Supplemental Material 1 – Diagnosis and Resolution of PPOI
advertisement
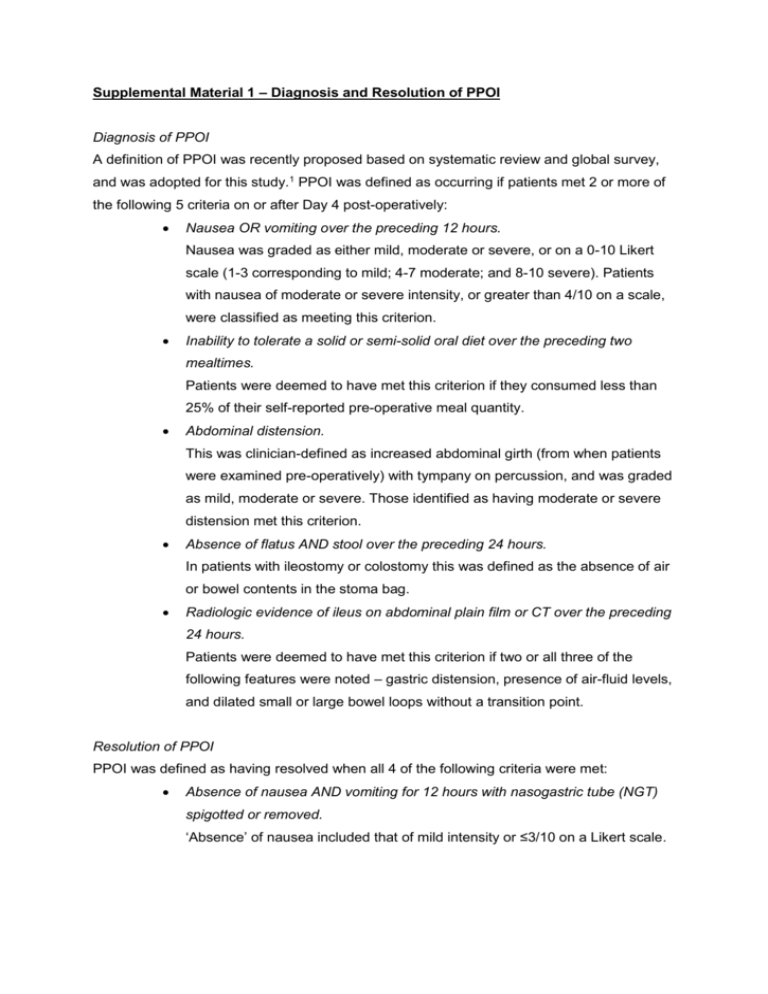
Supplemental Material 1 – Diagnosis and Resolution of PPOI Diagnosis of PPOI A definition of PPOI was recently proposed based on systematic review and global survey, and was adopted for this study.1 PPOI was defined as occurring if patients met 2 or more of the following 5 criteria on or after Day 4 post-operatively: Nausea OR vomiting over the preceding 12 hours. Nausea was graded as either mild, moderate or severe, or on a 0-10 Likert scale (1-3 corresponding to mild; 4-7 moderate; and 8-10 severe). Patients with nausea of moderate or severe intensity, or greater than 4/10 on a scale, were classified as meeting this criterion. Inability to tolerate a solid or semi-solid oral diet over the preceding two mealtimes. Patients were deemed to have met this criterion if they consumed less than 25% of their self-reported pre-operative meal quantity. Abdominal distension. This was clinician-defined as increased abdominal girth (from when patients were examined pre-operatively) with tympany on percussion, and was graded as mild, moderate or severe. Those identified as having moderate or severe distension met this criterion. Absence of flatus AND stool over the preceding 24 hours. In patients with ileostomy or colostomy this was defined as the absence of air or bowel contents in the stoma bag. Radiologic evidence of ileus on abdominal plain film or CT over the preceding 24 hours. Patients were deemed to have met this criterion if two or all three of the following features were noted – gastric distension, presence of air-fluid levels, and dilated small or large bowel loops without a transition point. Resolution of PPOI PPOI was defined as having resolved when all 4 of the following criteria were met: Absence of nausea AND vomiting for 12 hours with nasogastric tube (NGT) spigotted or removed. ‘Absence’ of nausea included that of mild intensity or ≤3/10 on a Likert scale. Ability to tolerate a solid or semi-solid oral diet at the preceding mealtime. More than 25% of self-reported pre-operative meal quantity was to have been consumed to meet this criterion. Absence of abdominal distension. ‘Absence’ of distension included those with clinician-determined mild distension as described above. Passage of flatus OR stool over the preceding 24 hours. In participants with a stoma this was defined as the presence of air or bowel contents in the stoma bag. Supplemental Material 2 – Standardised management guidelines for PPOI The clinical management of trial participants conformed to standardised evidence-based recommendations as follows.2 A NGT was inserted if vomiting was a feature. This was initially set to free drainage, and then spigotted with 6-hourly aspirates when output was less than 600mls/24 hours. When output fell below 300ml/24 hours the NGT was removed. Electrolytes (specifically sodium, potassium, magnesium and calcium) were monitored and corrected on a daily basis. Analgesia prescription was reviewed with weaning of opiates and progressive substitution with regular paracetamol, regular tramadol and regular or as-required non-steroidal inflammatory drugs. Opiates were reserved for breakthrough pain only. Maintenance fluid therapy of Dextrose 4% and Saline 0.18% with KCl was prescribed at 1ml/kg/hr. NGT losses or vomits greater than 500mls were replaced ml for ml with 0.9% Saline + 30mmol KCl at a maximum infusion rate of 330ml/hr. Fluid therapy in participants with clinical dehydration, acute renal impairment, fluid overload or haemodynamic instability was left to the discretion of the surgical team. If feasible, patients were asked to ambulate at least three times a day with assistance as necessary. Parenteral nutrition (PN) was commenced if patients were unable to sustain adequate oral intake for more than 7 days, or after 5 days if nutritionally deplete. PN was discontinued when participants were tolerating an oral diet. The PN prescription was determined by the nutritional support team. Nursing and medical staff were made aware of the presence of these guidelines via formal interactive ward-based teaching sessions and one-on-one reminders to involved personnel. Additionally, a single-page summary of guidelines was placed in the clinical notes folder of participants upon recruitment. References 1. 2. Vather R, Trivedi S, Bissett I. Defining postoperative ileus: results of a systematic review and global survey. J Gastrointestin Surg 2013; 17:962-972. Vather R, Bissett I. Management of prolonged post‐operative ileus: evidence‐based recommendations. Aust N Z J Surg 2013; 83:319-324.