims. Malingering must be included in the differential diagnosis, and factors to rule in or rule out malingering need to be actively considered and then accepted or rejected. Another important point is that malingering can coexist with psychiatric disorders. Individuals can have one psychiatric disorder and malinger in the way of faking or exaggerating symptoms of other disorders. Likewise, individuals can have a psychiatric condition and exaggerate or fake the symptoms of that condition, the persistence of symptoms of that condition, or the impact of those symptoms on their functioning. Any one of these constitutes malingering. The demeanor, affect, facial expressions, and behavior in the interview should not be used as the sole criteria for determining the presence or absence of malingering, because psychiatrists and other clinicians are inaccurate in their detection of lying or simulations in interviews. The demeanor of the claimant is usually not a helpful clue in determining the presence of malingering. Techniques utilized to increase the accuracy of detection of malingering include using multiple sources of data, prolonged interviews, and psychologic tests that assess effort or “faking” during test taking. Forensic evaluations necessitate an examination of the nexus between compensable damage and symptoms that are corroborated by multiple data sources and not just by subjective complaints by the claimant. Clinical approaches may therefore not be adequate for differentiating exaggerated or malingered presentation from atypical cases. It cannot be overemphasized that as many sources of data need to be used as are available. The most obvious source of information is the claimant. Other sources of information include clinical records, laboratory investigations, correspondence, collateral interviews, applications by the claimant, and psychologic test reports. Collateral interviews include direct interviews of treatment providers (both psychiatrists and psychotherapists), interviews of family members, interviews of coworkers or supervisors if possible, and interviews of friends or acquaintances if possible and relevant. Reviews of records are another source of helpful information. These include records of all treatments providers of psychiatry or psychotherapy, as well as providers in other specialties (eg, general practitioners) who may have documented or provided treatment for the claimant’s psychiatric symptoms. Records of applications for health insurance or other such policies are also surprisingly good sources of information; they may reveal statements by claimants that conflict with disability claim statements as the needs of each type of claim are diametrically opposed. Health or life insurance applicants must look as healthy as possible and disability claimants must look as sick as possible. Records of investigations by regulatory authorities or court hearings involving claimants are also very useful. Cripe19 criticized the use of records in determining an individual’s condition, pointing out that records reviews are based upon limited sampling, are based on different report writing styles, are an indirect method with a lack of direct contact, narrowly focus on only part of a clinical evaluation, and provide subjective biased interpretations There is also a lack of empirical studies to validate this method. These limitations would be evaded by the use of clinical interviews. Getting as many sources of data as possible helps get as accurate a picture of the claimant’s life as possible and helps to track chronologically the sequence of symptoms and events pertinent to the claim. These sources of data are subsequently utilized to determine if the claims of illnesses, symptoms, or impairment caused by illnesses, are corroborated or contradicted by other sources of information. Prolonged interviews have also been utilized to determine the validity or accuracy of claims. It is more difficult to maintain an exaggerated stance or maintain false symptoms over a prolonged period of time (eg, 4–6 hours), and fatigue as the interview progresses leads to mistakes or trouble remembering any falsehoods that may have been verbalized. Some evaluators interview claimants in two separate sessions, typically prolonging the second interview. This is helpful in obtaining information between sessions and then clarifying such information with the claimant in the second session. In addition, claimants sometimes do not recall what they said during the first interview and contradict themselves in the second interview. Interview and history taking helps determine the consistency of report or impairment. According to Reynolds,20 the key to appropriate determination consists of three components: Congruence of the current symptom presentation with the known history and facts surrounding the injury (in this case, the illness); congruence of the symptoms in juxtaposition with one another (ie, the internal consistency of the symptom presentation); and congruence of the course of symptom development and history with known (ie, probabilistic) outcomes or sequelae with like injuries (in this case, illness). Both forensic examiners and clinicians may be reluctant to give an opinion of malingering for a variety of reasons, which include litigation fear, concerns about error, and the pejorative nature of the term. One way of getting around this has been to utilize the term poor motivation or poor effort rather than malingering. However, this is not without disagreement either. Slick and colleagues4 suggested that redefining malingering in terms of poor motivation is euphemistic and inappropriate. As cited by Sreenivasan and colleagues,21 they therefore gave alternative descriptors of definite, probable, and possible to summarize evidence of exaggeration or fabrication of cognitive dysfunction. There are multiple reasons why claimants might exaggerate symptoms or impairments. Rogers3 posited that malingering represents an adaptive course of action in order to achieve a specific objective. Mittenberg and colleagues22 discussed a tendency among patient’s with mild head injury to reattribute benign emotional and other complaints to the head injury. Binder and Rohling23 concluded that patients with incentives had more abnormalities than those with more severe injuries but without financial incentives. There was an association between the presence of financial incentives and more severe symptoms after closed head injury. As this association was particularly strong in individuals with mild head injury, they concluded that financial incentives do have an effect on levels of disability and symptoms. Courtroom decision makers have a tendency to put more weight on the opinions or testimony of treaters rather than on forensic examiners, who are sometimes viewed as hired guns. Treaters sometimes lose sight of neutrality in their advocacy of their patients’ position, at times to the detriment of determining the facts. Reasons for this include overidentification with their patients, lack of access to all available information, acceptance of patients’ reports and requests at face value without objective validation, altruism, and narcissistic defensive reactions (in a desire to avoid a different opinion which may be seen as belittling their opinions or competence). There are cases in which treaters lose their objectivity and seem to collude with their patient claimants in adhering to a position of impairment and disability in the face of strong evidence to the contrary. This may be due to loss of neutrality as discussed above, or may sometimes be due to more nefarious reasons such as a desire to continue to obtain financial benefit from a patient who has to be in treatment to continue to receive benefits. Sometimes claimants seek out treatment from friends, associates or relatives where there is a clear loss of objectivity and often a clear goal of obtaining and maintaining disability. Psychologic Testing Psychologic tests can provide objective evidence of exaggerated cognitive or emotional symptoms that meets standards for the admissibility of scientific evidence set forth in Daubert versus Merrell Dow Pharmaceuticals.24 These standards may guide trial judges in decisions about the validity of an expert’s opinion in disability claims that become the subject of litigation.25 Signs of malingering may be present on standardized tests of mental status, tests used to evaluate personality characteristics, and on measures that are specifically designed to evaluate exaggerated cognitive impairment. Standardized Tests of Mental Status Disability evaluations frequently include assessment of the claimant’s attention, concentration, memory, and intelligence. The Wechsler Adult Intelligence Scale, Third Edition, (WAIS-III)26 is typically used to assess the claimant’s intelligence quotient, and contains measures of attention, concentration, verbal reasoning, nonverbal problem solving, and speed of thought process. The Wechsler Memory Scale, Third Edition, (WMS-III)27 is the most widely used means of testing verbal and nonverbal memory efficiency, and also contains tests of concentration and attention span. A claimant can produce reduced scores on the WAIS-III and WMS-III by intentionally giving incorrect answers, but a convincing level of impairment is more difficult to portray. Malingerers often obtain IQs or memory indexes that are not consistent with daily functioning or the claimed psychiatric diagnosis.7 For example, test scores in the borderline mentally retarded range (70–79) are inconsistent with independent global functioning or with the clinical presentation of dysthymia or anxiety disorders. The malingered pattern of component ability scores on the Wechsler tests is also often discrepant from the pattern produced by actual cognitive impairment. For example, performance on measures of attention span (such as digit repetition) that is significantly poorer than performance on memory tests (eg, story recall) indicates exaggeration because it is not possible for an individual to remember more information than they can initially attend to.28 Performance on tests of recall (eg, “Tell me the words I asked you to remember”) that is significantly better than performance on measures of recognition memory (eg, “Did I ask you to remember the word pen or pencil?”) also suggest exaggeration. 29 Regardless of the extent of memory impairment, it is in comparison easier to correctly recognize information and relatively more difficult to spontaneously recall information. Personality Tests The Minnesota Multiphasic Personality Inventory, Second Edition (MMPI-2)30 is the most frequently administered psychologic test for assessing emotional and somatic complaints in the context of disability evaluations. The MMPI-2 contains scales that assess the claimant’s selfreported Axis I symptoms and scales that assess the validity of the claimant’s complaints. Scale scores have an average of 50, and a score >65 may be consistent with an Axis I disorder. Obvious differences between the observed and self-reported magnitude of the claimant’s symptoms suggest exaggeration. A score ≥80 on the F (faking) validity scale probably reflects an attempt to claim excessive impairment. Scores of ≥70 on the L (lie) validity scale similarly suggest distortion of reported symptoms in order to manipulate the impression conveyed.31 The Millon Clinical Multiaxial Inventory, Third Edition (MCMI-3)32 assesses the claimant’s reported Axis I and Axis II symptoms. Scores >75 on the Axis I scales and >85 on the Axis II scales may be clinically significant. The MCMI-3 also contains scales that assess the validity of the claimant’s complaints. A score >75 on the debasement index suggests that the claimant presented more troublesome emotional and personal difficulties than are likely to be uncovered upon objective evaluation. The Structured Interview of Reported Symptoms33 and the Miller Forensic Assessment Test6 evaluate exaggeration of psychotic symptoms. Interview questions assess the presence of symptoms that are not typically comorbid, reportedly follow an atypical course, do not actually characterize Axis I disorders, are more extreme than clinically typical, occur in response to the interviewer’s suggestions, and are reported but not observed during the course of the interview. Significant numbers of such reported symptoms indicate malingering. Tests of Exaggerated Cognitive Impairment Claims of concentration and memory impairment are common in cases of disability related to mood disorders, anxiety disorders, pain, and dementia due to degenerative, traumatic, infectious, and other etiologies. Several tests have been specifically designed to assess the validity of concentration and memory impairment. The Test of Memory Malingering34 assesses visual memory for a series of pictures. The Portland Digit Recognition Test35 and Victoria Symptom Validity Test36 both assess recognition memory for numbers. The Word Memory Test37 assesses the accuracy of verbal memory for a word list. These tests appear to be demanding measures of concentration and memory, but are actually insensitive to impairment caused by Axis I disorders. Accuracy scores that are lower than those actually obtained by patients with these diagnoses indicates probable exaggeration. Each question on these tests has two possible answers, one correct and one incorrect. A claimant who could not concentrate on or recall any of the test items would answer approximately 50% of the questions correct just by chance. Accuracy scores that are significantly lower than would be obtained by guessing (eg, 30%) indicate that the claimant knew the correct answers and intentionally gave incorrect answers, and are therefore definitive evidence of malingered concentration and memory impairment. The Rey-15 item test is another measure of exaggerated visual memory difficulty. The Rey assesses recall for pictures and numbers presented simultaneously. This test has poor specificity and sensitivity, and is less reliable than the procedures described above.38 Limitations of Psychologic Tests Psychologic testing often provides useful information in the context of disability evaluations, but as with any diagnostic procedure, this utility has limitations. Approximately 40% of claimants that are exaggerating symptoms will not be identified by standardized tests of mental status or tests designed to assess the validity of cognitive impairment. Only approximately 30% of malingering claimants score below chance levels on cognitive tests, and approximately 40% of cases that involve symptom exaggeration can be identified by validity scales on personality tests.27 The true positive diagnostic accuracy rate (sensitivity) of psychologic tests is usually positively related to the rate of false negative diagnoses (specificity), the prevalence of exaggeration for the claimed disorder, and the complaints of the individual claimant (eg, affective versus cognitive symptoms, moderate versus severe functional impairment). Informed clinical practice therefore requires that multiple sources of information be considered. Factors For and Against Malingering Heilbrun39 suggested that factors that determine malingering should be broken down into three components—history, motivation, and behavior. Sreenivasan and colleagues21 provided a sample checklist for the assessment of amplification/malingering in head injury in which they created a model with which to weigh multiple factors in assessing head injury claimants. They broke down the components into the following: neuropsychologic testing issues, congruence of testing and behavior, congruence of symptoms or signs with clinic data, nonclinical factors, presence of psychiatric or other conditions that may contribute to amplified or atypical symptoms, and miscellaneous (eg, history of litigation, lying, malingering, criminal activity, job track record, and prior responses to injury). Malingering should be investigated by a search for features or symptoms in the following four domains: Motivation/circumstances, symptoms, claimant interview presentation, and activity/behavior outside interview (Table 1). The degree of correlation with malingering is proportionate to the number of the abovementioned factors and can be reported as highly consistent with malingering, moderately consistent with malingering, or minimally consistent with malingering. There are also factors indicating that a person may not be malingering and that the claim may be justified (Table 2). Illustrations of Malingering Motivation/Circumstances Financial Incentive One of the most common reasons for malingering is the financial incentive in obtaining income from the claim. Solution to Socioeconomic Problems Given economic and business cycles and social circumstances, sometimes getting disability payments is the only or best solution to a financial crunch. Sometimes this is very apparent in physicians who make claims for disability. One such physician was stuck with few options for practice. Due to child abuse conviction and false information provided on medical licensing board forms, and alcohol and prescription drug abuse, this physician lost his license to practice in the state in which he had a pain treatment practice. Due to patient neglect allegations and the earlier listed problems, he also was unable to get medical malpractice insurance coverage. In addition, he developed a bad reputation in the medical community and his referrals dwindled. The state in which he lost his license reported this fact and the only other state in which this physician was licensed also withdrew his medical license to practice there based on reciprocity issues. The physician therefore could not practice in any of the states in which he had licenses. It was in the midst of these circumstances that he made a claim for being disabled. Antisocial Acts/Behavior Antisocial acts and behavior consist of those that conflict with regulations, ethics, rules, laws, and other codes of conduct required of professionals or laypeople. An example of this is a podiatrist who had an unusual hallucination symptom claim. The psychiatric issues came to the forefront after a criminal investigation into insurance fraud. Prior to that, he did not have any psychiatric history. As a result of insurance fraud conviction, he was unable to practice as a podiatrist and needed income to pay for bills and his legal expenses. He pointedly avoided mentioning the fraud investigation to disability insurance agents until he was repeatedly questioned, upon which he admitted it. He also utilized the diagnosis of bipolar disorder in his criminal case as a mitigation factor in the sentencing phase. Career Dissatisfaction Career dissatisfaction is frequently seen in physicians who have very busy practices, diminishing financial rewards due to malpractice and managed care intrusion, and lack of time and opportunity to enjoy themselves outside the work environment. Work Conflict In cases where an individual has a conflict with coworkers or supervisors, he or she may choose to use disability claims as a means of getting out of the untenable work situation. It is plausible that the features or symptoms of a genuine mental condition (eg, irritability or bizarre behavior that alienates coworkers, reduced job performance due to decreasing cognitive abilities) contributed to the work situation becoming untenable. This can be investigated through workplace reports and interviews with coworkers and supervisors. End of Career Some individuals claim to be disabled at retirement age or after retirement because disability payments provide a source of income of sometimes up to 5 years between age of retirement and social security benefits. One such claim was made by an accountant in his 60s who had been in treatment for many years for major depressive disorder (MDD) with no change in his clinical status. He functioned as an accountant for a city and received good work reviews. As soon as he was eligible for retirement from his city job, he retired and then almost immediately made a claim for disability based on MDD. In Treatment for Documentation Purposes Sometimes an individual will not seek treatment or refuses to get treatment for claimed psychiatric conditions until he or she is informed that one of the requirements of the disability insurance policy is appropriate treatment by a medical professional. It is at this stage that the individual then enters treatment. Such individuals are often not fully compliant or are resistant to appropriate intervention for their claimed psychiatric condition. History of Lying, Malingering, and Dishonesty A past history of lying and malingering reveals a propensity for dishonesty that is relevant in a current claim of disability. Change in Diagnosis to Better Fit Policy Requirements A change in diagnosis to better suit policy requirements is a sign of malingering. One example is an individual who initially claimed to be disabled due to a cardiac condition. Upon deeper examination of his cardiac situation by the disability insurance company and independent examination, it turned out that he did not have a severe cardiac condition and that he was unimpaired from a cardiac point of view. Upon getting this news, the claimant then made a change in diagnosis to claim that he was depressed and therefore unable to function at his job. Another example is a woman who was in treatment for postpartum depression. She did receive disability benefits for 2 years based on this claim. However, after 2 years, she was informed by the disability insurance company that her policy only provided a disability benefit period of 2 years for mental health claims. At this point, the claimant and her psychiatrist made a change in diagnosis to bipolar disorder and the claimant then requested ongoing disability payments, arguing that bipolar disorder was a physical rather than mental condition. Symptoms Unusual or Atypical Symptoms As is the situation in malingering in any circumstance, lay people frequently choose dramatic symptoms or portray themselves as seen in the popular media. However, these dramatic or florid presentations are often inconsistent with typical symptoms seen in the psychiatric conditions being malingered. This also includes stretching of DSM-IV-TR criteria to make symptoms fit a specific disorder (eg, specific phobia to describe a physician’s litigation anxiety about seeing patients in a hospital). An example of unusual symptoms is the earlier mentioned podiatrist in his mid-30s who made a claim for disability based on a new diagnosis of bipolar disorder. One of the symptoms claimed was that of hallucinations of a female in the individual’s bedroom. Not only was the presence of visual hallucinations atypical, the specifics of the actual hallucination were dramatic and varied each time the claimant talked to different people. He told the insurance company representative that he saw a little old lady with green hair. He told his psychotherapist that he saw a woman with green hair and green eyes. He had told an independent psychiatrist who interviewed him that he saw a redheaded woman with green eyes. Currently Asymptomatic With Claim of Future Decompensation Some individuals are found to be in symptom remission for the anxiety or mood disorders based on their report and their psychiatrist’s records and report, but they nevertheless claim that if they were to return to their work, they would likely become symptomatic again due to the stress of the work. This then becomes the sole basis for the claim. There appears to be an increase in this type of claim especially in frequency of claims made by physicians. Exaggeration of Symptoms/Impairment There may be claimants who genuinely have symptoms which may not be severe enough to cause impairment in functioning. Just as there are individuals who work while undergoing treatment of mild to moderate psychiatric conditions, claimants may also start out in a more severely debilitated condition and then improve such that their condition is no longer impairing in severity. The claimants may still insist that they are unable to work. An example of this situation is a cardiologist 47 years of age who claimed to have severe MDD with impaired concentration and anhedonia. However, an examination of his past, both in his records and in his interview, showed that during the time that he was making this claim the cardiologist went on a 3-week recreational holiday with his family. During this holiday he not only enjoyed himself, but he also studied for a medical board examination which he subsequently passed. Psychologic Test Results These were discussed in detail above. Essentially, psychologic test results can provide evidence of lack of effort or faking of symptoms. These can especially be helpful in examining claims of impaired cognition such as with impaired concentration. The lack of evidence of poor effort or faking on psychologic tests by itself does not rule out malingering. If enough factors are present to suggest malingering, then malingering is a rational conclusion. In a somewhat paradoxical twist, good performance on tests of malingering can actually substantiate a diagnosis of malingering, as in a situation wherein an individual claims to have severely diminished concentration that impairs job performance. Most treaters do not perform careful tests of concentration but take their patient’s claims at face value. If such an individual is malingering and undergoes psychologic testing, there are two possible outcomes. First, the individual would not put in adequate effort and this may show up on tests of effort. Second, the individual could put in adequate effort and his or her performance on concentration tests would not be impaired. Therefore, even though psychologic testing would not show malingering based on tests of effort or faking, it would show that when the individual puts in good enough effort, the concentration is good. This then argues for the presence of malingering (ie, an exaggeration of impairment or a false claim of impaired concentration). Psychologic test results may be more helpful to rule in malingering than to rule it out, though it may be that only appropriately validated psychologic tests meet Daubert standards24 for admissibility in court. Daubert is more rigorous in terms of scientific evaluation of methods and more flexible regarding the application of new methods. Since only psychologic tests have known classification accuracy at this time, it might be argued by some that the clinical findings provide valuable support for the psychologic test results rather than the other way around. Symptoms Incongruent With Usual Course of Illness Based on the current standard of care, the goal of treatment of certain psychiatric conditions, such as MDD, is remission of symptoms. Even though there are treatment-resistant cases, treatment remission is achievable with optimal treatment. Therefore, in an individual who has not gone through the stages that would substantiate the presence of treatment resistant depression, lingering mild to moderate symptoms as the basis of a claim of disability would be suspicious for malingering. Remaining on subtherapeutic doses of medications or refusal to maximize doses or therapeutic regimens for prolonged periods of time may be seen as indicators of malingering. Claimant Interview Presentation Admission of Malingering Admission of malingering is a rare event if it occurs at all. Some authors have suggested that an empathic approach at the end of interviews with claimants in which the examiner discusses how understandable it would be for an individual to feel forced to portray themselves in a more sick fashion may bring about a concession from the claimant that they may be exaggerating or may not be as ill as they claim. In the practice of Roger Samuel, MD, the lead author of this article, such attempts have met with anger or derision. Despite best efforts, perhaps the examiner did not come across quite as empathic or tactful as other authors may have been. Since a frequent requirement of independent examinations is that the examiner should not provide any opinions or recommendations to the claimant, it may not be appropriate for the examiner to suggest that the claimant is malingering if this is framed in the form of an opinion. On the other hand, confrontation of the claimant with discrepancies may be a viable technique in eliciting admissions of exaggeration or falsifications. Lack of Cooperation With the Examiner Lack of cooperation may take the form of refusal to participate in the examination, refusal to continue the examination after it has started, or selective provision and withholding of information in the history. For example, a plaintiff in litigation against her employer (a school district) for being sent to work while in pain claimed to be suffering from MDD. Athough she was referred to the examiner by her attorney, on the advice of her attorney she refused to answer questions about her past psychiatric history and substance abuse history, both of which were relevant to her condition. Some malingerers act explosively or in an intimidating manner to get the examiner to shorten the interview. Refusing to participate in or complete an examination does not allow an independent examiner to get a full picture and may serve as a delaying tactic. In such circumstances, it is still possible to produce a neutral report that may be helpful as long as a disclaimer about the claimant’s participation is specifically noted. Relevant history from the records and whatever the claimant provides in combination with a description of the mental status of the claimant during the examination may be sufficient. Discrepancies Between Interview Report and Documentation Discrepancy between interview and documentation signifies false or exaggerated claims or noncompliance. One example of such a situation is when a claimant insisted that he had been fully compliant with office visits with his psychiatrists and with psychotropic medication prescribed, while a review of his records revealed significant lapses in treatment with psychiatrists as well as refusal to take or continue medications at various points in his treatment. Activity/Behavior Outside Interview Working During Period of Claim Some individuals claim that they are disabled despite records revealing that they actually worked during the claim, or are currently working. This is also seen in physicians who have ownoccupation policies, which provide them with disability insurance payments if they are not able to work in their specialty. One example was a radiologist who claimed to have bipolar disorder, which had never actually been diagnosed by any of his treating professionals. While claiming that he was disabled and impaired, it was discovered that he was doing teleradiology as well as osteoporosis treatment. Further investigation revealed a decline in his income in the years preceding his claim. Capacity for Recreation, Non-Work Activity In individuals who claim to have severe psychiatric conditions such as MDD, ability to enjoy their lives in recreational activities argues against the presence of a severe or impairing psychiatric condition. One such claimant stated she could not continue to manage her consulting business, while at the same time she led a very active life outside work. She traveled extensively, volunteered in hospitals, volunteered for political campaigns, and went out socially to dinners and dances. Another individual claimed he could not work as a salesman due to lack of motivation, drive, and concentration. However, investigation of his activities outside work revealed a tenacious and time consuming pursuit of litigation against his ex-wife after an acrimonious divorce. He was so enraged at what he perceived as the unfairness of the legal system (because judgments went against him) that he spent a considerable amount of effort and time in pursuing appeals in court. This involved producing detailed appeals, which required intact cognitive skills and persistence. Functioning Well Except in a Particular Line of Work As alluded to earlier, this is particularly the case in physicians who have an own-occupation policy. The previously mentioned cardiologist made a claim that he could not work as a cardiologist while at the same time he was working well as a bariatric physician. During the claim period in which he said he could not concentrate well enough to be a cardiologist, he studied for, took, and passed the Bariatric board examination. He was performing all the functions of a physician but argued that he could not perform the functions of a cardiologist because of concentration and future decompensation reasons. Noncompliance With Treatment Noncompliance includes refusal to see the appropriate professionals (eg, seeing general practitioners rather than psychiatrists), refusal to take or persist with medications, refusal to follow recommendations to see specialists, gaps in treatment due to missed office visits, or not scheduling office visits. This also includes an unwillingness to adhere to medication regimens or persist with medications for the slightest of reasons. Most psychiatrists are aware that virtually all psychotropic medications do produce some side effects in the first few weeks of treatment and that, given time, patients can usually adjust to and tolerate side effects. Some claimants go on and off different medications every few days claiming that side effects prevent them from continuing with any one medication for an adequate period of time and claiming poor response to treatment. Surveillance Surveillance can provide objective evidence of behavior that is incongruent with claims. Even though this is not quite as obvious as in other specialties (such as with back claimants who are seen carrying out activities that a real back injury would preclude), surveillance does sometimes reveal behavior outside treatment and examination situations, that strongly suggest exaggeration or faking. An example is an individual who made a claim to an independent examiner that he was homebound, anhedonic, and socially withdrawn. Contemporaneously-made surveillance tapes revealed that the claimant had an active social life which included going out to dinner on a yacht with friends as well as meeting business acquaintances in local coffee shops. He was seen to be cheerful, communicative, and gregarious on the surveillance tapes. Factors Arguing Against Malingering There are several factors that may indicate legitimacy of a claim. Aggressive Treatment Malingerers tend to shy away from treatment that is stigmatized as potent or potentially dangerous, such as electroconvulsive therapy or the use of antipsychotic medications or medications requiring monitoring for organ safety (such as hepatic function monitoring with divalproex). A willingness to accept and tolerate such interventions would argue against the presence of malingering. Objective Evidence The presence of documented concerns, symptoms, and complaints from the claimant and family members or from employers well before the issue of disability was raised also raises the threshold of suspicion for malingering. Obvious Losses The presence of an objectively significant and documented loss precipitating the onset of psychiatric symptoms (eg, the death of a child) suggests the validity of such symptoms. However, this does not stop an individual with some depression from grossly exaggerating the amount of his or her impairment. Self-Defeating Behavior Impaired judgement, impulsivity, and other symptoms due to psychiatric disorders frequently lead to behavior that imperils the safety, relationships, or financial well being of affected individuals. Thus, manic patients may spend foolishly and excessively to their monetary detriment, putting themselves or their family into debt and at times dire financial straits. This is to be contrasted with the carefully planned and executed schemes of an individual who engages in insurance fraud. When the scheme is detected and punished, such an individual may claim, as a means of mitigating the consequences, that the behavior was due to mania associated with bipolar disorder. Conclusion Malingering is a condition, not an illness or clinical disorder, in which there is intentional exaggeration and/or faking of symptoms or impairment for an external incentive. It can present as subtle or flagrant forms. Clinical decision making should utilize multiple data sources including interview of the claimant, records, collateral human sources of information, surveillance, and psychologic tests. The totality of the picture rather than any individual piece of data provides evidence for consistency with malingering, be it high, moderate, or minimal consistency. PP References 1. Carrol MF. Malingering in the Military. Psychiatr Ann. 2003;33(11)731-736. 2. Diagnostic and Statistical Manual of Mental Disorders. 4th ed text-rev. Washington, DC: American Psychiatric Association; 2000:739. 3. Rogers R. Clinical Assessment of Malingering and Deception. 2nd ed. New York, NY: Guilford Press; 1997. 4. Slick TJ, Sherman MS, Iverson GL. Diagnostic criteria for malingered neurocognitive dysfunction: proposed standards for clinic practice and research. Clin Neuropsychol. 1999;13(4):545-561. 5. Bianchini KJ, Greve KW, Glynn G. On the diagnosis of malingered pain-related disability: lessons from cognitive malingering research. Spine J. 2005:5(4);404-417 6. Miller HA. Miller Forensic Assessment of Symptoms Test Professional Manual. Odessa, FL: Psychological Assessment Resources; 2001. 7. Mittenberg W, Patton C, Canyock EM, Condit DC. Base rates of malingering and symptom exaggeration. J Clin Exp Neuropsychol. 2002;24(8):1094-1102. 8. Larrabee GJ. Detection of malingering using atypical performance patterns on standard neuropsychological tests. Clin Neuropsychol. 2003;17(3):410-425. 9. Rosenfeld B, Sands SA, Van Gorp WG. Have we forgotten the base rate problem? Methodological issues in the detection of distortion. Arch Clin Neuropsychol. 2000;15(4):349359. 10. Public Attitude Monitor (Survey). Oak Brook, IL: Insurance Research Council; 1992. 11. Public Attitude Monitor (Survey). Oak Brook, IL: Insurance Research Council; 1993. 12. Trueblood W, Schmidt M. Malingering and other validity considerations in the neuropsychological evaluation of mild head injury. J Clin Exp Neuropsychol. 1993;15(4):578590. 13. Frederick R, Sargaty S, Johnston JD, et al: Validation of a detour response bias on a forcedchoice test of non-verbal ability. Neuropsychol. 1994;8(1):118-125. 14. Rogers R, Harrell EH, Liff CD. Feigning neuropsychological impairment: a critical review of methodological and clinical considerations. Clin Psychol Rev. 1993;13(3):255-274. 15. Binder LM. Assessment of malingering after mild head trauma with the Portland Digit Recognition Test. J Clin Exp Neuropsychol. 1993;15(2):170-182. 16. Ekman P. Telling Lies: Clues to Deceit in the Marketplace, Politics, and Marriage. New York: W.W. Norton; 1985. 17. Rosen J, Mulsant BH, Bruce ML, Mittal V, Fox D. Actors’ portrayals of depression to test interrater reliability in clinical trials. Am J Psychiatry. 2004;161(10):1909-1911. 18. Workshop: Detecting deception from demeanor in forensic psychiatry. Workshop at: Annual Meeting of the American Academy of Psychiatry and the Law; October 21-24, 2004; Scottsdale, AZ. 19. Cripe LI. Limitations of records reviews. Division of Clin Neuropsychol. 2002;40(20):1. 20. Reynolds CR. Common sense, clinicians, and actuarialism in the detection of malingering during head injury litigation. In: Reynolds CR, ed, Detection of Malingering During Head Injury Litigation. New York, NY: Springer; 1997:261-286. 21. Sreenivasan S, Eth S, Kirkish P, Garrick T. A practical method for the evaluation of symptom exaggeration in minor head trauma among civil litigants. J Am Acad Psychiatry Law. 2003;31(2):220-231. 22. Mittenberg W, DiGiulio DV, Perrins, Bass AE. Symptoms following mild head injury: expectation as aetiology. J Neurol Neurosurg Psychiatry. 1992;55(3):200-204. 23. Binder LM, Rohling ML. Money matters: a meta-analytic review of the effects of financial incentives on recovery after closed head injury. Am J Psychiatry. 1996;153(1):7-10. 24. Daubert v. Merrell Dow Pharmaceuticals, 509 U.S. 579 (1993). 25. Hom J, Denny RL. Detection of Response Bias in Forensic Neuropsychology. New York, NY: Haworth Medical Press; 2002. 26. Wechsler D. Wechsler Adult Intelligence Scale. 3rd ed. San Antonio, TX: Psychological Corporation; 1997. 27. Wechsler D. Wechsler Memory Scale. 3rd ed. San Antonio, TX: Psychological Corporation; 1997. 28. Mittenberg W, Puentes GA, Patton C, Canyock EM, Heilbronner RL. Neuropsychological profiling of symptom exaggeration and malingering. J Forensic Neuropsychol. 2002;3(1-2):227240. 29. Langeluddecke PM, Lucas SK. Quantitative measures of memory malingering on the Wechsler Memory Scale-third edition in mild head injury litigants. Arch Clin Neuropsychol. 2003;18(2):181-197. 30. Hathaway SR, McKinley JC. The Minnesota Multiphasic Personality Inventory, 2nd ed. Minneapolis, MN: University of Minnesota Press; 1989. 31. Pope KS, Butcher JN, Seelen J. The MMPI, MMPI-2, and MMPI-A in Court: a Practical Guide for Expert Witnesses and Attorneys. Washington, DC: American Psychological Association; 1993. 32. Millon T. Millon Clinical Multiaxial Inventory-3 Manual. Minneapolis, MN: National Computer Systems; 1994. 33. Rogers R, Bagby RM, Dickens SE. Structured Interview of Reported Symptoms Professional Manual. Odessa, FL: Psychological Assessment Resources; 1992. 34. Tombaugh TN. The Test of Memory Malingering. Toronto, Canada: Multi-Health Systems; 1996. 35. Binder LM. Portland Digit Recognition Test Manual. Beaverton, OR: Laurence Binder; 1993. 36. Slick D, Hopp G, Strauss E, Thompson GB. Victoria Symptom Validity Test Professional Manual. Odessa, FL: Psychological Assessment Resources; 1997. 37. Green P. The Word Memory Test. Edmonton, Canada: Green’s Publishing Company; 2003. 38. Lezak MD, Howieson DB, Loring DW. Neuropsychological Assessment. 4th ed. New York, NY: Oxford University Press; 2004. 39. Heilbrun K. Forensic Mental Health Assessment. New York, NY: Oxford University Press; 2002. Dr. Samuel is president and medical director at the Boca Raton Psychiatric Group in Florida. Dr. Mittenberg is professor at the Center for Psychological Studies at Nova Southeastern University in Fort Lauderdale, Florida. Disclosure: Dr. Samuel is on the speaker’s bureau of Pfizer. Dr. Mittenberg reports no affiliation with or financial interest in any organization that may pose a conflict of interest. Acknowledgments: Drs. Samuel and Mittenberg would like to thank Neviana Nenov, MD, for her help in preparing and reviewing this manuscript. Please direct all correspondence to: Roger Z. Samuel, MD, President and Medical Director, Boca Raton Psychiatric Group, 7284 W. Palmetto Park Rd, Suite 201S, Boca Raton, FL 33433; Tel: 561-368-8998; Fax: 561-392-9170; E-mail: brpg7284@lycos.com.