Gas Exchange and Pulmonary Circulation
advertisement
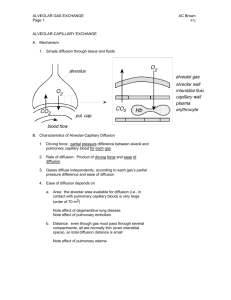
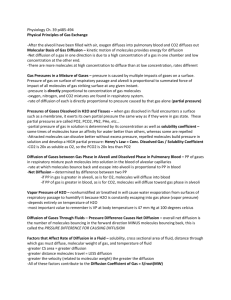
Gas Exchange and Pulmonary Circulation Learning Objectives • Understand diffusion and the rate of diffusion. • Understand gas pressure and partial pressure, and how these factors determine the net direction of diffusion. • Know the relevant partial pressures in atmospheric air, alveolar air and expired air and why they differ. • Know how the partial pressures of O2 and CO2 in alveolar air depend on the ventilation rate. • Know the basic anatomy of the respiratory membrane and what factors determine the rate of diffusion through this membrane. • Understand the diffusing capacity and the factors that increase it. Pulmonary Gas Exchange • This lecture will focus on the exchange of gases between the pulmonary blood and alveolar air, and the rate at which this occurs. • The gases exchange by diffusion: - O2 diffuses into the blood - CO2 diffuses out of the blood Diffusion Gases diffuse from an area of high concentration to an area of low concentration. It is based on the probability of freely moving molecules. Gas Pressure • Gas pressure is caused by the molecules colliding with the surface. • In the lungs, the gas molecules are colliding with the surfaces of the respiratory passages and alveoli. • Higher concentrations of gas will produce more collisions and cause a higher pressure. • This idea of pressure applies to gases whether in air or water. Partial Pressure • The total gas pressure is the pressure caused by all the gas molecules colliding with the surface. • The partial gas pressure is the pressure exerted by 1 gas species alone. Written as PO2 (partial pressure of O2), PCO2 (partial pressure of CO2). Atmospheric Air Partial Pressures Nitrogen 597 mm Hg 78.62 % Oxygen 159 mm Hg 20.84 % Carbon Dioxide 0.3 mm Hg 0.04 % Water 3.7 mm Hg 0.5 % Total 760 mm Hg 100 % • The rate of diffusion of a gas molecule is directly proportional to its partial pressure. Solubility Coefficient • The higher the solubility, the higher the solubility coefficient and the lower the partial pressure for a given concentration. Partial Pressure of Water • • • • Also called the vapor pressure. The PH2O of atmospheric air is 3.7 mm Hg. The PH2O at 37°C is 47 mm Hg. Thus, the air we breathe gets humidified during respiration. This occurs before the air gets to the alveoli. Direction of Diffusion • The net diffusion is determined by the difference between the partial pressures. • If the partial pressure of O2 is greater in the alveolar air than in the blood, the net diffusion of O2 will be into the blood. Comparing Atmospheric and Alveolar Air • In the alveoli: O2 is constantly being absorbed into the blood. CO2 is diffusing into the alveolar air. Air is humidified compared to atmospheric air. Rate of Alveolar Removal • The alveolar air is replaced slowly. During normal ventilation, ~1/2 of the gas is removed in 17 sec. • The slow replacement of alveolar air prevents sudden changes in [blood gas]. Partial Pressure of O2 in Alveoli • Alveolar PO2 depends on: - The rate of O2 absorption into the blood. - The rate of entry of new O2 during ventilation. Why does the alveolar partial pressure of O2 not increase above 150 mm Hg? Partial Pressure of CO2 in Alveoli • Alveolar PCO2 depends on: - The rate of CO2 excretion from the blood. - The rate of removal of CO2 during ventilation. Expired Air Anatomy Reminder for Respiratory Membrane Respiratory Membrane • Gas exchange between the alveolar air and pulmonary blood occurs through the membranes of the respiratory bronchioles, alveolar ducts and alveoli. • The respiratory membrane has a surface area of roughly 70 m2 or a 25 x 30-foot room. • The total quantity of blood in the pulmonary capillaries is 60-140 mL. • Spreading 60-140 mL over a 25 x 30-foot room allows for rapid respiratory exchange. Respiratory Membrane Factors Affecting Diffusion through the Respiratory Membrane • Thickness of the membrane. • Surface area of the membrane. • Diffusion coefficient. • Difference in partial pressure. Thickness and Surface Area of the Membrane • The thicker the membrane, the slower the rate of diffusion. E.g., edema in the interstitial space increases the distance gasses must diffuse. • If surface area decreases, the rate of diffusion will decrease. E.g., emphysema causes dissolution of alveolar walls. Diffusion Coefficient • The diffusion coefficient is proportional to the solubility/MW. • The greater the diffusion coefficient, the greater the rate of diffusion. • So, a small molecule that is highly soluble diffuses fast (e.g., CO2). CO2 diffuses ~ 20 x more rapidly than O2. Differences in Partial Pressure • As we have discussed, gases will diffuse from areas of high partial pressure to areas of lower partial pressure. Diffusing Capacity • Diffusing capacity is a measure of how well a gas diffuses across the respiratory membrane. • It is defined as the volume of a gas that will diffuse through the membrane each minute for a partial pressure difference of 1 mm Hg. Diffusing Capacity for O2 • Diffusing capacity for O2 is ~ 21 ml/min/mm Hg in the average young man. • Multiply this by the mean pressure difference (11 mm Hg) and one obtains the amount of O2 diffusing through the respiratory membrane each minute. In this example, 230 ml O2/min. Effect of Exercise on Diffusing Capacity • The diffusing capacity increases because of: - Dilating or opening dormant capillaries. - Improving the ventilation/perfusion ratio. Varying Degrees of Alveolar Ventilation and Capillary Blood Flow • Even normally, - Not all alveoli are equally ventilated. - Blood flow through the capillaries is not the same for all alveoli. VA will be used to define alveolar ventilation. Q will be used to define blood flow. The VA/Q is the ventilation/perfusion ratio. Zones of Pulmonary Blood Flow and VA/Q – Top of Lungs • Blood flow is low at the top of the lungs, compared to the bottom of the lungs. • Also, alveolar ventilation is low at the top of the lungs, compared to that at the bottom of the lungs, but blood flow is decreased more than ventilation. • The VA/Q at the top of the lungs is 2.5 x greater than ideal. Zones of Pulmonary Blood Flow and VA/Q – Bottom of Lungs • At the bottom of the lungs, there is too little ventilation relative to the blood flow. • The VA/Q at the bottom of the lungs is 0.6 x ideal. VA/Q During Exercise • During exercise, the blood flow to the upper part of the lung increases and the VA/Q reaches optimal values.