- The Portland Clinic
advertisement
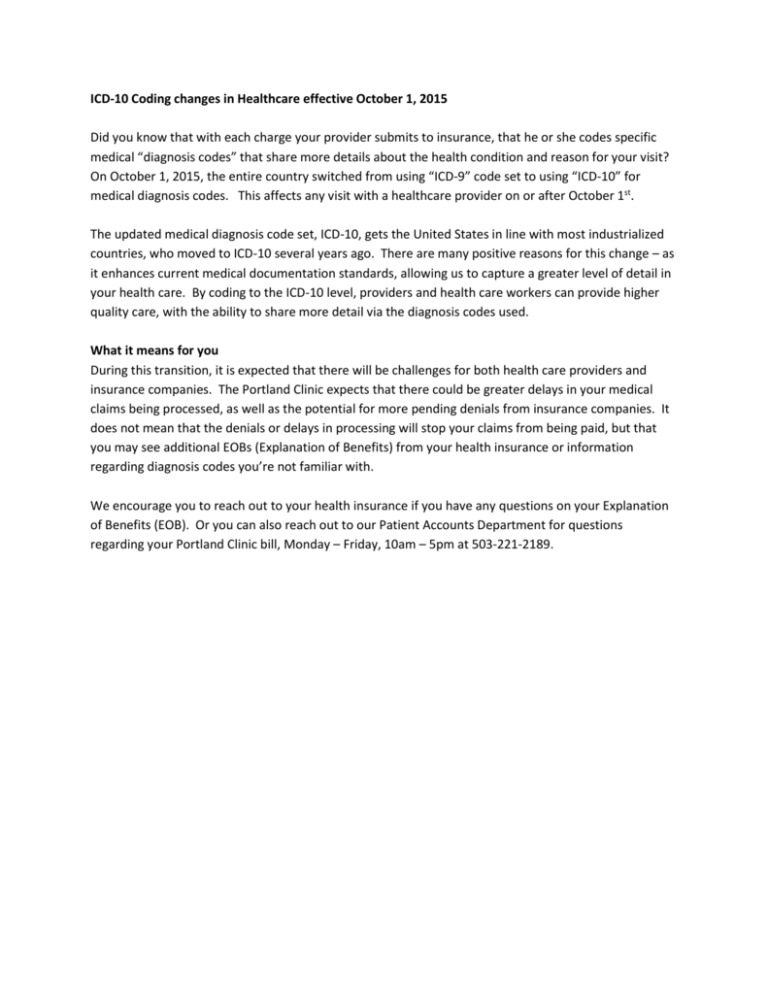
ICD-10 Coding changes in Healthcare effective October 1, 2015 Did you know that with each charge your provider submits to insurance, that he or she codes specific medical “diagnosis codes” that share more details about the health condition and reason for your visit? On October 1, 2015, the entire country switched from using “ICD-9” code set to using “ICD-10” for medical diagnosis codes. This affects any visit with a healthcare provider on or after October 1st. The updated medical diagnosis code set, ICD-10, gets the United States in line with most industrialized countries, who moved to ICD-10 several years ago. There are many positive reasons for this change – as it enhances current medical documentation standards, allowing us to capture a greater level of detail in your health care. By coding to the ICD-10 level, providers and health care workers can provide higher quality care, with the ability to share more detail via the diagnosis codes used. What it means for you During this transition, it is expected that there will be challenges for both health care providers and insurance companies. The Portland Clinic expects that there could be greater delays in your medical claims being processed, as well as the potential for more pending denials from insurance companies. It does not mean that the denials or delays in processing will stop your claims from being paid, but that you may see additional EOBs (Explanation of Benefits) from your health insurance or information regarding diagnosis codes you’re not familiar with. We encourage you to reach out to your health insurance if you have any questions on your Explanation of Benefits (EOB). Or you can also reach out to our Patient Accounts Department for questions regarding your Portland Clinic bill, Monday – Friday, 10am – 5pm at 503-221-2189.