respiratory membrane
advertisement
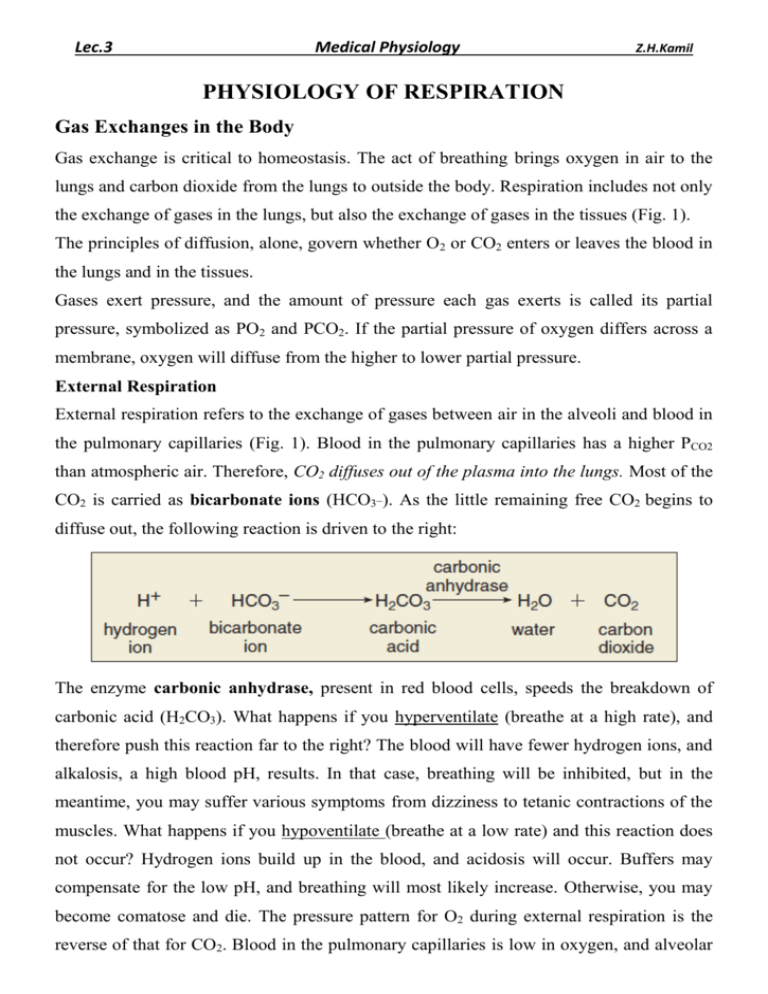
Lec.3 Medical Physiology Z.H.Kamil PHYSIOLOGY OF RESPIRATION Gas Exchanges in the Body Gas exchange is critical to homeostasis. The act of breathing brings oxygen in air to the lungs and carbon dioxide from the lungs to outside the body. Respiration includes not only the exchange of gases in the lungs, but also the exchange of gases in the tissues (Fig. 1). The principles of diffusion, alone, govern whether O2 or CO2 enters or leaves the blood in the lungs and in the tissues. Gases exert pressure, and the amount of pressure each gas exerts is called its partial pressure, symbolized as PO2 and PCO2. If the partial pressure of oxygen differs across a membrane, oxygen will diffuse from the higher to lower partial pressure. External Respiration External respiration refers to the exchange of gases between air in the alveoli and blood in the pulmonary capillaries (Fig. 1). Blood in the pulmonary capillaries has a higher PCO2 than atmospheric air. Therefore, CO2 diffuses out of the plasma into the lungs. Most of the CO2 is carried as bicarbonate ions (HCO3_). As the little remaining free CO2 begins to diffuse out, the following reaction is driven to the right: The enzyme carbonic anhydrase, present in red blood cells, speeds the breakdown of carbonic acid (H2CO3). What happens if you hyperventilate (breathe at a high rate), and therefore push this reaction far to the right? The blood will have fewer hydrogen ions, and alkalosis, a high blood pH, results. In that case, breathing will be inhibited, but in the meantime, you may suffer various symptoms from dizziness to tetanic contractions of the muscles. What happens if you hypoventilate (breathe at a low rate) and this reaction does not occur? Hydrogen ions build up in the blood, and acidosis will occur. Buffers may compensate for the low pH, and breathing will most likely increase. Otherwise, you may become comatose and die. The pressure pattern for O2 during external respiration is the reverse of that for CO2. Blood in the pulmonary capillaries is low in oxygen, and alveolar air contains a higher partial pressure of oxygen. Therefore, O2 diffuses into plasma and then into red blood cells in the lungs. Hemoglobin takes up this oxygen and becomes oxyhemoglobin (HbO2): Internal Respiration Internal respiration refers to the exchange of gases between the blood in systemic capillaries and the tissue fluid. In Figure 1, internal respiration is shown in the upper body and the lower body; however, the same events occur in both regions. Blood in the systemic capillaries is a bright red color because red blood cells contain oxyhemoglobin. Because the temperature in the tissues is higher and the pH is lower, oxyhemoglobin naturally gives up oxygen. After oxyhemoglobin gives up O2, it diffuses out of the blood into the tissues: Oxygen diffuses out of the blood into the tissues because the PO2 of tissue fluid is lower than that of blood. The lower PO2 is due to cells continuously using up oxygen in cellular respiration. Carbon dioxide diffuses into the blood from the tissues because the PCO2 of tissue fluid is higher than that of blood. Carbon dioxide, produced continuously by cells, collects in tissue fluid. After CO2 diffuses into the blood, it enters the red blood cells, where a small amount is taken up by hemoglobin, forming carbaminohemoglobin (HbCO2). Most of the CO2 combines with water, forming carbonic acid (H2CO3), which dissociates to hydrogen ions (H_) and bicarbonate ions (HCO3_). The increased concentration of CO2 in the blood drives the reaction to the right: The enzyme carbonic anhydrase, mentioned previously, speeds the reaction. Bicarbonate ions diffuse out of red blood cells and are carried in the plasma. The globin portion of hemoglobin combines with excess hydrogen ions produced by the overall reaction, and Hb becomes HHb, called reduced hemoglobin. In this way, the pH of blood remains fairly constant. Blood that leaves the systemic capillaries is a dark maroon color because red blood cells contain reduced hemoglobin. Hemoglobin activity is essential to the transport of gases, and therefore to external and internal respiration. External and internal respiration are the movement of gases between pulmonary capillaries and alveoli and between the systemic capillaries and body tissue fluid, respectively. Both processes depend on the process of diffusion. Figure 1: External and internal respiration. Oxygen Concentration and Partial Pressure in the Alveoli Oxygen is continually being absorbed from the alveoli into the blood of the lungs, and new oxygen is continually being breathed into the alveoli from the atmosphere. The more rapidly oxygen is absorbed, the lower its concentration in the alveoli becomes; conversely, the more rapidly new oxygen is breathed into the alveoli from the atmosphere, the higher its concentration becomes. Therefore, oxygen concentration in the alveoli, and its partial pressure as well, is controlled by: (1) the rate of absorption of oxygen into the blood. (2) the rate of entry of new oxygen into the lungs by the ventilatory process. Figure 2 shows the effect of both alveolar ventilation and rate of oxygen absorption into the blood on the alveolar partial pressure of oxygen (Po2). One curve represents oxygen absorption at a rate of 250 ml/min, and the other curve represents a rate of 1000 ml/min. At a normal ventilatory rate of 4.2 L/min and an oxygen consumption of 250 ml/min, the normal operating point in Figure 2 is point A. The figure also shows that when 1000 milliliters of oxygen is being absorbed each minute, as occurs during moderate exercise, the rate of alveolar ventilation must increase fourfold to maintain the alveolar Po2 at the normal value of 104 mm Hg. Another effect shown in Figure 2 is that an extremely marked increase in alveolar ventilation can never increase the alveolar Po2 above 149 mm Hg as long as the person is breathing normal atmospheric air at sea level pressure, because this is the maximum Po2 in humidified air at this pressure. If the person breathes gases that contain partial pressures of oxygen higher than 149 mm Hg, the alveolar Po2 can approach these higher pressures at high rates of ventilation. CO2 Concentration and Partial Pressure in the Alveoli Carbon dioxide is continually being formed in the body and then carried in the blood to the alveoli; it is continually being removed from the alveoli by ventilation. Figure 3 shows the effects on the alveolar partial pressure of carbon dioxide (Pco2) of both alveolar ventilation and two rates of carbon dioxide excretion, 200 and 800 ml/min. One curve represents a normal rate of carbon dioxide excretion of 200 ml/min. At the normal rate of alveolar ventilation of 4.2 L/min, the operating point for alveolar Pco2 is at point A in Figure 3—that is, 40 mm Hg. Two other facts are also evident from Figure 3: First, the alveolar PCO2 increases directly in proportion to the rate of carbon dioxide excretion, as represented by the fourfold elevation of the curve (when 800 milliliters of CO2 are excreted per minute). Second, the alveolar PCO2 decreases in inverse proportion to alveolar ventilation. Therefore, the concentrations and partial pressures of both oxygen and carbon dioxide in the alveoli are determined by the rates of absorption or excretion of the two gases and by the amount of alveolar ventilation. Figure 2: Effect of alveolar ventilation on the alveolar PO2 at two rates of oxygen absorption from the alveoli—250 ml/min and 1000 ml/min. Point A is the normal operating point. Figure 3: Effect of alveolar ventilation on the alveolar PCO2 at two rates of carbon dioxide excretion from the blood—800 ml/min and 200 ml/ min. Point A is the normal operating point. Diffusion of Gases Through the Respiratory Membrane Respiratory Unit. the respiratory unit (also called “respiratory lobule”), is composed of a respiratory bronchiole, alveolar ducts, atria, and alveoli. There are about 300 million alveoli in the two lungs, and each alveolus has an average diameter of about 0.2 millimeter. The alveolar walls are extremely thin, and between the alveoli is an almost solid network of interconnecting capillaries, because of the extensiveness of the capillary plexus. Thus, it is obvious that the alveolar gases are in very close proximity to the blood of the pulmonary capillaries. Further, gas exchange between the alveolar air and the pulmonary blood occurs through the membranes of all the terminal portions of the lungs, not merely in the alveoli themselves. All these membranes are collectively known as the respiratory membrane, also called the pulmonary membrane. Respiratory Membrane. The different layers of the respiratory membrane: 1. A layer of fluid lining the alveolus and containing surfactant that reduces the surface tension of the alveolar fluid 2. The alveolar epithelium composed of thin epithelial cells 3. An epithelial basement membrane 4. A thin interstitial space between the alveolar epithelium and the capillary membrane 5. A capillary basement membrane that in many places fuses with the alveolar epithelial basement membrane 6. The capillary endothelial membrane Despite the large number of layers, the overall thickness of the respiratory membrane in some areas is as little as 0.2 micrometer, and it averages about 0.6 micrometer, except where there are cell nuclei. The average diameter of the pulmonary capillaries is only about 5 micrometers, which means that red blood cells must squeeze through them. The red blood cell membrane usually touches the capillary wall, so that oxygen and carbon dioxide need not pass through significant amounts of plasma as they diffuse between the alveolus and the red cell. This, too, increases the rapidity of diffusion. Factors That Affect the Rate of Gas Diffusion Through the Respiratory Membrane the factors that determine how rapidly a gas will pass through the membrane are 1) the thickness of the membrane 2) the surface area of the membrane 3) the diffusion coefficient of the gas in the substance of the membrane, and 4) the partial pressure difference of the gas between the two sides of the membrane.