Example
advertisement
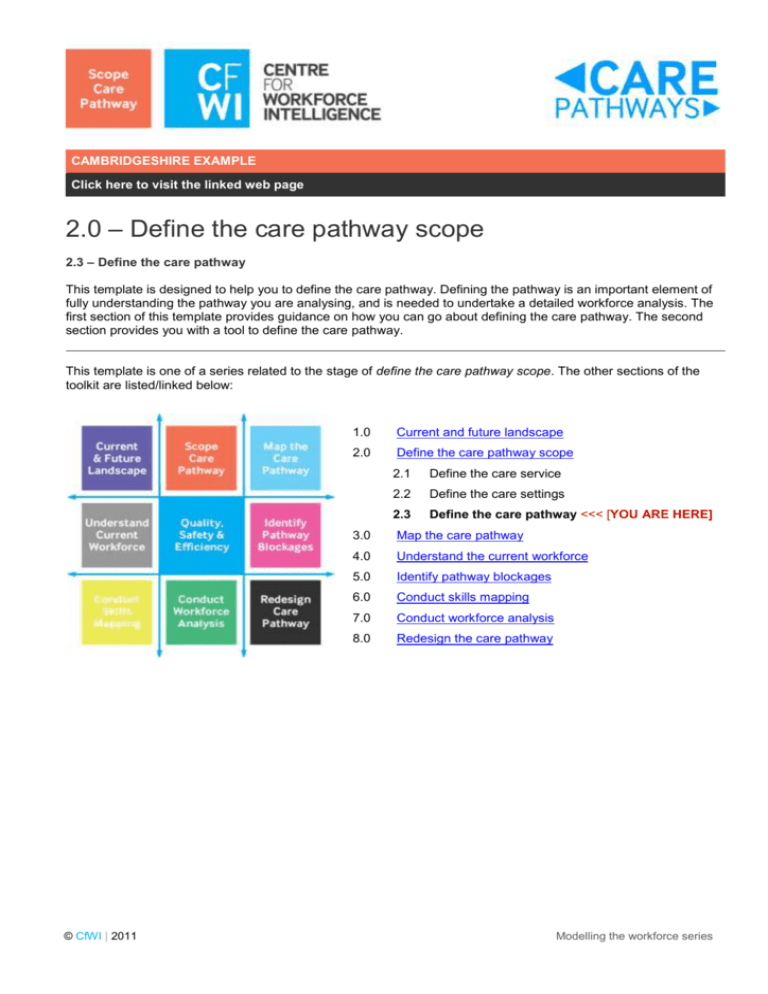
CAMBRIDGESHIRE EXAMPLE Click here to visit the linked web page 2.0 – Define the care pathway scope 2.3 – Define the care pathway This template is designed to help you to define the care pathway. Defining the pathway is an important element of fully understanding the pathway you are analysing, and is needed to undertake a detailed workforce analysis. The first section of this template provides guidance on how you can go about defining the care pathway. The second section provides you with a tool to define the care pathway. This template is one of a series related to the stage of define the care pathway scope. The other sections of the toolkit are listed/linked below: © CfWI | 2011 1.0 Current and future landscape 2.0 Define the care pathway scope 2.1 Define the care service 2.2 Define the care settings 2.3 Define the care pathway <<< [YOU ARE HERE] 3.0 Map the care pathway 4.0 Understand the current workforce 5.0 Identify pathway blockages 6.0 Conduct skills mapping 7.0 Conduct workforce analysis 8.0 Redesign the care pathway Modelling the workforce series Introduction DESCRIPTION OF THE STEP Analysis of patient/service user journeys between different care states has illustrated the diversity of these journeys, and the need to formalise and standardise them. Since the purpose of this toolkit is to model the workforce implications of care pathways, it is critical to have a clear definition of the care pathway in question. Care pathways are: routes that different patients/service users take through care settings and models of care defined by a combination of patient/service user choice, clinical need and evidence-based practice inclusive of the competencies needed to deliver that care supported by clinical protocols, which are documented agreements on diagnostics and treatments used at different steps of the care pathway. Care pathway definition: A care pathway is a defined sequence of activities, including access, diagnostic, therapeutic and supportive. These embrace the set of needs surrounding specific patient/service user groups. The workforce and the setting in which it operates can be configured and evaluated to deliver consistent, safe, effective and efficient services, thereby defining the patient's/service user’s experience of health and social care. Patient needs may be physical, mental or social, and their conditions may be high volume, high cost, complex or high risk. The setting for care delivery includes hospitals, the community, or new units/types of provision which could be developed. For more information about how to model your care pathway please refer to the following guidance: http://www.institute.nhs.uk/ http://www.mapofmedicine.com/ http://www.nice.org.uk/ RELEVANCE TO WORKFORCE To perform effective workforce modelling, each pathway must be carefully defined. There may be merit in extending the template to capture the primary (success) flow and exception or alternative flows through the pathway, before a process modelling stage. © CfWI | 2011 Modelling the workforce series The template DESCRIPTION OF THE TEMPLATE This template is a Microsoft Word table that allows you to clearly define the care pathways that you are analysing. TEMPLATE The following table should be used to define the care pathway you are modelling. Area Information Description The purpose of the integrated discharge care pathway is to ensure patients are discharged from hospital in a timely manner and receive the care and support that they need once they have returned to the community/or moved to another care setting. Desired outcomes include: reduced length of hospital stay reduced number of delayed discharges improved patient experience. Scope The integrated discharge pathway has been defined as: pre-admission to 6 weeks post-acute discharge for elective admission to 6 weeks post-acute discharge for non-elective. A 6 week post discharge period was chosen to ensure any problems with delivering care in the community, or appropriateness of place the patient/service user has been discharged to, are captured. Primary actors Patient/service user – wants to be discharged in a timely manner. They want to be seamlessly transferred between care services and receive a joined-up service. Strategic discharge planning manager – to ensure patients are discharged effectively and receive the care and support they require once they are back in the community; to keep delayed discharges are kept to a minimum. Discharge planning specialist nurses – to plan effectively the health care people need require once they are back in the community. Social workers – to plan effectively the support people require once they are back in the community. Care managers – to plan effectively the support people require once they are back in the community. Admin team – to provide support to the discharge planning team to ensure that they can effectively source and arrange care packages for people who require further support upon discharge; to enter relevant information into SWIFT. Care purchasing coordinators – to source the necessary care package and update © CfWI | 2011 Modelling the workforce series Area Information information on SWIFT. Secondary actors Occupational therapists – to deliver occupational therapy support to a person to help them with activities of daily living, promoting independence and a safer environment; to conduct assessments that feed into determining what care packages are required once a person is discharged. Physiotherapists – to deliver physiotherapy support to a person to help improve their mobility; to conduct assessments that feed into determining what care packages are required once a person is discharged. Districts nurses – to liaise with the discharge planning specialist nurses/ward nurses upon discharge to understand the person’s care needs in the community. Ward manager – to effectively discharge patients from the ward to prevent bed blocking and increase patient satisfaction. Hospital and community management – to minimise the number of delayed discharges reported to the Primary Care Trust (PCT); to reduce length of stay and increase patient satisfaction. Locality team – to liaise with the discharge planning team to arrange for re-ablement care in the community. GPs – to receive discharge letter and follow-up with patient/service user upon discharge. Pharmacists - to prepare To Take Outs (TTOs); to dispense discharge medications and prepare Medicine Administration Record (MAR) charts. Hospital transport – to liaise with ward staff to book transport/change transport needs. 1 Triggers The pathway begins once a patient/service user is referred to the discharge planning team. This is done as soon as it is known that they will require care and support in the community following discharge from hospital when the discharge risk assessment is populated and the N1 (section 2) is sent. Pre-conditions To enter the integrated discharge pathway, a patient/service user has a need for care and support once they have been discharged from hospital back to the community. This is assessed once the discharge risk assessment is populated. Post-conditions At the end of the pathway the patient has been discharged to an appropriate location in the community and is receiving the care and support that they require. The goal is to ensure that the patient/service user is not inappropriately readmitted and to ensure that they are receiving support in the community. Frequency On average, there are 349 complex discharge cases per month.1 Based on N2 data provided by the Discharge Planning Team. © CfWI | 2011 Modelling the workforce series Area Information Interactions The integrated discharge pathway could interact with every care pathway that involves a hospital admission and with every care pathway in the community. Priorities The purpose of the integrated discharge care pathway is to ensure patients are discharged from hospital in a timely manner and receive the care and support that they need once they have returned to the community/or moved to another care setting. Desired outcomes include: reduced length of hospital stay reduced number of delayed discharges improved patient experience. © CfWI | 2011 Modelling the workforce series

![Major Change to a Course or Pathway [DOCX 31.06KB]](http://s3.studylib.net/store/data/006879957_1-7d46b1f6b93d0bf5c854352080131369-300x300.png)