Understanding-Health-Insurance-in-2014-and
advertisement
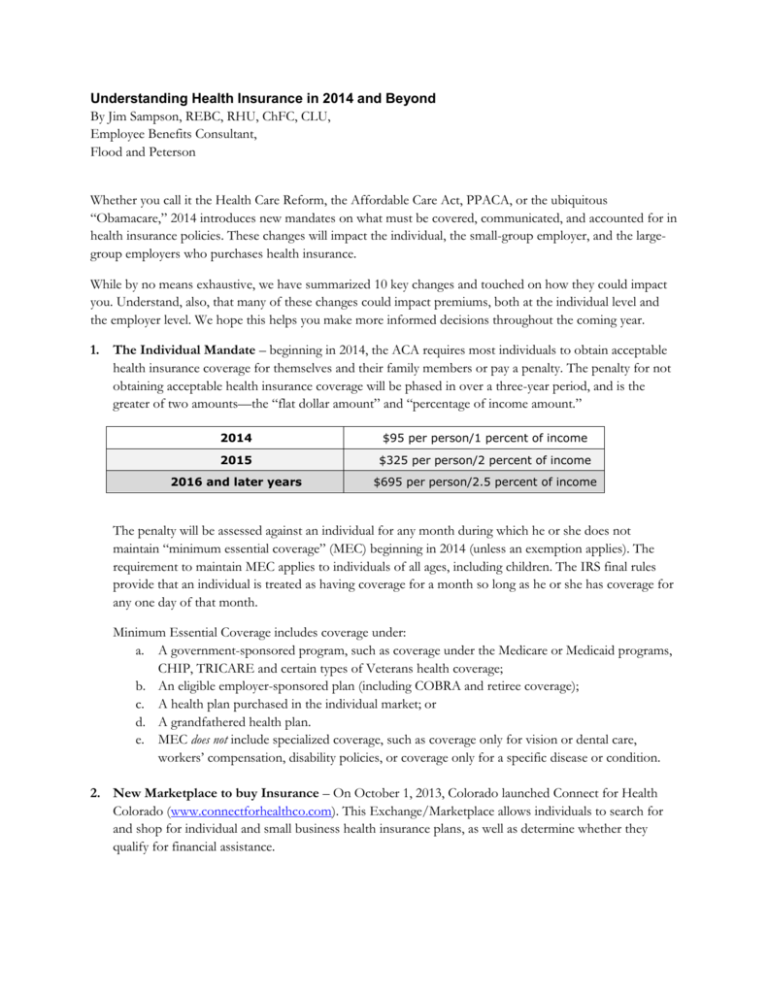
Understanding Health Insurance in 2014 and Beyond By Jim Sampson, REBC, RHU, ChFC, CLU, Employee Benefits Consultant, Flood and Peterson Whether you call it the Health Care Reform, the Affordable Care Act, PPACA, or the ubiquitous “Obamacare,” 2014 introduces new mandates on what must be covered, communicated, and accounted for in health insurance policies. These changes will impact the individual, the small-group employer, and the largegroup employers who purchases health insurance. While by no means exhaustive, we have summarized 10 key changes and touched on how they could impact you. Understand, also, that many of these changes could impact premiums, both at the individual level and the employer level. We hope this helps you make more informed decisions throughout the coming year. 1. The Individual Mandate – beginning in 2014, the ACA requires most individuals to obtain acceptable health insurance coverage for themselves and their family members or pay a penalty. The penalty for not obtaining acceptable health insurance coverage will be phased in over a three-year period, and is the greater of two amounts—the “flat dollar amount” and “percentage of income amount.” 2014 $95 per person/1 percent of income 2015 $325 per person/2 percent of income 2016 and later years $695 per person/2.5 percent of income The penalty will be assessed against an individual for any month during which he or she does not maintain “minimum essential coverage” (MEC) beginning in 2014 (unless an exemption applies). The requirement to maintain MEC applies to individuals of all ages, including children. The IRS final rules provide that an individual is treated as having coverage for a month so long as he or she has coverage for any one day of that month. Minimum Essential Coverage includes coverage under: a. A government-sponsored program, such as coverage under the Medicare or Medicaid programs, CHIP, TRICARE and certain types of Veterans health coverage; b. An eligible employer-sponsored plan (including COBRA and retiree coverage); c. A health plan purchased in the individual market; or d. A grandfathered health plan. e. MEC does not include specialized coverage, such as coverage only for vision or dental care, workers’ compensation, disability policies, or coverage only for a specific disease or condition. 2. New Marketplace to buy Insurance – On October 1, 2013, Colorado launched Connect for Health Colorado (www.connectforhealthco.com). This Exchange/Marketplace allows individuals to search for and shop for individual and small business health insurance plans, as well as determine whether they qualify for financial assistance. 3. Pre-existing Condition Exclusions - Effective for plan years beginning on or after Jan. 1, 2014, ACA prohibits health plans from imposing pre-existing condition exclusions (PCEs) on any enrollees. This change may encourage individuals to purchase their own policies after leaving a job, instead of enrolling in more costly COBRA insurance from the employer. 4. Limits on Cost-sharing - Effective for plan years beginning on or after Jan. 1, 2014, plans are subject to limits on cost-sharing or out-of-pocket costs. Out-of-pocket expenses may not $6,350 for self-only coverage and $12,700 for family coverage. This change has increased costs for many individual and group plans who previously passed on greater out of pocket costs. 5. Rating Methodology – Insurance companies will not rate insurance policies based on the member’s age, geographic location, family size, and tobacco status. A family’s premiums will now be the sum of each family member’s age-based rate. 6. Excessive Waiting Periods - Effective for plan years beginning on or after Jan. 1, 2014, a health plan may not impose a waiting period that exceeds 90 days. A waiting period is the period of time that must pass before coverage for an employee or dependent who is otherwise eligible to enroll in the plan becomes effective. 7. New Compliance Communications – A number of new notices must be given to employees at various times through the year. Be aware that as an employer, some of the notices you may have to provide include: a. Exchange Notices within 14 days of employee’s start date, b. Summary of Benefits and Coverage at initial and open enrollment, c. Statement of Grandfathered status if you still offer a plan that existed on March 23, 2010, and d. 60-Day Notice of Plan changes if significant changes are made outside of renewal. 8. New Fees built into premiums – In 2014 a number of new fees begin that will impact premiums. Those include: a. Research Fees - Health insurance issuers and self-funded group health plans must pay fees to finance comparative effectiveness research. For plan years ending on or after Oct. 1, 2013, and before Oct. 1, 2014, the fee is $2 multiplied by the average number of lives covered under the plan. b. Reinsurance Fees - Health insurance issuers and self-funded group health plans must pay fees to a transitional reinsurance program for the first three years of health insurance exchange operation (2014-2016). The fees will be used to help stabilize premiums for coverage in the individual market. For 2014, HHS has proposed a national contribution rate of $5.25 per month ($63 per year). For 2015, the annual contribution rate is proposed to be $44 per enrollee per year. c. Health Insurer Provider Fees - Beginning in 2014, the ACA imposes an annual, nondeductible fee on the health insurance sector, allocated across the industry according to market share. The aggregate annual fee for all covered entities is expected to be $8 billion for 2014, $11.3 billion for 2015 and 2016, $13.9 billion for 2017 and $14.3 billion for 2018. Insurance carriers will build this cost into their premiums. 9. Additional Medicare Tax - Effective Jan. 1, 2013, the Medicare Part A (hospital insurance) tax rate increases by 0.9 percent (from 1.45 percent to 2.35 percent) on wages over $200,000 for an individual taxpayers and $250,000 for married couples filing jointly. An employer must withhold the additional Medicare tax on wages or compensation it pays to an employee in excess of $200,000 in a calendar year. 10. Employer Penalties for Not offering Required Coverage (Large Employers only) - Employers with 50 or more employees (including full-time and full-time equivalent employees) that do not offer coverage to their full-time employees (and dependents) that is affordable and provides minimum value will be subject to penalties if any full-time employee receives a government subsidy for health coverage through an Exchange. This provision was delayed until 2015, but employers need to understand the mandate, examine how it might impact them, and begin to plan now. As you may suspect, the list could go on. However, these are top items that could impact your business or your family. For more help, feel free to contact Flood and Peterson. Founded in 1939, Flood and Peterson has become one of the most respected firms in the Rocky Mountain region and one of the nation’s largest independently owned agencies. With offices in Greeley, Fort Collins, and Denver, Colorado, we employ 118 dedicated, experienced professionals. Fifteen active partners lead our employee-owned company. Flood and Peterson advises clients in Commercial Insurance, Surety Bonds, Employee Benefits, 401K/Retirement Planning, and Personal Insurance.