to reduce the risk of vascular access haemorrhage (VAH)
P140
IMPROVING THE SAFETY OF PATIENTS WITH AN ARTERIOVENOUS FISTULA OR GRAFT : TO
REDUCE THE RISK OF VASCULAR ACCESS HAEMORRHAGE (VAH)
Lynn Davies, Elaine Saunders (Dialysis access nurse specialists) Mike Stephens, Adel Ilham (Consultant surgeons)
University Hospital of Wales
Background
The Renal Association ( guideline 4.3: Vascular access surveillance ) suggests that these three steps: 1) look 2) feel
3) listen should be routine in the assessment of vascular access in that it becomes a routine part of the haemodialysis
(HD) nurse’s pyramid of inspections and assessment when caring wholly for a HD patient with a AVF/G as their access for HD.
Acute blood loss through an AVF/G can be life threatening to the patient (Patient safety project 2007-2014). In our unit a recent concern was of small number patients encountering a vascular access haemorrhage (VAH) in the community/home. Reasons were poor skin integrity and poor cannulation technique which had not been reported or dealt with early resulting in a sudden bleed from needle sites post dialysis. An investigation highlighted that there was no structured education to HD patients which would allow them learn to assess their AVF /G to identify the early signs and symptoms for deterioration in skin integrity.
Written information, regular education and assessment of the patient’s understanding of VAH was not available, unclear or not recorded. There was no clarity on what had been discussed with the patient or the family/carer. All patients in the haemodialysis units who had a functioning AVF/G were questioned, their response were noted and recorded on a surveillance chart.
It became apparent that a large proportion of the 74% of prevalent patients with an AVF/G were unaware of the risk of haemorrhage from their AVF/G and did not know what to do or who to contact should it occur.
AIMS
1.
Our aims were to implement a programme by involving the patient and or their carers in order empower them to take responsibility in the care of their AVF/G. Improving their understanding of the risk of haemorrhage enabled them to identify the sign and symptoms of a potential VAH. We wanted each patient /carer to physically be able to cope with a bleed and know who to ring or report the incident to.
2.
Secondly, HD staff needed to be alerted to their responsibility to identify any patient at risk of a bleed and to inform, assess and report any signs and symptoms of deterioration to the patient’s skin over the AVF/G.
3. Thirdly, was to improve the communication, written and verbal on the information given to patients by the
HD staff.
RESULT
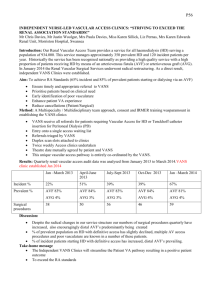
Clients with an AVF/G were all seen by the Dialysis Access Nurse specialists (DANS) who involved the HD unit staff looking after the patients for that session. In some instances a carer or nursing home were contacted where the patient was unable to comprehend or actually be able to press on the bleeding site. A surveillance form was created for each patient who allowed the DANS to keep a date of the consultation which included:
The name of the patient and the date it took place.
The condition of the skin over the fistula.
The cannulation technique used.
Did the patient understand how to care for the skin over the fistula /graft?
Did they know what to report: i.e if the skin was thin, broken, had white spots or aneurysms.
Did they know what to do if they had a small bleed from a needle site when in the community?
Did they know what to do if they had a severe bleed in the community?
Did they apply pressure to the needle sites post needle removal
The surveillance form is updated 6 weekly but allows the DANS to revisit if there is an immediate or ongoing issue.
This is now well embedded in to the care of this cohort of clients. Emergency bleeding information packs are part of the package now given to all patients stipulating the actions to take if a bleed from their AVF/G occurred in the community.
Access link nurses in the units are reminded regularly in meetings with the DANS to inform their HD staff of their obligation to assess the AVF/G and to educate and assess their patient’s understanding and ability to cope with a bleed.
Conclusion
By involving the patient and their cares in the education process their knowledge of coping with a bleed be it small or severe has improved immensely. All new and old patients with AVF/G are now part of a regular surveillance programme which now includes assessing their capability and understanding of vascular access haemorrhage this is supported and monitored by the DANS during their HD unit visits. Access link nurses are encouraged to communicate with other staff and have regular 3 monthly meetings with the DANS. Communication with the patient and the HD staff has improved in this matter both written and verbally.