When to use the EZ-IO
advertisement

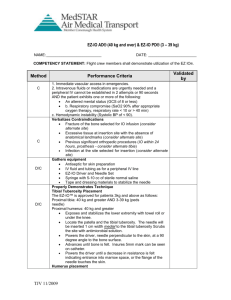
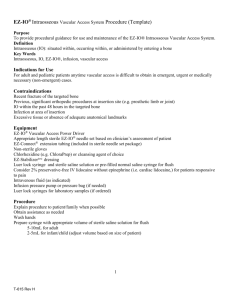
E Z - I O UPDA T E f or DA S The use of intraosseous (IO) access devices has become a vital tool in the pre-hospital environment over the last 4-5 years. In situations where intravenous access is difficult or unable to be obtained, IO access is able to provide a route for fluid and medication administration. This course will review the use of the EZ-IO system, including indications, contraindications, and the “6 Rights” of the EZ-IO. Content of this course is based on the current recommendations from Vidacare and the current Region 5 protocols. ANATOMY REVIEW Classification of bones: There are 206 named bones comprising the human skeleton. Bones are classified by their shapes either long, short, flat, or irregular. Long bones are named for their overall shape, not their overall size. The phalanges are considered long bones even though they are quite short. Long bones are longer than they are wide consisting of a shaft and two ends. The shaft of the bone is called the diaphysis. This forms the long axis of the bone. It is formed from a thick layer of compact bone that surrounds a medullary or marrow cavity. The epiphyses are the bone ends. They are often more expanded that the diaphysis and contain spongy bone. All limb bones excluding the bones of the wrists and ankles are long bones. Short bones are roughly cube shaped. Examples include the bones of the wrists and ankles. Sesamoid bones are special types of bones that form within tendons. The patella is an example. The function of some sesamoid bones is to alter the direction of the pull of a tendon. Flat bones are thin and somewhat curved. Examples include the sternum, scapulae, ribs, and bones of the cranium. Irregular bones have complicated shapes that do not fit in the other classes. We will focus our attention on the long bones. Every bone has a dense outer layer of compact bone which surrounds spongy or cancellous bone. Spongy bone is a honeycomb of osseous spicules called trabeculae. Within the spaces of the trabeculae is red or yellow bone marrow. The humerus: Focusing our attention on the proximal humerus, there is a smooth hemispherical head which articulates with the scapula so that it hangs freely to one side. Immediately inferior to the head is a slight constriction called the anatomical neck. Inferior to the anatomical neck are the laterally positioned greater tubercle and the medially positioned lesser tubercle. Separating the tubercles is the intertubercular sulcus. This sulcus guides the biceps tendon to its attachment point. It also houses a branch of the humeral circumflex artery. Just distal to the tubercles is the surgical neck, so called because it is the most frequently fractured site of the humerus. See the picture below for reference. The tibia: The tibia recieves its weight from the body via the femur and trasmits this weight to the foot. It is second only to the femur is size and strength. At its proximal end are the lateral and medial condyles. These articulate with the corresponding condyles of the femur. These condyles are spearated by the intercondylar eminance. Inferior to the condyles on the anterior surface of the tibia is the tibial tuberosity, to which the patellar ligamnet attaches. The shaft of the tibia is a tirangular shape. Neither its anterior border or its medial surface are covered with muscles. They can easily be palpated just deep to the skin over its entire length. Distally, the tibia is flat where it articulates with the talus bone of the foot. Medial to that joint is a projection called the medial malleolus. See the picture below for reference. I N DI C AT O NS: Intraosseous access is indicated for adults (≥ 40 kg) and pediatric patients (3-39 kg) anytime vascular access cannot be established after two attempts or 90 seconds. The patient must also be experiencing one or more of the following: altered mental status respiratory compromise hemodynamic instability status epilepticus refractory to IM medication administration. If IV access is not readily available, IO access may be considered prior to any IV attempts in the following situations: medical or traumatic cardiac arrest signs and symptoms of hypoperfusion (profound hypotension, tachycardia and altered mental status) a patient in extremis needing IMMEDIATE medication administration C O N T RA INDI CAT IO NS: The use of the EZ-IO device is contraindicated, and an alternate site should be considered, in the following situations: Fracture to the target site (proximal, distal tibia or proximal humerus) Previous orthopedic procedure (i.e. knee replacement) to target site Prosthetic limb or joint Intraosseous access within the past 24 - 48 hours at the target site Infection at the insertion site Inability to locate landmarks or excessive tissue over the insertion site History of osteogenesis imperfecta Region 5 protocol limits the use of the EZ-IO system to pediatrics above 3 kilograms. Vidacare recommends that a manual IO device (e.g. Illinois needle) be used if a pediatric patient is less than 3 kilograms. Region 5 protocols do not offer any recommendations in such a case. It is suggested that on-line medical direction be consulted. THE SIX RIGHTS OF THE EZ-IO Vidacare had developed the “Six Rights” of the EZ-IO in order to help providers remember key items to successful placement. These Six Rights are: 1. 2. 3. 4. 5. 6. Right Assessment Right Site Right Needle Right Flush Right Comfort Right Monitoring When these Six Rights are followed, proper placement and flow are more likely to be achieved. We will look at each item in detail. T HE RI G HT A SSE SS ME NT When to use the EZ-IO: The EZ-IO can be used for adult and pediatric patients anytime when vascular access is difficult to obtain in emergent, urgent, or medically necessary situations. A common misunderstanding of IO access is that it takes a long time for fluids, medications, or blood infused to reach the central circulation. This is false. Scientific studies have proven any fluid infused into the intraosseous space enters the central circulation within just a few seconds. The EZ-IO is an immediate option that can serve as your main line. It may also serve as a bridge to peripheral, PICC or central venous access. In accordance with Region 5 protocols, providers should assess the patient and consider using the EZ-IO after two attempts at IV access or 90 seconds have elapsed trying to establish IV access or when a patient exhibits signs and symptoms of: Altered mental status Respiratory compromise Hemodynamically unstable Status epilepticus refractory to IM medication administration Other considerations include the following: Patients with minimal risk factors (discussed later) The need for vascular access in less than 10 seconds to allow for proper pharmacology administration A patient requiring large fluid volume infusions Such presentations include but are not limited to: Shock trauma Cardiac resuscitation, arrhythmia, myocardial infarction, congestive heart failure, or chest pain Hypothermia Neurological - status epilepticus, stroke, coma, head injury Respiratory - respiratory arrest, status asthmaticus Hematologic – systematic hemophiliac crisis, sickle cell crisis Metabolic crisis - DKA, diabetic shock Circulatory crisis – dehydration, end stage renal disease, dialysis Once the decision is made to gain IO access, assess the chosen site for any of the following five site contraindications for using EZ-IO at that location: Prosthesis or previous orthopedic procedures near the insertion site: An easy rule of thumb to use is if the patient has a surgical scar over a joint; assume there is a titanium appliance within the joint. DO NOT USE THE EZ-IO at that location. The EZ-IO needle sets cannot penetrate titanium. Simply move to another FDA and/or Region 5 approved insertion site and assess that site for use. Trauma or Fracture (in the target bone): If there is a fracture (or suspected fracture) in the bone in which the EZ-IO is to be placed, an alternate site must be chosen. Fluid will follow the path of least resistance. When an IO is placed in a fractured bone, the fluid will extravasate into the surrounding tissue through the fracture. This can lead to complications including compartment syndrome. If a tibial fracture is suspected, both the proximal and distal sites will be contraindicated as they share the same common pathway inside the bone. However, if the patient has a fractured femur but an intact tibia, the tibial sites COULD be used as they are totally separate bones. The circulation from lower leg should be assessed to judge the appropriateness of using the lower extremity for EZ-IO. Inability to locate landmarks (e.g. due to excessive tissue): If the clinician is unable to locate the landmarks for an insertion site for any reason (including excess adipose tissues), select an alternate insertion site where you can identify the bony landmarks. Infection at the insertion site: Vidacare and Region 5 do not recommend inserting the EZ-IO through any visible or documented infection or inflamed region at the insertion site. IO access within past 48 hours (in the target bone): Healing from IO insertion generally takes 48 hours and is defined as the point where another IO can be safely placed at the same anatomical site. By that time, fibrin formation and clotting are sufficient to prevent extravasation through the previous IO puncture. Complete healing, to the point where X-ray can no longer detect the hole, usually takes several days or weeks. These five safety limitations are critical assessment considerations prior to insertion of an IO device. T HE RI G HT SIT E Once you have decided that a patient will benefit from the EZ-IO, the first step is to identify the right site for needle placement. The FDA has approved three sites that the EZ-IO can be placed: the proximal humerus, proximal tibia, and the distal tibia. Note that the Region 5 protocols do not list the proximal humerus as an insertion site. It is important to properly locate these sites to ensure successful insertion. Pr o x i mal Hu mer u s : The greatest advantage of using the humeral site is flow rate. The close proximity of the greater tubercle of the humerus to the heart ensures rapid infusion of medications into the central circulation. Average flow rates of five liters per hour can be achieved using the humeral site. The proximal humerus has been reported as being less painful site to access compared to either of the tibial sites. This is also the preferred site for patients who are responsive to pain. The proximal humerus insertion site is located directly on the most prominent aspect of the greater tubercle. To properly landmark this site, ensure that the patient’s hand is pronated (palm down) and resting on the umbilicus. The elbow must be adducted (close to the body). This ensures that the intertubercular sulcus is rotated medially protecting the structures within. Slide your thumb up the anterior shaft of the humerus until you feel the base of the greater tubercle, this is the surgical neck. Approximately 1 cm above the surgical neck is the insertion site. Access the link below to watch a video on how to properly landmark this site as well as live insertions. https://www.youtube.com/watch?v=Wu-KVibUGNM Pr o x i mal T i bi a Adults: The proximal tibia insertion site is approximately 2 cm below the patella and approximately 2 cm medial to the tibial tuberosity. Remember: “Big Toe IO” means to look on the big toe side of the leg for the tibial plateau (the flat spot). Flow rates ranging from 350 mL – 3300 mL per hour within pressures of 300 mmHg have been achieved in the proximal tibia. Pediatrics: The pediatric insertion site at the proximal tibia is the same for adults. The tibial tuberosity is not palpable on infants and some small children less than two years old. The proximal tibia insertion site in pediatrics is approximately 2 cm or 2 fingerbreadths below the patella and approximately 1 cm medial to the tibial tuberosity. In small children, generally under the age of two, if the tibial tuberosity cannot be palpated, locate the distal aspect of the patella, move approximately 2 cm distally and then medially to the flat aspect of the tibia. Di s t al T ib i a The distal tibia insertion site is located approximately three centimeters or three fingerbreadths proximal to the most prominent aspect of the medial malleolus. Place one finger directly over the medial malleolus; move approximately 3 cm proximal and palpate the anterior and posterior borders of the tibia to assure that your insertion site is on the flat center aspect of the bone. Again; “Big Toe IO”. Note: for pediatric patients, the distance is less. T HE RI G HT NEE DLE Selecting the proper needle is just as important as selecting the site. EZ-IO needles come in three sizes: 15mm (pink), 25mm (blue), and 45mm (yellow). All three needle sets are 15 ga needles. A common misconception is that the patient’s age should be the lone deciding factor when selecting the proper length of needle. Instead of age, the amount of tissue at the insertion site should be used to determine the correct length of needle. One way to determine the depth of tissue is to palpate the insertion site with your finger or thumb. If there is a small amount a tissue, like that over your knuckle, a shorter needle will be needed. If the tissue depth is excessive, similar to pressing your finger or thumb over the femur, then a longer needle is needed. The 45mm needle is recommended as the primary set for proximal humerus site for patients over 40kg (90lbs). Another way to confirm proper needle selection is by using the 5mm mark on the EZ-IO needle set. With the needle attached to the driver, insert the needle through the skin until the tip rests against the bone at a 90 degree angle. Look at the needle to assure that you can visualize at least one black line above the surface of the skin. If you cannot see a black line, the needle set selected is too short to reach the medullary space appropriately. Remove the current needle set, discard and use the next larger size. See the picture below for reference. Pr o p er i n sert i on Please note that with all patients, minimal pressure should be placed on the driver during insertion. This is especially true with pediatric patients. With softer and smaller bones, special care must be taken during insertion to avoid excessive pressure and recoil. Recoil can occur when the clinician feels the lack of resistance upon entry into the medullary space and inadvertently pulls back on the driver. This recoil may displace the needle set from the medullary space. After ensuring the proper site and the proper needle, it is now time to insert the EZ-IO needle. First assemble all of the required components. This includes the EZ-IO driver, selected needle set, Betadine swaps or alcohol preps, 2% lidocaine, and saline flushes. Inspect the needle set ensuring all the components are present and not damaged. Open the EZ-Connect tubing and prime the extension set with 2% preservative free Lidocaine, if the patient is conscious. If the patient is allergic to lidocaine or is unconscious, prime the extension set with 0.9% normal saline. In either case, leave the syringe attached. Next clean the selected site with copious amounts of Betadine or alcohol preps. Betadine is preferred if available provided the patient is not allergic to iodine products. If time permits, the site should be swabbed three separate times in ever increasing outward circles using a fresh swab each time. Attach the needle set to the driver, this is held in place by a magnet in the needle. Remove the cap from the needle set by holding the cap and briefly activating the driver. This will unseat the cap and allow for easier removal. Insert the needle through the skin at a 90 degree angle until you feel the tip of the needle touch the bone. Verify that at least one black line is visible. Stabilize the extremity with your non-dominant hand. Hold the needle over the exact location and angle you plan to insert with. Gently and BEFORE PULLING THE TRIGGER, insert the needle set through the skin until you feel the tip of the needle touch the outer surface of the bone. Now, squeeze the trigger and apply gentle, steady pressure to insert needle. Let the driver cut through the bony cortex while continuing to hold the trigger ON. Once the insertion is completed secure the extremity to prevent movement and accidental dislodgement of the IO catheter. Adult: Be sure to “drive” the needle all the way thru cortex until the needle is seated with the hub flush against the skin. For the proximal humerus specifically, Vidacare recommends the 45 mm needle (yellow) on patients > 40 kilograms. Angle the needles set at 45 degrees to the anterior plane of the body and advance the needle in a posterior-medial direction (See picture below). Region 5 makes no recommendation for the use of the proximal humerus as an access site. Advance the needle set approximately 1 cm after contact with bone or after entry into medullary space. In the humeral site, the needle set should be advanced until catheter hub is against the skin. When using the proximal humerus, it is recommended the catheter is stabilized using the EZ-IO stabilizer. Pediatrics: Stop immediately when you feel the resistance change. This indicates entry into the medullary space and avoids penetrating the full thickness of the bone. ALWAYS USE CARE to ensure you have selected the appropriate size needle set based on tissue depth and when inserting past the sensation of pressure change or loss of resistance. While holding the hub, pull the driver away from the needle, unscrew (counter clockwise) the needle from the hub and remove it, and immediately place the needle into the sharps box. Attach the EZ-Connect tubing to the needle. Confirmation of proper placement of the needle into the medullary space can be done several ways. Aspiration of marrow and/or blood into the EZ-Connect tubing can be used however, aspiration may not always occur, even if the EZ-IO needle has been placed properly. The absence of marrow/blood does not mean an unsuccessful placement. A firmly seated, stable needle and the ability to administer pressurized fluids without difficulty are indicators of successful placement. After insertion, check the following: That the needle is firmly seated Attempts to aspirate for blood or bone marrow were made There is no leaking around the site There are no indications of extravasation Secure the site using the provided EZ stabilizer and place the EZ-IO wrist band on the patient. T HE RI G HT FLUSH One of the most common mistakes made in IO placement is not properly flushing the IO site prior to administering fluids and/or medications. The intraosseous space is filled with a marrow that is held in place by a thick fibrin mesh. This fibrin mesh must be displaced in order to achieve optimal flow. The EZ-IO must be flushed rapidly with 10mL of saline to displace the fibrin network. The flush may have a similar sensation as pushing D50 through an IV site. Region 5 protocol recommend that the site be flushed with 20-50 mg of 2% preservative free Lidocaine for adults and 0.5 mg/kg for pediatrics. This flush is to be followed by a 10 mL flush of 0.9% normal saline for adults and a 5 mL flush for pediatrics. After flushing, the IO should flow easily and rapidly. Occasionally, additional saline flushes may be needed. If an IO site is not flowing properly, flush the site with another 10 mL saline flush to see if flow improves. Remember: NO FLUSH = NO FLOW. E n s u ri n g op ti mal f lo w r at es The final step in ensuring successful EZ-IO insertion is using the right amount of pressure to maintain proper fluid flow. The pressure inside the medullary space is approximately one-third that of the patient’s mean arterial pressure (systolic BP + 2(diastolic BP)/3). In order to achieve the best flow rate, the pressure of the fluids in the IV bag being administered must be higher than the pressure in the medullary space. Using a pressure infuser is the easiest way to increase fluid pressure. A blood pressure cuff may be used in lieu of a pressure infuser. T HE RI G HT CO MFO RT It is a misconception that insertion of the EZ-IO needle is the most painful part of the procedure. Many patients and volunteers noted that the pain from insertion is similar to that of insertion of an 18ga IV needle. The majority of the pain associated with IO insertion comes from the increased pressure inside to medullary space during fluid administration. One of the advantages of IO access is the fact that the medullary space is a non-collapsible space, but it is also non-expandable. When fluid is introduced in to IO space, pressure is placed on the visceral nerve endings causing pain. Proper pain management is an important part of using the EZ-IO system. Remember, many of the procedures we doing routinely cause pain, how we treat the discomfort is as important as the procedures. If a patient is responsive to pain, administration of 40mg (2mL) 2% preservative free Lidocaine, prior to flushing with saline will help reduce the pain associated with increased pressure in the medullary space. Lidocaine provides a local anesthetic effect to the area of insertion. In order for this to happen, the administration must be done slowly, over 15-30 seconds. T HE RI G HT MO NI T ORI NG Regular, periodic assessment is essential for safe IO access management. As a general rule, do what you would normally do with a peripheral IV site in terms of assessment, site care, flow rate intervention, and medication use. Verification of placement before each infusion is recommended. Ensure the site is intact on each assessment visit, the needle is securely in place, the patient identifiers are in place, the patient is comfortable and of course, the EZ-IO is working optimally. The EZ-IO must be removed 24 hours from the time of insertion. Remo vi n g E Z - I O Need l e The EZ-IO needle must be removed from the patient within 24 hours. To remove the EZ-IO needle from the patient, first clamp the EZ-Connect tubing and disconnect it from the EZ-IO needle. Attach a lure lock compatible syringe to the EZ-IO needle; this is used as a handle to aid in removal. Rotate the syringe and needle clockwise, to release the needle from the cortex, and pull straight out while continuing to rotate clockwise. DO NOT ROCK THE NEEDLE BACK AND FORTH. After rotating several times the needle should come completely out. There may by minor bleeding at the insertion site. Clean and dress the insertion site with an adhesive bandage or similar dressing. The EZ-IO needle must be removed from the patient within 24 hours. Havi n g I s su es ? If you ever have questions or problems with the EZ-IO system, Vidacare provides a 24 hour “hot line” to assist with clinical issues. In every EZ-IO needle set there is a fluorescent colored wrist band that should be attached to the patient. This wrist band alerts the receiving staff that the patient has an IO in place and when it was place. The 1-800 “hotline” number is also on the wrist band. The placement of an IO needle can be both safe and beneficial for patients in need of emergent vascular access. Remember the Six Rights of EZ-IO Placement: 1. 2. 3. 4. 5. 6. Right Assessment Right Site Right Needle Right Flush Right Comfort Right Monitor REFERENCES: BCMS. EZ-IO Update for Buncombe County EMS [Web page]. Retrieved from http://emsstaff.buncombecounty.org/inhousetraining/ez_io_Update/ez_io_overview.htm Hoehn, K., Marieb, E. (2007). Human Anatomy and Physiology 7th Edition. 178-180, 231-232, 242-244. Vidacare. The Clinical Principles of Successful Intraosseous Vascular Access [Powerpoint presentation]. Retrieved from: http://www.teleflex.com/en/usa/ezioeducation/EZ-IO-Clinical-PrinciplesNo-Vid-2014-2780.pptx. Vidacare. Clinical Principles to Successful IO Insertion EZ-IO Six Rights 5-30-12 (1) [Powerpoint presentation]. Retrieved from: www.teleflex.com/en/usa/ezioeducation/EZ-IO-Clinical-PrinciplesNo-Vid-2014-2780.pptx Region 5. (2013). Region 5 Paramedic Protocols