Slide (4) 1
This presentation will cover several areas starting theoretically and moving through to practical
application
Quick over view from the experts on pain
What It is /Pain pathways new advances in understanding /How does it present / why its
important to Rx appropriately
How does this effect pharmacology: The old & the new :
recognised drugs & ways of doing things
Recent innovations in pain management in response to new understandings of pain
pathways
The old drugs a new,
Research has provided evidence base for the use of old know drugs in new innovative
ways; we will briefly look at some of these concepts
We will look briefly at recent changes to clinical practice via modality of analgesic delivery
or different ways we utilize the drugs we have on hand
And finally
New ones Of course there are always New drugs
And whatever else happens to work it way into the presentation
Slide (4) 2 WHATS PAIN
Definition:Technically Pain is:
Always subjective
Learnt application of the word through (early) life experiences to perceived situation by the
individual
Unquestionably a sensation, in a part or parts of the body, but it is also always unpleasant and
therefore also an emotional experience for most. But may/may not have pathophysiological
cause! ………
It nevertheless elicits a pain response (International Association for the Study of Pain 1994)
However, many people may report pain in the absence of tissue damage or any likely
pathophysiological cause; usually this happens for psychological reasons.!
Subjectively: usually no way to distinguish individuals experience from that due to tissue
damage. Thus . If they regard their experience as pain & its reported in the same ways as
pain caused by tissue damage, it should be accepted as pain.
This definition avoids tying pain to stimulus. Activity induced in the nociceptor and the
nociceptive pathways by a noxious stimulus is NOT pain, which is always a psychological
state, even though we may well appreciate that pain most often has a proximate physical cause.
Futher:
Acute pain: ‘pain of recent onset & probable limited duration (90D), usually has identifiable
temporal & causal relationship to injury or disease’.
Chronic pain: ‘commonly persists beyond the time of healing of an injury & frequently there may
not be any clearly identifiable cause’ ((Ready & Edwards, 1992)ANZCA 2010).
A continuum is now recognized between acute & chronic pain rather than distinct entities.
Increased understanding of the mechanisms of acute pain has led to improvements in
clinical management & in the future it may be possible to more directly target the
pathophysiological processes associated with specific pain syndromes. ANZCA 2010
1
However in clinical practice pain is “whatever the experiencing person says it is, existing
whenever he says it does." (by Margo McCaffrey in 1968).
I propose that the future spoken of in 2010 is here today with the easy access to the Acute Pain
rd
Management: Scientific Evidence, 3 Ed 2010, Australian & New Zealand College of Anaesthetists
& Faculty of Pain Medicine, and an increased understanding of the pharmacokinetics of analgesic
drugs and there adjunctive’s
Slide 6) 3 Statement of Evidence for clinical practice (ANZCA 2010)
specific early analgesic interventions reduce the incidence of chronic (persistent) pain after
surgery. (level 11)
Persistent post surgical pain risk factors include: severity of pre & postoperative pain,
intraoperative nerve injury & psychological vulnerability. (level 1V)
Pre-emptive vs preventive analgesia:i.e. Epidural, Ketamine, Gadapentin, Clonidine
ANZCA recommendations provide us a guide to effective management of pain.
1. Epidural prior to thorocotomy & continued post op. Thorocotomy incidence of chronic pain
greatly reduced with 10% pt rating pain > 5/10 p10
2. Peri operative Gabapentin to pt having mastectomy Gabapentin pre mastectomy-neuropathic
pain at 6 mths : placebo group 25% / treated group 5%.
Pre-emptive - Where a preoperative treatment is more effective than the identical treatment
administered after incision or surgery.:
Epidural.
Wound infiltration with LA prior to incision
Patient Education to reduce anxiety
Pre-emptive vs preventive analgesia
The timing of a single analgesic intervention (pre incision vs post incision), defined as pre-emptive
analgesia, has a significant effect on postoperative pain relief with epidural analgesia. (level
1)There is evidence that some analgesic interventions have an effect on post operative pain and
/or analgesic consumption that exceeds the expected duration of action of the drug defined as
preventive analgesia. Eg Ketamine. (level 1) ANZCA 2010
So the evidence supports that pharmacology works and works well, so what are some of
the wholes in the system
1 Lack of accurate preoperative work up,where appropriate pre emptive analgesia is known to be
of benefit: i.e.
Epidural for amputations,
pregabalin for anticipated or know neuropathic pain,
conversion to methodone from Norspan 7/7 pre op,
appropriate education & assessment of patient to ascertain existing potential tolerance/ or
sensitivty levels; expected or perceived pain levels currently experienced or expected
2. Inability to target specific types of pain appropriately (lack of adequate pain type assessment) &
/or knowledge of targeted pharmacology (narcotic & adjunctive)
3. Time constraints, pre operatively, intra operatively and post operatively
Slide (7) 4
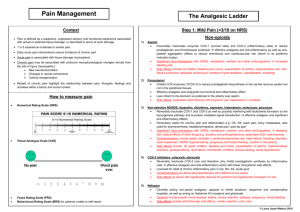
The WHO ladder illustrates the basic world standards for pain management. However it looks
primarily at one the 4 element of the pain processing: Perception & thus in light of recent R&D is
incomplete
2
Slide (8) 5 “You must unlearn what you have learned”
There are many things we must unlearn from old ways of using medications, expected delivery
methods, expected hospitalisation times i.e. joint replacements . The list goes on
Personal Bias’s: Our individual conditioned response to a patient in pain – working out of our
perception not theirs. Particularly with acute on chronic patients or those who use illicit
substances as well. Judge not least you be judged” Patient respect to quality care mandated that
we do not judge.
Slide (9) 6 Acute pain exacerbations may result in neural sensitization &
release of mediators both peripherally & centrally
Recent advances in postoperative pain management aims to limit this process & are
loosely grouped in the following areas:
Molecular Mechanisms: Extremely complex evolving concepts: a increased
variety of receptors; neurotransmitters (inhibitory/excitatory) ; at an increased
number of levels from the site of injury (or not) – through to intricate parts of the
brain. Impulse's going up the ascending pathway through the dorsal horn/spinal
cord to the relevant areas in the brain where a variety of registrations occur & then
send stimulus signals down the descending pathway to the site of perceived
stimulus. Exacerbations of acute; acute on chronic or chronic pain can lead to
neural sensitization & release of mediators both peripherally & centrally. N-Methyl DAspartate (NMDA) activation results in ‘clinical wind up: central sensitization (wind
up), long-term potentiation of pain (LTP), & transcription-dependent sensitization.
Pharmaceutical products Advances in molecular mechanisms knowledge have
led to the development of multimodal analgesia & new pharmaceutical products to
treat postoperative pain.
Routes and modes of delivery: R&D to develop longer lasting drugs, those with
different property combinations, or differing routes of administration
Other modes of analgesia, (adjunctives): New types, use of established drugs in
new ways LA, gabapentin etc
Organizational and procedural aspects: New ways of stream lining procedures,
new education programs to psychologically modulate patient perceptions
Molecular Mechanisms (extremely complex, for me @ least )
1.Molecular Mechanisms: peripheral sensitization - primary mediators –secondary mediators
N-Methyl D-Aspartate (NMDA) receptor & central sensitization (CS): Clinical wind up occurs from the processes of
(NMDA) activation,
wind up CS,
2.Long-term potentiation of pain (LTP), early LTP (reversible ) unrelieved will progress to late irreversible memory
pathway's in the brain in response to perceived pain registration regardless of presence of pain stimulus
3. Transcription-dependent sensitization(TDS) activation of NMDA wind up and early LTP of pain are
transcription-independent processes. TDS is mediated by inflammation & related alterations in the dorsal root
ganglion, the dorsal horn, & irreversible structural modifications in the central nervous system. TDS : 2 forms:
1. activity independent localized - includes the late phase of LTP, & 2 activity independent widespread - Late phase
LTP seen mainly in the hippocampus and other cortical areas.
3
4. Common mechanisms of pain and memory: neurokinin (NK1);COX-2 & NMDA receptor are involved in CS,
but not involved in hippocampal LTP memory The common mechanisms in hippocampal early phase LTP & CS
are phosphorylation of synaptic receptors and the insertion of AMPA receptors into the post-synaptic membrane.
There is only synaptic strengthening in hippocampal LTP, while CS also can cause neuronal network changes &
other cellular mechanisms. Necessary then to avoid the interruption of memory formation & cortical function
while treating CS since the process of LTP is present in CS as well as in memory mechanisms in the cortex .
Slide (10) 7 Pain Processing Element
•
•
•
•
•
Transduction
– Noxious mechanical, chemical and thermal stimuli are converted to action
potential
Transmission
– AP conducted through nervous system
Modulation
– Alteration of neural transmission along the pain pathway, principally at dorsal
horn
Perception
– Final common pathway. Integration of painful input into somatosensory and
limbic cortex.
Traditional analgesic approaches may target only perception
Slide (11) 8 This diagram details the Pain Processing Element highlights the
wide range of possible site for adjunctive therapies pharmacology activity
Slide (12) 9 Diagram of pain pathways
Rational: Pain management pharmacology i.e. targeting ‘pain processing’
mechanism with specifically targeted drugs allows accumulative synergistic effect
of pharmacology. ‘a little bit of a lot lessens the load’ . This reduce the risk of both
ongoing pain sensation with it physiological & psychological effects. But
potentially more importantly the risk of ‘wind up’ formulation & minimize adverse
effects in critical structure including but not restricted to: NMDA; receptors, PAG &
RVM centres in the Brain.
NMDA = N-methyl-d-aspartate; PAG = periaqueductal gray; RVM = rostral
ventromedial medulla (brain stem)
Pain Pathway understanding, although the "gate control" theory of pain basic
idea still has merrit: incoming pain stimuli can be "gated" (shut off) by other stimuli,
because many nerve cells talk to one another in the dorsal horn of the spinal
cannel as important fibers coming from the periphery into the dorsal horn send
impulses brain ward that are then interrupted and relayed back to source (overs
implication) recent R&D has details are far more intricate detailed process which
continues to evolve as neuroscience understanding advances
Tiny unmyelinated 'C' fibres: important carriers of the long-lasting burning pain that makes a surgical wound (for
example) such an unpleasant experience. There is controversy about where these fibres terminate - in primates
4
many terminate in the deep dorsal horn and even the ventral horn, although conventionally lamina II has been said
to be their destination (Willis and Westlund).
Thin myelinated 'A delta' fibres, concerned with more accurate localisation of pain, and terminating mostly
laterally in laminae I and V.
Rather chunky 'A beta' fibres that carry information about vibration and position sense from the periphery to the
cord.
Unpleasant stimuli entering via the C fibres can be suppressed by concurrent stimulation of A delta fibres (high
amplitude low frequency stimulation, for example by acupuncture) or by impulses passing through A beta fibres.
Examples of the latter include TENS (transcutaneous electrical nerve stimulation) and the simple expedient of
rubbing the skin, which is well known by mothers to decrease perception of pain!
Pain pathways components :st
nd
A)Peripheral receptors; 2 distinct types responses to a painful stimulus 1 /2 . 1st pain is well-localised to part
of body surface & brief, described as sharp, and "pricking“ .The receptors are high threshold mechanoreceptors .
There appear to be specific "nociceptors" which mediate pain, and ONLY pain
nd
The 2 is more diffuse & protracted & due to stimulation of receptors that exist in many tissues (but not in,
paradoxically, the brain). Described often as dull (i.e. not sharp) and aching - being poorly localised. Receptors are
termed polymodal nociceptors. Pain tends to last beyond the termination of an acute painful stimulus. Sources,
nd
pathways, perception of & Rx is very different. Visceral pain is predominantly of the “2 pain" type. Although
Visceral pain can however sometimes be referred to a region of the body surface (for example, shoulder tip pain with
sub-diaphragmatic irritation). See [Cervero, F. Physiological Rev 1994(74.1) 95-129pp] for a review of the sensory
innervation of the viscera.
Evidence that neurotransmitters such as substance P (=sP), vasoactive intestinal polypeptide (VIP) and
calcitonin gene-related peptide are important mediators, either as neurotransmitters, or sensitisers of
visceral pain receptors. Prostaglandins, histamine, serotonin, bradykinin, ATP, potassium, and H+ ions also
appear important in this regard, especially serotonin, which appears to act mainly on 5HT3 receptors.
Pain perception, thresholds for feeling pain are remarkably constant from individual to individual. i.e. Peripheral
receptor stimulation of sufficient intensity will reproducibly cause pain at the same level in most people. The
response of the individual, & his tolerance of the pain, will however differ markedly between individuals.
Of great interest is "Neurogenic Inflammation". Here, stimulation of C fibres causes a local reaction:
vasodilatation & increased capillary permeability; due to retrograde transport & local release of sP and
calcitonin gene-related peptide. Resulting in potential release:, K+, H+, acetylcholine, histamine and
bradykinin & these cause prostaglandin & leukotriene production (which may end up sensitizing highthreshold mechanoreceptors)! Neurogenic inflammation may spread to surrounding tissues antidromically!!
Peripherally acting analgesia include: NSAID, corticosteroids, LA (which may theoretically inhibit neurogenic
inflammation if given early enough, an area of great controversy), & even novel drugs such as substance P
antagonists (One such antagonist that does NOT appear to work very well is capsaicin, but opioids, serotonin
antagonists, baclofen & clonidine may also inhibit sP release).
Of note is the recent identification of two different types of cyclo-oxygenase, with the potential for developing more
specific NSAID’s, with (perhaps) fewer side-effects.
st
B. Neural pathways. 1 pain: responses are conveyed from the periphery to the dorsal horn of the spinal cord in
small myelinated fibres (A delta) while 2nd pain is conveyed in non-myelinated C fibres. Important, especially
when considering the "gate control theory" detailed below. Also of importance to this theory are afferent stimuli
coming in large myelinated fibres (A beta fibres), from peripheral vibration / pressure / touch receptors.
Neurogenic pain, originating in damaged or abnormal C fibers, thus may respond to membrane- stabilizing drugs
such as anticonvulsants (e.g. carbamazepine).
C. Spinal cord pathways.
Complex. We will consider: initial connections : laminae in the spinal grey matter close to where the fibres enter the
spinal cord.
Local interconnections.
Ascending pathways and descending (control) pathways are considered much later.
Neural pathways;
Spinal Cord mechanisms & long tracts;
Brainstem, thalamus, cortex & other areas.
Descending pathways. Ascending Pain Connections
We now have sufficient resources to examine the various ascending pain pathways. First, the primitive spino-reticulodiencephalic connections Next, we examine the phylogenetically more modern pathways from cord to lateral
thalamus and thence to the S I cortex. These pathways are discriminative pain pathways, and have little to do with
perception of pain as a 'sore' stimulus! These pathways have few or no opioid receptors - morphine (for example)
will have no effect on such pathways
Descending Pain Connections
As important as the ascending pathways are fibres that descend from brainstem to spinal cord to modulate the
incoming signals. Notable neurotransmitters mediating this anti-nociceptive effect include noradrenaline
(norepinephrine), especially in the locus coeruleus, and serotonin in the raphe nuclei. Opioid receptors are
prevalent here. Some descending connections are: Descending connections that modulate incoming pain
impulses.
Incoming painful stimuli are transmitted (A) to the dorsal horn, and from there (B) to the periaqueductal grey (PAG).
Descending impulses pass (C) to the raphe nuclei, especially the nucleus raphe magnus, in the upper medulla, and
thence back to the dorsal horn via reticulospinal fibres (D).
The above shows only the serotonergic descending fibres. Other pain-suppressing impulses pass from the PAG to the
locus coeruleus, and from there to the dorsal horn.
Pain in the periphery - the nociceptor
5
The above connections are awfully complex. One might think that once we moved out to the periphery, things might
become more simple. Not so! Most tissues are well provided with specific pain receptors called nociceptors.
Formerly it was thought that painful stimuli were detected through 'overstimulation' of receptors for other modalities.
This is incorrect. The quality of the pain perceived on stimulation of nociceptors seems to depend on the site of
stimulation, and the nature of the fibres transmitting the sensation. Even in the periphery, there is a distinction
between the sharp immediate pain ("first pain") transmitted by A delta fibres, and the prolonged unpleasant burning
pain mediated through the smaller unmyelinated C fibres.
Nociceptors have numerous different receptors on their surfaces that modulate their sensitivity to stimulation. These
include GABA, opiate, bradykinin, histamine, serotonin and capsaicin receptors, but the various roles of these
receptors are poorly characterised.
The most fascinating aspect of pain perception in the periphery is that normally most nociceptors lie dormant.
Inflammation sensitizes this vast population of nociceptors, making them far more sensitive to stimulation
(hyperalgesia). Hyperalgesia may be primary (felt at the site of stimulation, related to sensitization of the neurones
innervating that area) or secondary (felt at a site remote from the original injury, and probably related to NMDAmediated "wind-up").
& Neurotransmitters
A plethora of neurotransmitters mediates transmission of the sensations of pain in both brain and spinal cord. The list
is intimidating, and grows daily. We can try and 'lump' these neurotransmitters into various groups:
Excitatory neurotransmitters:
Important are glutamate and the tachykinins, agents that act at the various neurokinin receptors including as
substance P ('P is for pain'), neurokinin A and neurokinin B. Other substances that transmit pain impulses from
incoming nerves in the dorsal horn including calcitonin gene-related peptide, vasoactive intestinal polypeptide,
somatostatin and bombesin.
Inhibitory neurotransmitters:
There are several inhibitory neurotransmitters, but in the central nervous system, gamma amino butyric acid
(GABA) appears to reign supreme. Over forty percent of inhibition in the mammalian central nervous system is
GABAergic.
Neurotransmitters involved in Descending Pain Regulation:
Here, the alpha-2 stimulatory effects of noradrenaline (norepinephrine) and the effects of serotonin are
prominent. Opiates relieve pain by stimulating mu and delta receptors at a host of sites.
Specific neurotransmitters
Glutamate
A brief Medline search for articles using the abbreviation "NMDA" in the past ten years will garner about twelve
thousand references. This attests the fanatical interest researchers have in this, the hottest of the glutamate
receptors, but one mustn't forget that there are at least two others, the "AMPA" receptor and the obscure and
devious metabotropic receptor. The NMDA receptor mediates a host of spinal responses to severe painful
stimulation, but there are several catches to understanding how it works. Normally, the receptor is inactive as it is
physiologically choked by a magnesium ion sitting in its ion channel. In order for this ion to be removed, adjacent
peptide receptors have to be stimulated - the Mg++ then pops off, and an emphatic painful response occurs.
Neurophysiologists have known about this phenomenon for ages, gracing it with the label "wind-up" - as the
frequency of C-fibre stimulation increases there is a dramatic and long-lasting central response, with some
populations of spinal neurones becoming more and more sensitive to stimulation.
Consequences of glutamate receptor activation include production of c-fos (discussed below) and spinal production of
prostanoids and the ubiquitous Dr NO, nitric oxide. Unfortunately all this knowledge benefits clinicians surprisingly
little, as drugs that antagonise the effect of glutamate at the NMDA receptor tend to induce psychosis in humans,
but the combination of low dose NMDA antagonists with opioids may be supra-additive with fewer side effects.
GABA
GABA is widespread in the brain and spinal cord. Together with its partner glycine, it has major inhibitory effects,
dramatically evident in poisoning with strychnine, which antagonises glycine. Interneurones in laminae I, II and III
are GABA-rich, and mediate gate control in the dorsal horn by synapsing on neurones that contain substance P.
There are several distinct GABA receptors that work quite differently - the GABAA receptor is a "ligand-gated ion
channel" that allows chloride ions to leak into the cell, while the GABAB receptor is a "seven-spanning"
transmembrane structure that activates G proteins.
Again, the clinical utility of this knowledge is small, as GABAB receptor agonists such as baclofen, which are
analgesic at the spinal level in rats, have little effect in man, although they may potentiate the analgesia of
morphine. Benzodiazepines modulate the GABAA receptor allosterically - but GABAA seems more important at
supraspinal than spinal sites.
Tachykinins
It will probably be several years before newer agents such as neurokinin antagonists have been tested sufficiently
for widespread clinical use, although (for example) NK-1 antagonists such as CP-96 345 have been shown to
moderately decrease isoflurane MAC in tail-clamped rats (shudder!) when given intrathecally. Neurokinin receptors
probably do mediate pain in the spinal cord - substance P binds to the NK-1 receptor while neurokinins A and B
bind respectively to the NK-2 and NK-3 receptors. Collectively these substances are known as 'tachykinins'. The
tachykinin receptors are G-protein coupled, and increase intracellular calcium levels, triggering gene transcription.
E. Descending pathways.
Descending modulation of pain sensation originates from three main areas: Brainstem, where the Periaqueductal grey
matter (PAG) is particularly important.
Fibres pass from PAG to the reticular formation of the medulla (the nucleus raphe magnus or "NRM", and the closely
associated nucleus reticularis gigantocellularis pars alpha, and nucleus reticularis paragigantocellularis, all together
called the ventromedian medulla or "VMM") where connections are serotoninergic, and from there axons descend
in the "dorsolateral funiculus" of the spinal cord, to end up (surprise, surprise) on interneurones right next to the
substantia gelatinosa (lamina II) in the cord. The synapses here are enkephalinergic. Stimulation of this system
causes inhibition of incoming pain impulses. Thus, although serotonin applied peripherally augments pain, its action
centrally is important in descending inhibition of incoming painful impulses! New evidence suggests that GABA is
also important in inhibition of pain pathways by the VMM [Neuroscience Jul 1996 73(2) 509-18pp].
6
Slide (13) 10 Diagram at the neural level
Busy diagram but just know that there is lots of neurotransmitters & receptors that makes the
process of effective targeted pain management complicated but also gives lots of options for
onging pain management
Molecular Mechanisms: peripheral sensitization - primary mediators –secondary mediators
NMDA receptor and central sensitization (CS): Clinical wind up occurs from the processes of N-Methyl D-Aspartate
(NMDA) activation,
wind up CS,
Long-term potentiation of pain (LTP), early LTP (reversible ) unrelieved will progress to late irreversible memory
pathway's in the brain in response to perceived pain registration regardless of presence of pain stimulus
Transcription-dependent sensitization(TDS) activation of NMDA wind up and early LTP of pain are transcriptionindependent processes. TDS is mediated by inflammation & related alterations in the dorsal root ganglion, the
dorsal horn, & irreversible structural modifications in the central nervous system. TDS : 2 forms: 1. activity
independent localized - includes the late phase of LTP, & 2 activity independent widespread - Late phase LTP seen mainly
in the hippocampus and other cortical areas.
Common mechanisms of pain and memory: neurokinin (NK1);COX-2 & NMDA receptor are involved in CS, but not
involved in hippocampal LTP memory The common mechanisms in hippocampal early phase LTP & CS are
phosphorylation of synaptic receptors and the insertion of AMPA receptors into the post-synaptic membrane. There
is only synaptic strengthening in hippocampal LTP, while CS also can cause neuronal network changes & other cellular
mechanisms. Necessary then to avoid the interruption of memory formation & cortical function while treating CS
since the process of LTP is present in CS as well as in memory mechanisms in the cortex .
Slide (14) 10 Practical concepts in pain: Not controlling post operative pain has negative
effcts benefits;
Not controlling post operative pain has negative benefits;
Physiologically and psychological aspects of patient experience of pain are considered together
left as to right hands. Then next slide provides a summary of these effects
Exacerbations of acute A on C, or Chronic pain can lead to neural sensitization & release of
mediators both peripherally & centrally. N-Methyl D-Aspartate (NMDA) activation results in ‘clinical
wind up: central sensitization (wind up), long-term potentiation of pain (LTP), & transcriptiondependent sensitization
Advances in molecular mechanisms knowledge have led to the development of multimodal
analgesia & new pharmaceutical products to treat postoperative pain.
R&D New pharmacological products to treat postoperative pain include extended-release epidural
morphine & analgesic adjuvants such as capsaicin, ketamine, gabapentin, pregabalin
dexmetomidine, and tapentadol. Newer postoperative patient-controlled analgesia (PCA) in modes
such as intranasal (ie fentanyl), regional, transdermal, and pulmonary (USA) presents another
c
interesting avenue of development .( N. Vadivelu, S. Mitra, & D. Narayan, (2010) Recent
Advances in Postoperative Pain Management ,Yale J Biol Med. Mar 2010; 83(1): 11–25.
Published online Mar 2010)
Molecular Mechanisms: peripheral sensitization - primary mediators –secondary mediators
NMDA receptor and central sensitization (CS): Clinical wind up occurs from the processes of N-Methyl D-Aspartate
(NMDA) activation,
wind up CS,
Long-term potentiation of pain (LTP), early LTP (reversible ) unrelieved will progress to late irreversible memory
pathway's in the brain in response to perceived pain registration regardless of presence of pain stimulus
Transcription-dependent sensitization(TDS) activation of NMDA wind up and early LTP of pain are transcriptionindependent processes. TDS is mediated by inflammation & related alterations in the dorsal root ganglion, the
dorsal horn, & irreversible structural modifications in the central nervous system. TDS : 2 forms: 1. activity
7
independent localized - includes the late phase of LTP, & 2 activity independent widespread - Late phase LTP seen mainly
in the hippocampus and other cortical areas.
Common mechanisms of pain and memory: neurokinin (NK1);COX-2 & NMDA receptor are involved in CS, but not
involved in hippocampal LTP memory The common mechanisms in hippocampal early phase LTP & CS are
phosphorylation of synaptic receptors and the insertion of AMPA receptors into the post-synaptic membrane. There
is only synaptic strengthening in hippocampal LTP, while CS also can cause neuronal network changes & other cellular
mechanisms. Necessary then to avoid the interruption of memory formation & cortical function while treating CS
since the process of LTP is present in CS as well as in memory mechanisms in the cortex .
Slide (15) 11 Controlling post operative pain has negative effects: Physiologically &
Psychological effects Diaragm
Slide (16) 12 Practical concepts in Pain: cont’d
Practical concepts in Pain: So what do we actually see and what seems to work
1.Patient comfort/Functional ability/activity =
Patient expectations: Fact or Fiction +
+2 Basic Pain Assessment (thorough
+ 3 Present / Past History)
+ 4 Positioning
+ 5 Pharmacology
We will look at each of these in turn
The purpose of pain management is to allow the patient to be comfortable at rest & to a greater
degree whilst activity also. After all no one has time to lie around in our modern busy hospitals!
Slide (17) 13 Patient comfort
What is patient comfort? As with the subjective nature of pain perception, patient comfort level is
also a subjective assessment being a balance between pain registration (their score & FAS);what’s
perceptually emotionally, physiologically & pharmacologically achievable in a given situation for
the individual.
I often call these situations patchwork quilts or coats of analgesia that adequately covers the
painful stimulus allowing patients to attend activities of daily living comfortably.
It is a process that is expected to improve over time as healing continues the need for analgesia
reduces but at all time a patient ideally can preform their activity of daily living, initially with
assistance possibly but ultimately unadded as far as practicable
Thus, the more complex the situation the more effective pre operative education and pain
management will enhance post operative outcomes
Effective pre operative education which may include training in relaxation & breathing
techniques in combination with realistic evidence based patient targeted ouitcomes education can
be very beneficial in the postoperative recovery phases. This may mitigate pain registration &
adverse outcome, thus enhance recovery time.
Hip surgery expectation up same day dressed in street clothes home day 1 that what’s educated
and that what patient expect and in the main that’s what happens
8
Slide (18) 14 1. Comprehensive assessment of pain. 2. Past history / present
comorbitities& projected outcomes are considered together as they are always
interconnected & individualised to the patient & particular situation at hand.
Standardised Scoring system: i.e. numerical; visual analogue scale; Wong baker; Behavioural
rating scale + Functional Activity Score (FAS), BHS has a standard assessment & measurement
th
of acute pain chart at each patient bed., pain is considered the 5 basic observation & as such is
recorded on RORC, & all other ORC type charts.& there a few of them!
Direct Pain type Rx: Recognition of the 8 pain types (BHS we use a table of the 8 pain types
with descriptor information & suggested pharmacological treatments available; & we also refer to
ANZCA 2012 for specific condition treatment regimes if patients are unable to give accurate pain
type descriptions.
Note chronic pain patients & possibly those with cognitive impairment may have difficulty
localizing to pain; actual pain descriptors as part of their coping mechanism - psychological
aversion to the pain stimulus – they just don’t want to look at or concentrate on the pain
experienced when its intense.. They may be more able to describe when some level of control
achieved.
Thus as a nurse it is important to be vigilant to the nonverbal cues, frequency, intensity & or
alteration to pain experienced, patient spontaneous descriptors & any alteration in non verbal pain
stimulus registration post Rx’s. In addition, having a grasp of the onset /peak action times of drugs
given (route specific) will allow more accurate assessment and negate ‘wind up tiggers’.(asking if
improved when inadequate time elapsed for response registration. i.e bolusing APP /epidural)
Slide (19) 15 Comprehensive assessment of pain BHS tool
Slide (20) 16 1. Comprehensive assessment of pain 2) Past history / comorbitities cont’d
What are the elements of a comprehensive pain assessment these can also be stated as:
Patient individual interpretation of their 3 P’s Present, Past and projected situation, will colour their
end interpretation of a pain response & subsequent response to management,
Thus, it is important to individualise the experience & normalise to expected outcomes (this may
be the general population or in complex case specific to the individual)
Anatomically: loss of perceived vital organ/ or actual loss of vital organ; amputations pt
happy for same (glass half full) – unhappy about same – (half empty), back surgery working
/retired etc
Physiologically: individuals ability to tolerate/metabolise medications will effect what’s
used; ability to effectively heal or rehabilitate will effect expected & actual pain management
plans & outcomes
Psychologically: in combination with the above & taking into consideration the patients
congnitive resilence & or capacity to understand the surgical process & outcomes
The American Academy of Pain Medicine (AAPM), American Pain Society (APS), American
Society of Addiction Medicine (ASAM), & NAABT recognizes these definitions below as the
current accepted definitions.
I. Addiction:
Addiction is a primary, chronic, neurobiologic disease, with genetic, psychosocial, & environmental
factors influencing its development & manifestations.
It is characterized by behaviors that include one or more of the following: impaired control over
drug use, compulsive use, continued use despite harm, and craving.
9
II. Physical Dependence:
Physical dependence is a state of adaptation that is manifested by a drug class specific withdrawal
syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level
of the drug, &/or administration of an antagonist.
III. Tolerance:
Tolerance is a state of adaptation in which exposure to a drug induces changes that result in a
diminution of one or more of the drug’s effects over time.
Physical dependence & tolerance are normal physiology. Addiction is a disorder that is damaging
& requires treatment
Present / Past History (previous pharmocology exposure (always be mindful of self medicating
with drugs Script/elicit/alcohol all will effect “tolerance” /treatment options, conversely analgesic
naive patient may have little requirement (codeine % Caucasian population don’t possess enzyme
required to convert codeine to morphine so passes through system with no effect; past pain levels
+ Positioning
+ Pharmacology
= Patient comfort/Functional ability
Analgesia is titrated to patient’s report of pain and functional ability.
.
Slide (21) 17
How does the patient describe the pain chart?
Slide (22) 18 3 .Patient expectation: Fact or fiction
Patient expectations: No doubt that appropriate pre operative education (ideally pre anaesthetic
clinic staff with specialised staff) is of great benefit to patients understanding of what’s a
reasonable expectation:
1 Thoughts : Understanding the Pt knowledge/ expectation from past experience/exposure
or others feedback, that may or will impact of current presentation allows for effective remodeling
(education on new ways of doing things) so that patient’s knowledge and thus expected outcomes
hence are in keeping with current practice.
- i.e (recent in particular Ortho: THR educ), debunk misconcept’s of patient being ill needing
to lie in bed, or the magnitude of the surgical assault/ thus expected outcome i.e. lap choly/ open
choly expected pain differences; adbo surgery: spinal /general anaesthesia or open / laparoscopic
procedures
2. Actions : clear expectations of what physical activity &/ or how quickly there is
expected to be a return to ADL’s discussed pre operatively and reinforces post operatively,
this includes length of hospital stay
3. Reality: glass half full not half empty, encouragement that is empathetic and
sincere ensuring that all adjunctive therapies and supports are instigated in a timely
manner.
True these patient are in their initial post operative stage one would hope that much
of this has already been attended too, but if not there may be a need for
organizational change
Comprehensive Pain Assessment: This requires a detailed actual assessment of the descriptive
type, location, intensity, duration, new or old & importantly any known relieving strategies by the
patient or staff.
10
In combination with relevant past history. Understanding a patient history of the pain experience
and what previous medications strategies or other relieving techniques may be beneficial.
Likewise Acute on Chronic pain operative site may be insignificant to pre operative complaint or
post operative pain insignificant to preoperative despite operative procedure (arthritic pains
Co Morbidities liver/ kidney (metabolism), diabetes,(neuropathies) paraplegias past injury relevant
and/ or contributory pain tolerance issues, Importance of support: Both Physical and Psychological
will help shape a patients perception of the pain experience
Positioning/Reassurance: One of the simplest and most effective things – ensure good body
alignment and reduced tension of the operative site – if appropriate provide counter tension (towel
over abdomen – and be able to explain its benefits to the patient – increase likelihood of patients
using techniques.
Pharmacology choice appropriate to pain type (8). Not all responsive to narcotic some responsive
to adjunctive type pharmacology ie neuropathic pain Acute Pain Management ANZCA,
The importance of adjunctive therapy: allow for a broader coverage of pain receptor sites and thus
greater opportunity to minimise the pain signal registration for the individual in response to smaller
dosing of any one particular drug . Has the side benefit of reduce side effects and tolerance
response in .
Other aspects: Supportive therapies, counselling
Slide (23) 19 3.Patient expectation: Fact or fiction cont’d
Past injury/scaring or chronic pain, Rx for same (tolerance)
Elicit drug / Alcohol use (tolerance)
Renal/Liver impairment effects pharmacology metabolism & excretion
(consideration particularly in the
elderly)
pt age/metabolic capacity. As a rule of thumb in the young and the elderly it ideal to use drugs with
less active metabolites therefore less risk of accumulative effect or side effects. In addition the
dosing requirements is usually less than for adult patients, although children dosing is usually up
to age 8-10years onset of elderly dosing is dependent on co morbidity states but generally
considered around age 70
Slide (24) 20 4. Positioning
Positioning: importance of support & reassurance this allows patient to have some control
over their body even if only perceived ie towel to counterbrace abdomen when coughing (helpful to
explain mechanism - increases compliance if patients understand why)
Optimized supportive patient position will greatly assist pain management, it’s simple and
often overlooked.
Abdominal surgery knee’s up takes tension of the abdominal muscles.
Elevation of limbs reduces swelling
Sitting as upright as possible takes weight off the diagram.
Limbs supported in position of comfort
Other supportive devices
Occasional with effective communication of expected outcomes considerate of patient pre
condition and utilizing optimized positioning is significant enough to control pain
Slide (25) 21
Slide (26) 22 5.Targeted Pharmacology
11
Targeted Pharmacology
1. ANZCA: Appropriate to pain type, & importance of adjunctive therapy ‘a little bit of a
lot reduces side effects & increase relieve’.
2. Begin to make your patchwork quilt
1. Deliver pre/intr & post opearatively; as able, consider drug route onset/peak
action for effect & efficiency (APP, IV vs Oral)
2. Note: use of narcotic of morphine being questions due to
onset/peak/metabolism time considerations
3. Dosing considerations Age/ Gender/ tolerance/ sensitivity (1,5)
4. Dose x Pt specific Wt x 24hrs (6 The general (although this is a complex situation to
which generalization fit poorly) trend, the total clearance (CL) of drugs metabolised
by oxidation, conjugation or reduction, & also of drugs with flow-dependent hepatic
clearance, is not diminished in obesity.
Practical guidelines for dosage adjustment are proposed. For drugs with distribution
restricted to lean tissues, the loading dose should be based on the ideal
bodyweight of patients. For drugs markedly distributed into fat tissue the loading
dose is based on total bodyweight
Obese patients drug dosing is difficult, as dosages based on pharmacokinetic data obtained in
normal-weight individuals could induce errors. Physiopathological modifications in the obese can
affect drug tissue distribution & elimination. Body constitution is characterised by a higher
percentage of fat & a lower percentage of lean tissue & water. Despite cardiac output & total
blood volume increasing, the blood flow per gram of fat is less than in nonobese individuals.
Histological hepatic alterations are commonly reported in morbidly obese individuals. A higher
glomerular filtration rate is also observed.
Most of the pharmacokinetic information concerning obesity deals with distribution. Published
data concerning molecules with moderate and weak lipophilicity are homogeneous. In obese
compared with normal weight individuals, the total volume of distribution (Vd) is moderately
increased (aminoglycosides, caffeine) or similar (H2-blockers, neuromuscular blockers), but the
Vd corrected by kilogram of actual bodyweight is significantly smaller. These drugs distribute to a
limited extent in excess bodyweight.
For highly lipophilic drugs, despite this common characteristic, discrepancies in distribution in
obesity exist between drugs belonging to different pharmacological classes. Some drugs show a
clear augmentation of Vd and elimination half-life (benzodiazepines, carbamazepine,
trazodone, verapamil, sufentanil), indicating a marked distribution into adipose tissue. For
others, Vd and Vd/kg are decreased (cyclosporin, propranolol), suggesting that factors others
than lipid solubility intervene in tissue distribution.
The general (although this is a complex situation to which generalization fit poorly) trend, the total
clearance (CL) of drugs metabolised by oxidation, conjugation or reduction, & also of drugs
with flow-dependent hepatic clearance, is not diminished in obesity.
Usually CL is identical in obese & nonobese individuals, sometimes it is increased in obesity (
prednisolone, some benzodiazepines). With some drugs a significant reduction in CL is observed
in obese individuals (methylprednisolone, propranolol). Renal clearance of aminoglycosides and
cimetidine increases in obese individuals.
Practical guidelines for dosage adjustment are proposed. For drugs with distribution restricted to
lean tissues, the loading dose should be based on the ideal bodyweight of patients. For drugs
markedly distributed into fat tissue the loading dose is based on total bodyweight.
Adjustment of the maintenance dose depends on possible changes in CL. In some cases (atracurium,
prednisolone) dosage adjustment does not follow these recommendations, owing to pharmacodynamic
12
data. (Clinical Pharmacokinetics August 1993, Volume 25, Issue 2, pp 103-114 Date: 04 Nov 2012 Clinical
Pharmacokinetics of Drugs in Obesity Georges CheymolSummary
Slide (27) 23 Pain window diagrams
Slide (28) 24 Tree of analgesia
So how do we know what drugs to use: understanding the different pharmogenics of each sub
group of analgesia and their sites of action in the pain pathways will help. However this is a very
complex process as new areas of pain pathway sites of actions are being discovered almost daily.
Nevertheless drawing a line in the sand & starting somewhere is required. This knowledge is then
coupled with either an understanding of the ascending and descending and brain registration
areas functions in pain pathway interruption and modulation. In the late 1960’s the was the Gate
Theory – today this has grown markedly . (Far to broad a topic to cover in this presentation.
However the ANZCA Acute pain management book has done a lot of the leg work if you can
achieve an effective thorough pain assessment.
Lipid soluble narcotics (hydromorphone (Dilaudid), fentanyl) Water soluble narcotics
(preservative-free (PF) morphine, Duramorph
Why Use Opioids
• Mode of Action:
– Mimic action of endorphins.
– Attach to receptor sites to produce analgesia.
– Majority of receptor sites are found within the substantia gelatinosa of the dorsal
horn (spinal cord).
– Inhibit the release of substance P a neurotransmitter required for nociceptive
transmission.
• Opioid Recptors
Receptor Action
Mu 1
Analgesia, euphoria and dependence
Mu 2
Respiratory depression, bradycardia, purities, miosis,
nausea and vomiting, inhibition of gut motility
Kappa
Analgesia, sedation, miosis
Delta
Analgesia, dysphoria
sigma
Dysphoria, hallucinations, mydriasis
Achieving analgesia in the recovery room Opioids and Adjunctive therapy
• Maximize regional analgesia
• Analgesia is titrated to patient’s report of pain and functional ability.
• Analgesia frequently achieved with opioid loading doses(s) with consideration given to:
– sedation score, respiration rate, BP, and age
• Use Adjunctive: paracetamol, NSAID, Tramadol, and ketamine may also be appropriate.
APP Order
• Morphine 1-2 mg 5 minutely up to 10 mg PRN
• Fentanyl 20-40 mcg 5 min. up to 200 mcg PRN
Notice which pain settles with opioid. Is there a pain that appears not to be responsive?
Has a non-opioid been considered?
Opioid Recovery room loading
• Small amounts often to gain rapid analgesia
• Peak effect of morphine ~ 15 minutes
13
•
•
•
Load then allow time for medication to peak
Minimum wait of 20- 30 minutes in recovery following parenteral opioid administration
Ketamine improves analgesia in patients with severe pain that is poorly responsive to
opioids (level 11)
ANZCA 2005
Practice points
• Opioid requirement decreases with increasing age
• Continuous Intravenous Infusions
• Difficult to predict the infusion rate required to achieve consistent analgesia in each
individual.
• It takes 5 half-lives of a drug to reach a constant plasma drug concentration following
changes in infusion rate
• Programmed bolus doses should be used to achieve patient comfort, before rate changes.
Practice Points Pain and opioids
• Pain acts as a physiological antagonist to the central depressant effects of opioids
• As tolerance develops to the analgesic effect, so to does a greater tolerance develop to the
respiratory depressant effect.
• Respiratory effects of opioids
• May produce a decrease in tidal volume and respiratory rate, or changes in respiratory
rhythm.
• Respiratory depression more likely when:
– first dose is given
– pain subsides (e.g. IDC insertion)
– drug dose error
– the dose not reviewed in renal failure
Adverse effects of opioids
– CNS:sedation;euphoria ;constriction of pupils (miosis)
– GIT Emesis stimulation of the chemoreceptor trigger zone in the medulla.
– worst in ambulatory patients.
– Constipation:delayed gastric emptying, inhibition of bowel motility.
– Urinary retention: increased tone in the bladder sphincter
– CVS: Hypotension- Arteriole and vein vasodilatation;
– histamine release:Pruritus; histamine release which may result in local or
generalised itching, not associated with a rash.
– Allergy: rare, but similar to other allergic reactions.
Management options for opioid induced side effects.
• Decrease the dose of opioid (e.g. PCA dose).
• Regular concurrent use of other analgesics and non drug therapies.
• Monitoring sedation levels will help prevent clinically significant respiratory depression.
• Decrease the dose of opioid if constantly drowsy thus preventing respiratory rate
depression
• Sedation and respiratory depression can be exaggerated by the co - administration of e.g.
diazepam, temazepam, or prochlorperazine with an opioid.
•
.
Opioid requirement decreases with increasing age
Continuous Intravenous Infusions
• Difficult to predict the infusion rate required to achieve consistent analgesia in each individual.
• It takes 5 half-lives of a drug to reach a constant plasma drug concentration following changes
in infusion rate
14
• Programmed bolus doses should be used to achieve patient comfort, before rate changes.
Pain and opioids
• Pain acts a a physiological antagonist to the central depressant effects of opioids
• As tolerance develops to the analgesic effect, so to does a greater tolerance develop to the
respiratory depressant effect.
Respiratory effects of opioids
• May produce a decrease in tidal volume and respiratory rate, or changes in respiratory rhythm.
• Respiratory depression more likely when:
– first dose is given
– pain subsides (e.g. IDC insertion)
– drug dose error
– the dose not reviewed in renal failure.
STATEMENT OF EVIDENCE
• As significant background and /or intermittent hypoxaemia may occur for a number of days
postoperatively, Supplemental oxygen is recommended for at least the first 48-72 hours
following major surgery and in elderly or high-risk patients regardless of the analgesic method
used.
NHMRC Reader et al 1992a
Adverse effects of opioids
• Central Nervous system
– sedation
– euphoria
– constriction of pupils (miosis)
• Emesis
– stimulation of the chemoreceptor trigger zone in the medulla.
– worst in ambulatory patients.
• Constipation
– delayed gastric emptying, inhibition of bowel motility.
• Urinary retention
– increased tone in the bladder sphincter
• Hypotension
– arteriole and vein vasodilatation
– histamine release
• Pruritus
– histamine release which may result in local or generalised itching, not associated with a rash.
• Allergy
– rare, but similar to other allergic reactions.
Management options for opioid induced side effects.
15
•
•
•
•
•
Decrease the dose of opioid (e.g. PCA dose).
Regular concurrent use of other analgesics and non drug therapies.
Monitoring sedation levels will help prevent clinically significant respiratory depression.
Decrease the dose of opioid if constantly drowsy thus preventing respiratory rate depression
Sedation and respiratory depression can be exaggerated by the co - administration of e.g.
diazepam, temazepam, or prochlorperazine with an opioid.
Morphine
• Gold standard
• Receptors: Mu +++ kappa + delta + agonist
• short half life 2-3 hours.
• Two main metabolites M3G and M6G, M6G is approximately twice as potent an analgesic
as morphine.
Bupamorphine 7 days 72 hr to peak
• Partial agonist may antagonize the effects of a previously administered agonist Opioids depending on
– proportion of receptors occupied
– time interval between the administration of the two drugs
–
Buprenorphine patches are available as low-dose 7d release patches or in higher dose
patches replaced every 72hr.
Steady plasma concentrations occur on average 12hr after application of the transdermal
patch.
Dangerously high plasma concentrations can occur if patients are actively warmed whilst
wearing a transdermal patch, also pressure sensitive
BD label checking and signing safe guide
• Example: Buprenorphine was compared with naloxone for reversal of prepoperative
fentanyl (Boysen K et al 1988)
•
Acute Pain in Buprenorphine Maintained Patients
Use some form of opioid maintenance medication prefer Tramadol
Acute pain in hospitalized patient
provide analgesia as indicated for the condition
Caution: avoid high dose analgesic medication compounded with paracetamol in
patient with Hepatitis B or C
consider maintenance with methadone pre operative 7/7 weaning Norspan
Methadone—long-acting pure opioid agonist.
In the acute pain setting methadone should be continued at the same dose.
If the patient is unable to take methadone orally, substitution with parenteral methadone or
other opioids may be required in the short term
Oxycodone
• Synthetic opioid with better oral bioavailability than morphine and a slightly longer duration
of action than oral morphine.
Receptors: Mu+++, Kappa+ and Delta+ agonist
•
• 20mg oral oxycodone ~ 10 mg IM morphine
• Oral oxycodone will take ~ 40 minutes to act
Also available in a control release tablet – 40% of drug dose is released in first hour(
enteric coated (functioning gut required)
Synthetic opioid with better oral bioavailability than morphine and a slightly longer duration
of action than oral morphine.
•
16
Codeine
Receptor: Mu+++ kappa+ and delta+ agonist
Well absorbed orally but a low affinity for opioid receptors.
Owes its analgesic effects to conversion by CYP2D6 to morphine, a pathway that is inactive
in about 10% of the population.
Number Needed to Treat = 16.7 for 60mg dose and 1.9 for combination 1gm paracetamol
with 60mg codeine.
Synthetic Opioids
Pethidine Rarely used
`synthetic opioid
Receptor Mu ++ kappa+ and delta + agonist.
• elimination half life 2 - 6 hours.
• norpethidine is its main metabolite, it has a long half life of 15 - 20 hours and will provide
analgesia.
• build up of norpethidine can cause irritability, tremors and convulsions.
• Pethidine has been reported to more than double the risk of delirium.
• Muscle fibrosis can occur when administered by IM route
Intra Operative
Remifentanil
• Ultra short acting synthetic opioid
• half-life is ~ 3 minutes. Usually delivered by infusion and rapid recovery when stopped.
• Long acting analgesics may be needed before discontinuation.
• Not for epidural or spinal route use as contains glycine
Alfentanil
• derived from fentanyl
• onset of analgesia in 15-120 seconds
• duration of analgesia is dose related.
• when compared to fentanyl, alfentanil is 25% more potent.
• elimination half life of 90 minutes is significantly shorter than other opioids.
• secondary serum peak levels reported.
•
•
Fentanyl
• Receptors: Mu+++ and delta+ agonist
• Onset of analgesia 30 - 120 seconds
Half life 1-2 hours
Peak onset 1 -5min, duration 30min, metabolite <72hrs (lipid soluable)/inert
• No active metabolite - safer opioid in the presence of renal impairment.
• Secondary serum peak levels reported @ 4hr (caution with continuos IV infusion ) leak
taken up in fat cell with rebound release reported
• Life threatening respiratory depression has been reported when transdermal or IV route
fentanyl has been administered to opioid naïve patients (particularly early patch design)
• spinal anaesthesia. Fentanyl 10–30µg has a rapid onset (10–20 min) and a short duration
• Transdermal administration. Very lipid-soluble opioids are absorbed through skin. Fentanyl
patches are available in five sizes (12–100µg/hr) and patches are replaced every 72hr of
action (4–6hr)
Tramadol racemic mixture
• synthetic centrally acting opioid-like drug
17
•
•
•
•
•
•
•
•
Less than half of its analgesic activity is at the µ-opioid receptor. It inhibits noradrenaline
and serotonin uptake at nerve terminals, thereby enhancing the inhibitory pathway.
Lower tolerance & abuse potential, less respiratory depression, & constipation compared to
other opioids reported.
Metabolised in the liver & excreted in the kidney. Main metabolite of tramadol is Odesmethyltramadol (M1) which is more potent. Formation of M1 also depends on the
presence of CYP2D6 within the cytochrome P450 system (see codeine).
Parenteral load give slowly (15-30 minutes) to reduce incidence of adverse reaction
Nausea and dizziness - very common > 1/10
Drug interactions with anti-convulsants, and anti-depressants .Serotonin syndrome
Minimal respiratory and gastro-intestinal stasis.
Drug interaction with warfarin, and not recommended if coexisting condition of epilepsy
exists
Equianalgesia (note equianalgesia differ from text to text slightly)
Drug
Oral dose (mg)
Parental dose
(mg)
Morphine
30
10
Pethidine
300
75
Oxycodone
20 – 30
Codiene
200 - 240
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
Systemic Medications: Opioids
Opioid Receptors: ì, ê and ä receptors
Location of receptors: Periphery following inflammation;Spinal cord dorsal horn;
Supraspinally in the brainstem, thalamus and cortex; PAG, nucleus raphe magnus and RVM
in descending pathway
Mechanism of Action:
Spinal
++
Inhibition of Ca influx presynaptically
+
Enhacing K efflux postsynaptically
Activation of descending inhibitory GABAergic circuit
Peripheral
Inhibition of release of pro inflammatory and pro nociceptive substances
Adverse Effects & Problems: Respiratory Depression;Nausea and
Vomiting;Sedation;Urinary Retention
Euphoria/Dysphoria;Constipation;Tolerance;Dependence and Addiction
Transdermal Fentanyl Delivery System (Ionsys)
Needle free, patient activated system for in-hospital use
Iontophoresis
Low intensity electrical field used to transport fentanyl across skin into circulation
Each double click delivers 40mcg over 10 min; For us in adults > 18 years; Used for 24
hours or 80 doses
Tramadol: Reasemtic noradrenaline /serotonin
Moderate affinity ì receptor agonist 5ht3 agonist.
Acts on spinal modulating pathways
Inhibition of neuronal NA and Serotonin uptake
Stimulation of presynaptic serotonin release
Adverse Effects:
Nausea & Vomiting: Ondansetron interferes with analgesic effect
Non addictive, less sedation
Dose: 3 mg/kg IM/IV/PO for moderate to severe pain
18
•
•
•
•
•
•
•
•
Buprenorphine:Semisynthetic, Agonist-Antagonist
Routes of administration:
IV, IM, Neuraxial, SC, SL, Trasdermal
Useful in morphine intolerant patient;Ceiling effect for respiratory depression, but not for
analgesia.
Antiflammatory action:Useful in intra-articular injections; Prolongs duration of analgesia in
peripheral nerve blocks with LA
Methadone:Synthetic broad spectrum opioid;Mu receptor agonist;NMDA
antagonist;Inhibitor of monoamine transmitters
Useful in treatment of neuropathic pain; Orally well absorbed; No dose adjustment in renal
disease; Drug most commonly used for opioid rotation
•
•
ANZCA’s Opioid Key messages
1. Dextropropoxyphene has low analgesic efficacy (U) (Level I [Cochrane Review]).
2. Tramadol is an effective treatment for neuropathic pain (U) (Level I [Cochrane Review]).
3. Gabapentin, non-steroidal NSAIDs and ketamine are opioid-sparing medications and reduce
opioid-related side effects (N) (Level I).
4. In appropriate doses, droperidol, metoclopramide, ondansetron, tropisetron, dolasetron,
dexamethasone, cyclizine and granisetron are effective in the prevention of postoperative nausea
and vomiting (N) (Level I [Cochrane Review]).
5. Alvimopan and methylnaltrexone are effective in reversing opioid-induced slowing of
gastrointestinal transit time and constipation (N) (Level I [Cochrane Review]).
6. Droperidol, dexamethasone and ondansetron are equally effective in the prevention of
postoperative nausea and vomiting (U) (Level I).
7. Paired combinations of 5HT3 antagonist, droperidol or dexamethasone provide superior
prophylaxis of postoperative nausea and vomiting than either compound alone (N)(Level I).
8. Naloxone, naltrexone, nalbuphine, droperidol and 5HT3 antagonists are effective
treatments for opioid-induced pruritus (N) (Level I).
9. Opioids in high doses can induce hyperalgesia (N) (Level I).
10. Tramadol has a lower risk of respiratory depression and impairs gastrointestinal motor function
less than other opioids at equianalgesic doses (U) (Level II).
11. Pethidine is not superior to morphine in treatment of pain of renal or biliary colic (U) (Level II).
12. Morphine-6-glucuronide is an effective analgesic (N) (Level II).
13. In the management of acute pain, one opioid is not superior over others but some opioids are
better in some patients (U) (Level II).
14. The incidence of clinically meaningful adverse effects of opioids is dose-related (U) (Level II).
15. High doses of methadone can lead to prolonged QT interval (N) (Level II).
16. Haloperidol is effective in the prevention of postoperative nausea and vomiting (N) (Level II).
17. Opioid antagonists are effective treatments for opioid-induced urinary retention (N) (Level
II).PTER 4
18. In clinically relevant doses, there is a ceiling effect for respiratory depression with
buprenorphine but not for analgesia (N) (Level III-2).
19. Assessment of sedation is a more reliable way of detecting early opioid-induced
respiratory depression than a decreased respiratory rate (S) (Level III-3).
19
20. The evidence for risk of cardiac arrhythmias following low-dose droperidol is poor (N) (Level
III-3).
21. In adults, patient age rather than weight is a better predictor of opioid requirements, although
there is a large interpatient variation (U) (Level IV).
22. Impaired renal function and the oral route of administration result in higher levels of the
morphine metabolites morphine-3-glucuronide and morphine-6-glucuronide with increased risk of
sedation and respiratory depression (S) (Level IV).
The following tick box þ represents conclusions based on clinical experience and expert opinion.
;; The use of pethidine (U) and dextropropoxyphene (N) should be discouraged in favour of other
opioids.
Paracetamol
• Used as a component of multimodal therapy.
• Importance of around the clock regular dosing.
• Intravenous route option (give over 15 minutes 6/24hr)
• Commence ASAP
• 4g daily in adult (warfarin interaction at 3 g per week ↑ INR potential)
•
ANZCA’s Paracetamol Key Message
Paracetamol (acetaminophen) is the only remaining para-aminophenol used in clinical practice
and is an effective analgesic (see below) and antipyretic. It is absorbed rapidly and well from the
small intestine after oral administration with a bioavailability of between 63% and 89% (Oscier &
Milner, 2009). It can also be given rectally and intravenously (see below and Section 6).
The mechanism of action of paracetamol remains unclear. In contrast with opioids,
paracetamol has no known endogenous binding sites, and unlike NSAIDs, apparently does not
inhibit peripheral cyclo-oxygenase activity. There is increasing evidence of a central
antinociceptive effect. Although the mechanism of analgesic efficacy of paracetamol remains
elusive, it may involve direct and indirect inhibition of central cyclo-oxygenases, but the activation
of the endocannabinoid system and spinal serotonergic pathways also appear to be essential
(Bertolini et al, 2006; Botting, 2006; Pickering et al, 2006; Mallet et al, 2008; Pickering et al, 2008).
Paracetamol has also been shown to prevent prostaglandin production at the cellular
transcriptional level, independent of cyclo-oxygenase activity (Mancini et al, 2003).
As one of the mechanisms of action of paracetamol appears to be linked to the serotonergic
system, it is possible that other drugs with serotonergic effects could affect pain relief. In
volunteers, coadministration of tropisetron or granisetron blocked the analgesic effects of
paracetamol (Pickering et al, 2006 Level II; Pickering et al, 2008 Level II). The significance of this
in the clinical setting has not yet been elucidated.
NSAIDs
The term NSAIDs is used to refer to both nsNSAIDs and coxibs (COX-2 selective inhibitors).
NSAIDs have a spectrum of analgesic, anti-inflammatory and antipyretic effects and are effective
analgesics in a variety of acute pain states. Many effects of NSAIDs can be explained by inhibition
of prostaglandin synthesis in peripheral tissues, nerves, and the CNS (Botting, 2006). However,
NSAIDs and aspirin may have other mechanisms of action independent of any effect on
prostaglandins, including effects on basic cellular and neuronal processes. Prostaglandins are
produced by the enzyme prostaglandin endoperoxide (PGH) synthase,
which has both cyclo-oxygenase and hydroperoxidase sites. Two subtypes of cyclo-oxygenase
enzyme have been identified – the ‘constitutive’ COX-1, the ‘inducible’ COX-2: a COX-3 is also
being investigated (Simmons et al, 2004; Gajraj & Joshi, 2005; Botting, 2006; Kam & So, 2009).
20
Prostaglandins have many physiological functions including gastric mucosal protection, renal
tubular function and intrarenal vasodilation, bronchodilatation, production of endothelial
prostacyclin that leads to vasodilation and prevents platelet adhesion, and platelet thromboxane
that results in platelet aggregation and vessel spasm. Such physiological roles are mainly
regulated by COX-1 and are the basis for many of the adverse effects associated with ns NSAID
use. Tissue damage induces COX-2 production leading to synthesis of prostaglandins that result
in pain and inflammation, and COX-2 induction within the spinal cord may play a role in central
sensitisation. COX-2 may also be ‘constitutive’ in some tissues,
including the kidney, cardiovascular system and brain (Kam & So, 2009). NsNSAIDs are
‘nonselective’ cyclo-oxygenase inhibitors that inhibit both COX-1 and COX-2. Aspirin acetylates
and inhibits cyclo-oxygenase irreversibly but nsNSAIDs are reversible inhibitors of the enzymes.
The coxibs have been developed to inhibit selectively the inducible form (Simmons et al, 2004;
Gajraj & Joshi, 2005; Botting, 2006).
NSAIDs
Mechanism of Action:Inhibition of Cyclo-oxygenase enzymes (type 1 & 2);Reduce
concentrations of PGE2 :
Sensitise peripheral nociceptors to histamine and bradykinin;Centally Increase Substance P and
Glutamate Increase sensitivity of second order neurons Decrease NTs from descending pathway
Benefits:Opioid Sparing; Reduced incidence of opioid side effects: Anti-inflammatory effects
Adverse Effects: Platelet Dysfunction; Gastrointestinal Ulceration; Nephrotoxicity; Impaired bone
healing; Hypersensitivity
Non Steroidal anti-inflammatory drugs.(NSAID’s)
• All have three properties in common
– analgesic
– anti-pyretic
– anti inflammatory
• Primary action is the inhibition of the production of cyclo-oxygenase (COX) and thus the
inhibition of the production of prostaglandins, prostacyclin and thromboxane
• Prostaglandin function
– released in response to cell damage
– sensitise and activate nociceptors to bradykinin
– some are hyperalgesic PGI2 and PGE2
– PGE2 inhibits acid secretion and increases mucous secretion in the stomach.
– Exert a pyretic effect through the hypothalamus
– vasodilatation and diuresis within the kidney
– responsible for many endocrine functions
Generic name
– Ibuprofen (400mg)
– Diclofenac (50mg)
– Naproxen
– Indomethacin
– Ketoralac 10mg
– Piroxicam (Feldene)
NNT
2.7
2.3
Elimination 1/2 life Hrs
2
1
15
6
6
53
21
Non Steroidal Anti -Inflammatory Drugs
• Used with caution in the elderly.
• The route of administration does not influence the potential for serious side effects.
• Safer to use the NSAIDs with lowest observed risk e.g Ibuprofen, Diclofenac.
Contraindications must be respected.
• Prior gastric ulceration
• Concurrent use of oral anticoagulants.
• Interaction with Ace inhibitors and B blockers.
• Concurrent use of gentamicin.
NSAID’s
• Effective for mild to moderate pain
• Reduces opioid requirement
• Drug of choice after day case surgery.
• Selective COX 2 inhibitors e.g meloxicam
(elim. 1/2 life 20 hrs), IV paracoxib (single dose given in theatre) replaces celebrax, (elim. ½ life
10 – 20 min – is a prodrug (no effects on body needs to be metabolized to have effect) –
converted to valdecoxib (1/2 life 6 – 8hrs).
Cox 2 inhibitors have less GIT side effects, does not affect platelet aggregation and
thromboxane production.
Non Steroidal anti-inflammatory drugs( NSAID’s)
• Most exhibit a spectrum of action including:
• analgesic
• anti-pyretic
• anti-inflammatory
• anti-platelet
• Primary action is the inhibition of the production of cyclo-oxygenase (COX) and thus the
inhibition of the production of prostaglandins, prostacyclin and thromboxane
• Alone are effective for mild to moderate pain and are seen as a component of multimodal
therapy for severe pain.
• May reduce opioid requirements by up to 30%
• ? Drug of choice after day case surgery.
• The route of administration does not influence the potential for serious side effects
• Selective COX 2 inhibitors e.g celecoxib
– has little or no effect on COX 1 at therapeutic doses.
•
•
Potential side effects
– renal dysfunction
– gastric irritation
– reversible platelet dysfunction.
– trigger asthma
Safer to use the NSAID’s with shorter half life e.g. Diclofenac, Ibuprofen, or COX 2.
IV - Parecoxib sodium (dynastat) Cox 2 (only given in theatre)
22
•
Contraindications must be respected.
Paracetamol &NSAIDs Key messages
1. Paracetamol is an effective analgesic for acute pain; the incidence of adverse effects
comparable to placebo (S) (Level I [Cochrane Review]).
2. Non-selective NSAIDs are effective in the treatment of acute postoperative and low back pain,
renal colic and primary dysmenorrhoea (N) (Level I [Cochrane Review]).
3. Coxibs are effective in the treatment of acute postoperative pain (N) (Level I [Cochrane
Review]).
4. With careful patient selection and monitoring, the incidence of nsNSAID-induced
perioperative renal impairment is low (U) (Level I [Cochrane Review]).
5 Non-selective NSAIDs do not increase the risk of reoperation for bleeding after
tonsillectomy in paediatric patients (Q) (Level I [Cochrane Review]).
6. Coxibs do not appear to produce bronchospasm in individuals known to have
aspirinexacerbated respiratory disease (U) (Level I).
7. In general, aspirin increases bleeding after tonsillectomy (N) (Level I).
8. Non-selective NSAIDs given in addition to paracetamol improve analgesia compared with
paracetamol alone (U) (Level I).
9. Paracetamol given in addition to PCA opioids reduces opioid consumption but does not result in
a decrease in opioid-related side effects (N) (Level I).
10. Non-selective NSAIDs given in addition to PCA opioids reduce opioid consumption and the
incidence of nausea, vomiting and sedation (N) (Level I).
11. Non-selective NSAIDs and coxibs are effective analgesics of similar efficacy for acute pain (U)
(Level I).PTER 4
12. Preoperative coxibs reduce postoperative pain and opioid consumption, and increase patient
satisfaction (N) (Level I).
13. Coxibs given in addition to PCA opioids reduce opioid consumption but do not result in a
decrease in opioid-related side effects (N) (Level I).
14. Coxibs and non-selective NSAIDs have similar adverse effects on renal function (U) (Level I).
15. Non-selective NSAIDs do not significantly increase blood loss after tonsillectomy but do
increase the need for reoperation due to bleeding (N) (Level I).
16. Parecoxib and/or valdecoxib compared with placebo do not increase the risk of
cardiovascular adverse events after non-cardiac surgery (N) (Level I).
17. Coxibs and non-selective NSAIDs are associated with similar rates of adverse
cardiovascular effects, in particular myocardial infarction; naproxen may be associated with a
lower risk than other non-selective NSAIDs and celecoxib may be associated with a lower risk
than other coxibs and non-selective NSAIDs overall (N) (Level I).
18. Perioperative non-selective NSAIDs increase the risk of severe bleeding after a variety of other
operations compared with placebo (N) (Level II).
19. Coxibs do not impair platelet function; this leads to reduced perioperative blood loss in
comparison with non-selective NSAIDs (S) (Level II).
20. Short-term use of coxibs results in gastric ulceration rates similar to placebo (U) (Level II).
23
21. Use of parecoxib followed by valdecoxib after coronary artery bypass surgery increases the
incidence of cardiovascular events and is therefore contraindicated (S) (Level II). The following
tick boxes þ represent conclusions based on clinical experience and expert opinion.
;; Adverse effects of NSAIDs are significant and may limit their use (U).
;; The risk of adverse renal effects of non-selective NSAIDs and coxibs is increased in the
presence of factors such as pre-existing renal impairment, hypovolaemia, hypotension, use of
other nephrotoxic agents and ACE inhibitors (U).
Inhalational agents Key messages
1. Nitrous oxide has some analgesic efficacy and is safe during labour (U) (Level I).
2. Nitrous oxide is an effective analgesic agent in a variety of other acute pain situations (U) (Level
II).
3. Methoxyflurane, in low concentrations, may be an effective analgesia in the hospital and
prehospital setting (N) (Level IV).APTER 4
The following tick boxes þ represent conclusions based on clinical experience and expert opinion.
;; Neuropathy and bone marrow suppression are rare but potentially serious complications of
nitrous oxide use, particularly in at-risk patients (U).
;; The information about the complications of nitrous oxide is from case reports only. There are no
controlled studies that evaluate the safety of repeated intermittent exposure to nitrous oxide in
humans and no data to guide the appropriate maximum duration or number of times a patient can
safely be exposed to nitrous oxide. The suggestions for the use of nitrous oxide are extrapolations
only from the information above. Consideration should be given to duration of exposure and
supplementation with vitamin B12, methionine, and folic or folinic acid (U).
;; If nitrous oxide is used with other sedative or analgesic agents, appropriate clinical
monitoring should be used (U).
NMDA-receptor antagonists
NMDA receptor/ion channel complexes are sited peripherally and centrally within the nervous
system (De Kock & Lavand’homme, 2007). Activation of NMDA receptors via glutamate release
from excitatory synapses augments the propagation of nociceptive information and is linked to
learning and memory, neural development and neuroplasticity, as well as acute and chronic pain
states and opioid-induced tolerance. At the spinal level, NMDA receptor activation results in the
development of central sensitisation manifested clinically as hyperalgesia and allodynia
(De Kock & Lavand’homme, 2007; Hocking et al, 2007). The NMDA-receptor antagonists
ketamine, dextromethorphan, amantadine, memantine and
magnesium have been investigated for the management of acute pain.
NMDA antagonist Ketamine
• Used as an analgesic in sub-anaesthetic doses
• Ketamine bolus loading in PAR
• May be administered as intravenous infusion - refer to protocol in Pain service folder
• NMDA receptor antagonist
• Useful in neuropathic and inflammatory induced pain, patient’s with opioid tolerance.
• Opioid sparing
Ketalar/Ketamine
24
Generic Ingredients: ketamine hydrochloride
Company Hospira Australia Pty Ltd
Pregnancy Category B3*
Permitted in sport
Use: Nonbarbiturate IV and IM anaesthetic esp for short procedures; induction prior to other
general anaesthetics; supplement to low potency agents
Contra: Hazardous raised BP conditions eg severe CV disease, heart failure, severe or poorly
controlled hypertension, recent MI, stroke history, cerebral trauma, intracerebral mass/
haemorrhage
Prec: Acute, chronic alcoholism; incr CSF pressure, IOP; psychiatric illness, neurosis; acute
intermittent porphyria; seizures; intracranial mass, lesions, head/ globe injury, hydrocephalus;
pulmonary, URTI; hyperthyroidism; hypovolaemia; dehydration; mild-mod hypertension;
tachyarrhythmias; abuse potential; sole use in pharynx, larynx, bronchial tree, visceral pain
pathway procedures; renal, hepatic impairment; cirrhosis; rapid IV admin (< 60 sec); cardiac
disease (monitor); pregnancy; lactation (should not use); others, see full PI
Adverse: Arrhythmia; incr/ decr BP, pulse; respiratory depression, apnoea, laryngospasm;
diplopia; nystagmus; emergence reaction (hallucination, illusion, delirium, confusion, excitement,
irrational behaviour); anaphylaxis; incr muscle tone; GI effects incl hypersalivation; inj site reaction
Interact: Halogenated hydrocarbon anaesthetics, barbiturates, narcotics; benzodiazepines;
ergometrine; theophylline; atracurium; tubocurarine; CNS depressants incl skeletal muscle
relaxants; thiopental; thyroid hormones; antihypertensives
Ketalar Solution for injection (S8) Ketamine (HCl); benzethonium Cl; single use vial
Dose Individualise dose; for IMI or slow (60 sec) IVI. Induction. IVI: range 1-4.5 mg/kg; 2 mg/kg
usually produces anaesthesia within 30 sec, lasting 5-10 min. IMI: range 6.5-13 mg/kg; 10 mg/kg
usually produces anaesthesia within 3-4 min, lasting 12-25 min; see full PI. Maintenance. May
admin additional incremental IV, IM doses (1/2 to full induction dose). Hepatic impairment,
cirrhosis: consider dose reduction
Pack 200 mg/2 mL [5]
Reference MIM’s online 2011
NMDA Antagonists
Ketamine:NMDA receptor antagonism theoretically reduces central sensitisation, hyperalgesia
and opioid tolreance
Currently role in postoperative pain relief is complex; Insignificant difference in pain ; Clinically
insignificant opioid sparing
Psychomimetic side effects – hallucination, nighmares
NMDA antagonist
• Ketamine
• Mechanism of action
– selective blocking agent of the excitatory receptor NMDA.
– ? other mechanisms of action
• Used in neuropathic pain states at low doses.
Ketamine is a water- and lipid-soluble drug that rapidly penetrates into the CNS. Like the
barbiturates, ketamine accumulates rapidly and then undergoes redistribution with subsequent
degradation in the liver
25
ketamine acts by interrupting association pathways between the thalamocortical and the limbic
systems
NMDA receptor antagonists:Ketamine doses (0.15–1 mg/kg),
exerts a specific NMDA blockade & hence, modulates central sensitization .(2)
Acute neuropathic pain after surgery Parenteral ketamine (NMDA receptor antagonist,
5mg/hr) & Lignocaine (neuronal membrane stabilisation, 5mg/kg over 30–40min
followed by 0.5–1.5mg/kg/hr) can be given in the acute phase to alter both
peripheral and central neuronal plasticity. Treatment may take up to a week or more.
This should be supervised by a suitably qualified pain specialist
NMDA-receptor antagonists ANZCA’s Key messages
1. Perioperative low-dose ketamine used in conjunction with patient-controlled analgesia morphine
is opioid-sparing and reduces the incidence of nausea and vomiting (N) (Level I
[Cochrane Review]).
2. In general, a perioperative low-dose ketamine infusion is opioid-sparing, but does not produce a
clinically significant reduction in pain scores or opioid-related adverse effects (S) (Level I).
3. Ketamine is a safe and effective analgesic for painful procedures in children (N) (Level I).
4. Ketamine and dextromethorphan have preventive (U) but not pre-emptive analgesic effects (N)
(Level I).
5. Magnesium does not reduce postoperative pain scores or opioid consumption and has no
preventive analgesic effect (N) (Level I).
6. Ketamine may improve analgesia in patients with severe acute pain that is poorly
responsive to opioids, although evidence is conflicting (W) (Level II).
7. Ketamine reduces postoperative pain in opioid-tolerant patients (N) (Level II).
The following tick box þ represents conclusions based on clinical experience and expert opinion.
;; The primary role of low dose ketamine is as an ‘antihyperalgesic’, ‘antiallodynic’,
‘tolerance-protective’ and preventive analgesic, rather than as an analgesic per se (N).
Antidepressant Tricyclic anti-depressants
Drug Name: Amitryptiline
Mechanism of action:
Increase available serotonin and noradrenaline by blocking reuptake.
• Increase endorphin levels
• The analgesic effect appears quicker that their antidepressant effect. (3-4 days versus 3
weeks).
• The dose required for an analgesic effect is lower that that required for their antidepressant
effect.
• They have a muscle relaxant effect in diffuse musculoskeletal pain.
• They may enhance the analgesia produced by opioids.
• They are often used for neuropathic burning pain.
• Side effects
• sedation and anticholinergic effects including dry mouth, constipation and urinary retention.
• Cardiac arrhythmias, glaucoma, weight gain and loss of libido
• start at a low dose so that patients can become accustomed to using them
• sometimes their side effects are beneficial e.g improvement in sleep due to sedation.
Antidepressant drugs ANZC’s Key messages
26
1. In neuropathic pain, tricyclic antidepressants are more effective than selective
serotonergic re-uptake inhibitors (S) (Level I [Cochrane Review]).
2. Duloxetine is effective in painful diabetic neuropathy and fibromyalgia (N) (Level I
[Cochrane Review]).
3. There is no good evidence that antidepressants are effective in the treatment of chronic low
back pain (R) (Level I [Cochrane Review]).
4. Tricyclic antidepressants are effective in the treatment of chronic headaches (U) and
fibromyalgia (N) (Level I).
5. Antidepressants reduce the incidence of chronic neuropathic pain after herpes zoster (U) (Level
II).
Note: withdrawal of previous key message:
Antidepressants reduce the incidence of chronic neuropathic pain after breast surgery This has
been deleted as the information and evidence supporting it has been withdrawn.HAPTER 4
The following tick boxes represent conclusions based on clinical experience and expert opinion.
;; Based on the experience in chronic neuropathic pain states, it would seem reasonable to use
tricyclic antidepressants and selective serotonin re-uptake inhibitors in the management of acute
neuropathic pain (S).
;; To minimise adverse effects, particularly in elderly people, it is advisable to initiate
treatment with low doses (U).
Anticonvulsant drugs
Anti-convulsants
• Drug Names:Carbamazepine /Sodium Valproate Gabapentin
• Mechanism of action
• stabilise nerve cell membranes by blockade of voltage sensitive sodium channels
• Increase brain serotonin, and GABA
• reduce evoked and spontaneous activity of spinal neurons with and without peripheral
nerve injury
• ? modulates voltage dependant calcium channels.
• Used in neuropathic pain to combat pain described as shooting / knife like.
• Side effects
• dizziness, sedation, gait disturbance, GIT upset, liver dysfunction, thrombocytopenia and
bone marrow depression.
Gabapentin does not have the above severe adverse side effects
Anti-convulsants
• Carbamazepine /Sodium Valproate
• Gabapentin
• Mechanism of action
– stabilise nerve cell membranes by blockade of voltage sensitive sodium channels
– Increase brain serotonin, and GABA
– reduce evoked and spontaneous activity of spinal neurons with and without peripheral nerve
•
injury
– ? modulates voltage dependant calcium channels.
Used in neuropathic pain to combat pain described as shooting / knife like.
27
•
Side effects
– dizziness, sedation, gait disturbance, GIT upset, liver dysfunction, thrombocytopenia and
bone marrow depression.
– Gabapentin does not have the above severe adverse side effects.
Anticonvulsant drugs Key messages
1. Gabapentin is effective in the treatment of chronic neuropathic pain (Q); lamotrigine is most
likely ineffective (N) (Level I [Cochrane Review]).
2. Carbamazepine is effective in the treatment of trigeminal neuralgia (N) (Level I [Cochrane
Review]).
3. Pregabalin is effective in the treatment of chronic neuropathic pain related to diabetic
neuropathy (N) (Level I).
4. Perioperative gabapentinoids (gabapentin/ pregabalin) reduce postoperative pain and opioid
requirements (U) and reduce the incidence of vomiting, pruritus and urinary retention, but increase
the risk of sedation (N) (Level I).
The following tick box þ represents conclusions based on clinical experience and expert opinion.
;; Based on the experience in chronic neuropathic pain states, it would seem reasonable to use
anticonvulsants in the management of acute neuropathic pain (U).
Anti-arrhythmic agents; Membrane stabilisers
• Intravenous lignocaine (Beirs Block)
• Oral mexiletine (not used in Theatre)
• Sodium channel blockers which act to suppress abnormal activity in damaged neurones,
without blocking normal nerve conduction.
Membrane stabilisers ANZCA’s Key messages
1. Both lignocaine (lidocaine) and mexiletine are effective in the treatment of chronic neuropathic
pain (S); there is no difference in efficacy or adverse effects compared with carbamazepine,
amantadine, or morphine (N) (Level I [Cochrane Review]).
2. Perioperative intravenous lignocaine reduces pain and opioid requirements following abdominal
surgery (S) as well as nausea, vomiting, duration of ileus and length of hospital stay (N) (Level I).
The following tick boxes represent conclusions based on clinical experience and expert opinion.
;; Based on the experience in chronic neuropathic pain states, it would seem reasonable to use
membrane stabilisers in the management of acute neuropathic pain (U).
;; Lignocaine (intravenous or subcutaneous) may be a useful agent to treat acute
neuropathic pain (U).
Alpha- 2 agonist Clonidine
Action:The stimulation of damaged peripheral nerve terminals by ephedrine is described as
Sympathetically maintained pain.
• Clonidine reduces the release of ephedrine on to the peripheral nerve terminal.
• Other actions unclear
Autonomic drugs which have proven beneficial in the treatment of neuropathic pain include the
alpha–2 agonists: clonidine and alpha–1 antagonists (e.g. prazosin, terazosin).
The role of the alpha-2 adrenergic system in neuropathic pain has been studied using various
pharmacological interventions and animal models.
In animal studies, alpha-2 adrenergic agonists produce analgesia by actions in the periphery,
28
supraspinal central nervous system and in the spinal cord.clonidine is believed to produce
analgesia at the spinal level, in part through stimulation of cholinergic interneurones in the spinal
cord. This cholinergic mediation of analgesia, as reflected by cerebrospinal fluid acetylcholine
concentration, is activated by intrathecal, but not IV, injection of clonidine.
However, clonidine has been shown to produce analgesia to experimental pain stumuli after
systemic and epidural injection. However, clinical studies of systemic clonidine for analgesia have
yielded conflicting results. Alpha-2 adrenergic agonists produce sedation and reduced blood
pressure in addition to analgesia. Small doses (50 mg) of clonidine may reduce blood pressure
more after an intrathecal than an IV injection.
Clonidine has also been shown to potentiate the neuropathic pain-relieving action of the NMDA
antagonist MK–801 while preventing its neurotoxic and hyperactivity side-effects.Clonidine is
available in several different dosage forms and can be administered orally, transdermally or
spinally. Conversely, systemic dexmedetomidine, another alpha-2 adrenergic agonist, has been
shown neither to prevent nor attenuate neuropathic pain behaviour in rats. Dexmedetomidine has
an affinity for all three alpha-2 adrenergic receptor subtypes. The role of the different subtypes of
alpha-2 adrenoreceptors remains unclear.
ArticleDate:20050907
SiteSection: Article All rights reserved © 2011. Designed by AnaesthesiaUK.
Clonidine, an a2-adrenergic agonist, has been shown to prolong the action of local anaesthetics
especially when used in the intrathecal or epidural space. It activates a negative-feedback
mechanism via its action on a2-receptors, which decreases catecholamine release. This
modulates input at the dorsal horn. Clonidine also has cholinergic effects and increases the
amount of acetylcholine available centrally. Its main adverse effects are hypotension, bradycardia
and sedation. When combined with ropivacaine 0.1%, as little as 25 µg of clonidine in the epidural
space has been associated with bradycardia and sedation. However, hypotension was significant
only with doses of more than 75 µg epidurally.
Clonidine has also been shown to prolong local anaesthesia in peripheral blocks, probably by
direct peripheral action. A recent study using only Clonidine for interscalene blocks showed
significantly longer analgesia when compared with a group receiving Clonidine subcutaneously.3
The exact mechanism of peripheral action is unknown. Clonidine may act on peripheral a2receptors or reduce the vascular uptake of local anaesthetic by its vascular adrenergic effects.
Clonidine may exert a peripheral analgesic action by causing the release of enkephalin-like
compounds. Doses up to 150 µg administered peripherally have minimal side-effects.
Anaesthesia UK : Local Anaesthetic Pharmacologywww.frca.co.uk/article.aspx?articleid=100505 α2 Adrenergic Agonists ;Primarily preoperative and intraoperative use
Clonidine: α2 agonist, α2: α1 biding 220:1; PO, IV, TD, Neuraxial routes;Reduced postoperative
opioid requirement
Side Effects: Sedation, Bradycardia, hypotension
Dexmedetomedine: Superselective α2 agonist: α2:α1 binding 1620:1;Supraspinal, Spinal &
Peripheral action;
No respiratory depression;
Alpha- 2 agonist
• The stimulation of damaged peripheral nerve terminals by ephedrine is described as
Sympathetically maintained pain. Clonidine reduces the release of ephedrine on to the
peripheral nerve terminal.
• Other actions unclear
• Clonodine)(Have sedative, anxiolytic, analgesic and haemodynamic-stabilising effects. They act
on alpha2 adrenoreceptors in the CNS to reduce noradrenergic activity, and also on receptors in
other tissues. The main site of analgesic action is thought to be the spinal cord. Stimulation of
29
imidazoline receptors results in a central hypotensive and antiarrhythmic action.)
Alpha-2 agonists Key message
1. The use of systemic alpha-2-agonists consistently improves perioperative opioid analgesia but
the frequency and severity of side effects may limit their clinical usefulness (U) (Level II).
Magnesium,
Magnesium :30–50 mg/kg,
•
•
•
•
•
•
•
•
– followed by 7–15 mg/kg/h IV
– In the Peripheral Nervous System it interferes with the release of neurotransmitters
at all synaptic junctions & potentiates the action of local anesthetics(3)
Peripheral nervous system: interferes with the release of neurotransmitters at all synaptic
junctions & potentiates the action of local anesthetics.[40]
At the neuromuscular junction, magnesium concentrations of 5 mmol/L cause significant
presynaptic neuromuscular blockade and enhance the action of the nondepolarizing muscle
relaxants.[40]
It can precipitate severe muscle weakness in patients with Eaton-Lambert syndrome, patients
with myasthenia gravis, or patients pretreated with a small dose of a defasciculating agent.[40]
Magnesium prolongs the action of depolarizing neuromuscular blocker drugs (e.g.,
succinylcholine); administration before the use of succinylcholine prevents the release of
potassium provoked by the neuromuscular blocking drug (see Chapter 29).
Magnesium has several important pharmacologic actions.
Its route of elimination is renal, and any patient who is oliguric or in a reduced urine
output state requires downward dosing adjustment of magnesium therapy.
Magnesium should be regarded as a cardiovascular drug, first and foremost, with
calcium antagonistic and antiadrenergic properties that may be accompanied by
minimal myocardial depression.[40]
Magnesium :30–50 mg/kg,
•
•
•
•
•
•
•
•
– followed by 7–15 mg/kg/h IV
– In the Peripheral Nervous System it interferes with the release of neurotransmitters
at all synaptic junctions & potentiates the action of local anesthetics(3)
Peripheral nervous system: interferes with the release of neurotransmitters at all synaptic
junctions & potentiates the action of local anesthetics.[40]
At the neuromuscular junction, magnesium concentrations of 5 mmol/L cause significant
presynaptic neuromuscular blockade and enhance the action of the nondepolarizing muscle
relaxants.[40]
It can precipitate severe muscle weakness in patients with Eaton-Lambert syndrome, patients
with myasthenia gravis, or patients pretreated with a small dose of a defasciculating agent.[40]
Magnesium prolongs the action of depolarizing neuromuscular blocker drugs (e.g.,
succinylcholine); administration before the use of succinylcholine prevents the release of
potassium provoked by the neuromuscular blocking drug (see Chapter 29).
Magnesium has several important pharmacologic actions.
Its route of elimination is renal, and any patient who is oliguric or in a reduced urine
output state requires downward dosing adjustment of magnesium therapy.
Magnesium should be regarded as a cardiovascular drug, first and foremost, with
calcium antagonistic and antiadrenergic properties that may be accompanied by
minimal myocardial depression.[40]
30
Magnesium: 30–50 mg/kg,
•
•
•
•
•
•
•
•
– followed by 7–15 mg/kg/h IV
– In the Peripheral Nervous System it interferes with the release of neurotransmitters
at all synaptic junctions & potentiates the action of local anesthetics(3)
Peripheral nervous system: interferes with the release of neurotransmitters at all synaptic
junctions & potentiates the action of local anesthetics.[40]
At the neuromuscular junction, magnesium concentrations of 5 mmol/L cause significant
presynaptic neuromuscular blockade and enhance the action of the nondepolarizing muscle
relaxants.[40]
It can precipitate severe muscle weakness in patients with Eaton-Lambert syndrome, patients
with myasthenia gravis, or patients pretreated with a small dose of a defasciculating agent.[40]
Magnesium prolongs the action of depolarizing neuromuscular blocker drugs (e.g.,
succinylcholine); administration before the use of succinylcholine prevents the release of
potassium provoked by the neuromuscular blocking drug (see Chapter 29).
Magnesium has several important pharmacologic actions.
Its route of elimination is renal, and any patient who is oliguric or in a reduced urine
output state requires downward dosing adjustment of magnesium therapy.
Magnesium should be regarded as a cardiovascular drug, first and foremost, with
calcium antagonistic and antiadrenergic properties that may be accompanied by
minimal myocardial depression.[40]
Calcitonin
Calcitonin is a 32 amino acid peptide hormone that regulates calcium homeostasis in
vertebrates. It also has analgesic properties, primarily through receptor-mediated modulation of
serotonergic activity in pain pathways of the central nervous system. Salmon calcitonin synthetic
form has greater potency
The adverse effects of calcitonin therapy such as
sedation, nausea, skin flushing and diarrhoea may reflect increased serotonergic activity. In
rodents, the 5HT3 antagonist tropisetron reduced its analgesic efficacy, which may be relevant in
humans during the treatment of nausea and vomiting (Visser, 2005). Salmon calcitonin, (IV, SC,
IM, IN or rectal) reduces acute pain at rest and on movement and improves mobilisation (in 7 to 28
days) in patients with osteoporotic vertebral fractures and side effects are usually minor and
mainly gastrointestinal (Blau & Hoehns, 2003 Level I; Knopp et al, 2005 Level I).
IV (and likely SC) salmon calcitonin is effective in the treatment of acute phantom limb pain
(Jaeger & Maier, 1992 Level II). However, it was not effective for chronic phantom limb pain
(Eichenberger et al, 2008 Level II).
Bisphosphonates
IV pamidronate (3 daily doses) reduced pain associated with acute osteoporotic vertebral fractures
for up to 30 days post-treatment (Armingeat et al, 2006 Level II).
Bisphosphonates reduced sub-acute bone pain associated with metastatic carcinoma of the breast
(Pavlakis et al, 2005 Level I) or prostate (Yuen et al, 2006 Level I) and in multiple myeloma
(Djulbegovic et al, 2002 Level I).
Salmon calcitonin and bisphosphonates ANZCA’s Key messages
31
1. Bisphosphonates reduce bone pain associated with metastatic cancer and multiple myeloma
(N) (Level I [Cochrane Review]).
2. Salmon calcitonin reduces pain and improves mobilisation after osteoporosis-related vertebral
fractures (S) (Level I).
3. Salmon calcitonin reduces acute but not chronic phantom limb pain (N) (Level II).
4. Pamidronate reduces pain associated with acute osteoporotic vertebral fractures (N) (Level II).
Cannabinoids Key message
1. Current evidence does not support the use of cannabinoids in acute pain management
(S) but these drugs appear to be mildly effective when used in the treatment of chronic
neuropathic pain, including multiple sclerosis-related pain (N) (Level I).
Neuraxial Analgesia: Epidural Analgesia
Superior to systemic opioids; Efficacy determined by:Catheter-incision site congruency;Choice of
analgesic drugs; LA+Opioid;Rates of infusion;Duration of epidural analgesia; At least 2-4 days;
Type of pain assessment:Dynamic Vs Rest
Peripheral Regional Analgesia
Pain control superior to systemic opioids; Fewer side effects compared to systemic opioids; Fewer
neurologic and infectious complications compared to neuraxial block; Prolonged duration; Single
injection and continuous catheter techniques
Indications of peripheral Nerve Blocks:
Pain control superior to systemic opioids; Fewer side effects compared to systemic opioids; Fewer
neurologic and infectious complications compared to neuraxial block; Prolonged duration; Single
injection and continuous catheter techniques
Peripheral Nerve Block
Indication: Lumbar plexus; Surgery of knee; Femoral Nerve; TKA, ACL repair, femoral neck
fracture, saphenous vein stripping, muscle biopsy of anterior, medial or lateral thigh; Sciatic Nerve;
AK amputation (combined with lumbar plexus block
Ankle replacement, arthrodesis; Calcaneal osteotomy; Achilles tendon repair; Popliteal Fossa; BK
amputation (combined with saphenous nerve block); Ankle surgery: Triple arthrodesis, Achilles
tendon repair; Foot surgery: Bunion surgery, transmetatarsal amputation
Paravertebral Block: Suited for thoracic, breast surgery, VATS, cholecystectomy, nephrectomy
etc
Used to treat rib fracture pain; Potential space, contains anterior and posterior ramus of the spinal
nerve root with white and grey rami communicantes; Single injection or continuous catheter
technique; Comparable to thoracic epidural blockade
No hypotension, PONV, urinary retention
Other Techniques: Rectus Sheath Block; Transversus abdominis plane block; Placement of
continuous wound catheter
Continuous intra-articular infusion of LA; Periarticular soft tissue injection of LA; Intrapleural or
Intraperitoneal Analgesia
32
Complications: Intravascular injection (lIntralipid); Unintentional neuraxial spread; Scalene block;
Lumbar plexus block
Paravertebral block; Nerve Damage; Incidence 1:10000 – 1:30000; Significant nerve
damage 1:1 00 000
Direct injury, hematoma, infection, ischemia; >90% recover within 1 week; 92 -97% within 46 weeks, 99% within 1 year
Definition: Any technique of pain management that allows the patients to manage their own
analgesia on demand
Compensates for interpatient and intrapatient variability in analgesic needs, variability of serum
drug levels, administrative delays
Local anaesthetics
• Local anaesthetic agents produce reversible conduction blockade of impulses along central
and peripheral nerve pathways by altering membrane permeability to sodium ions.
• Preferentially block smaller diameter nerve fibres.
– C fibre
– A delta and Sympathetics
– A beta - touch and pressure
– A alpha- motor function of skeletal muscles
• To prevent conduction 3 nodes in succession must be blocked.
Long acting Local Anaesthetic Agents (Amide Group)
• Bupivacaine (Marcaine) S/P small cardiotoxic window
• Ropivacaine (Naropin)
• Levobupivacine (Chirocaine)
• Short acting LA: Lignocaine
Amide group
Ropivacaine :pure S (-) enantiomer :low lipid solubility
•
Toxicity CVS and CNS occurs at plasma levels greater than 4 mcg/kg.
Chirocaine (Levobupivacaine): High Lipid solubility
Toxicity CVS and CNS occurs at plasma levels greater than 2 – 3 mcg/kg
Bupivacaine: racemic mixture; high lipid solubility
Toxicity: CVS and CNS occurs at plasma levels greater than 1.5 – 2 mcg/kg
Side effects of Local Anaesthetics
• Hypotension due to peripheral vasodilatation
• Motor blockade
• CNS toxicity - tingling of lips, tinnitus, nystagmus, convulse.
• CVS toxicity - bradycardia, heart block, cardiac arrest.
• .
References:
Australian Medicines Handbook Pty Ltd. Last modified by AMH: July 2011.
MIM’s online 2010
Oxford Medicine online data base Anesthetics, 2010
\ Systemic Medications: Opioids
Opioid Receptors: ì, κ and δ receptors
Location of receptors:
Periphery following inflammation
Spinal cord dorsal horn
Supraspinally in the brainstem, thalamus and cortex
33
PAG, nucleus raphe magnus and RVM in descending pathway
Mechanism of Action:
Spinal
Inhibition of Ca++ influx presynaptically
Enhacing K+ efflux postsynaptically
Activation of descending inhibitory GABAergic circuit
Peripheral
Inhibition of release of pro inflammatory and pro nociceptive substances
Adverse Effects & Problems:
Respiratory Depression
Nausea and Vomiting
Sedation
Urinary Retention
Euphoria/Dysphoria
Constipation
Tolerance
Dependence and Addiction
Transdermal Fentanyl Delivery System (Ionsys)
Needle free, patient activated system for
in-hospital use
Iontophoresis
Low intensity electrical field
used to transport fentanyl
across skin into circulation
Each double click delivers 40mcg over 10
min
For us in adults > 18 years
Used for 24 hours or 80 doses
Pethidine:
Phenylpiperidine derivative μ and κ receptor
agonist.
34
+
Also has Na channel blocking and Atopinergic
action
Routes
IM, IV, PO
Duration of Action
2-4 hours
Side effects
CNS excitation- seizures, myoclonus due to nor-pethidine
toxicity
Interaction with MAO inhibitors, antidepressants
Dose
100mg IV/IM q 4 hr
300 mg PO q 4 hr
Watch for
Nausea,vomiting, euphoria, ventillatory depression
sedation
Tramadol:
Moderate affinity ì receptor agonist.
Acts on spinal modulating pathways
Inhibition of neuronal NA and Serotonin uptake
Stimulation of presynaptic serotonin release
Adverse Effects:
Nausea & Vomiting
Ondansetron interferes with analgesic effect
Non addictive, less sedation
Dose: 3 mg/kg IM/IV/PO for moderate to severe pain
Buprenorphine:
Semisynthetic, Agonist-Antagonist
Routes of administration:
IV, IM, Neuraxial, SC, SL, Trasdermal
Useful in morphine intolerant patient
Ceiling effect for respiratory depression, but not for analgesia.
Antiflammatory action
Useful in intra-articular injections
Prolongs duration of analgesia in peripheral nerve blocks with LA
Methadone:
Synthetic broad spectrum opioid
Mu receptor agonist
NMDA antagonist
Inhibitor of monoamine transmitters
Useful in treatment of neuropathic pain
Orally well absorbed
No dose adjustment in renal disease
Drug most commonly used for opioid rotation
35
NSAIDs
Mechanism of Action
Inhibition of Cyclo-oxygenase enzymes (type 1 & 2)
Reduce concentrations of PGE2 :
Sensitise peripheral nociceptors to histamine and bradykinin
Centally Increase Substance P and Glutamate Increase sensitivity of second order neurons Decrease
NTs from descending pathway
Benefits:
• Opioid Sparing
• Reduced incidence of opioid side effects
• Anti-inflammatory effects
Adverse Effects:
• Platelet Dysfunction
• Gastrointestinal Ulceration
• Nephrotoxicity
• Impaired bone healing
• Hypersensitivity
α2 Adrenergic Agonists
Primarily preoperative and intraoperative use
Clonidine:
• α2 agonist, α2: α1 biding 220:1
• PO, IV, TD, Neuraxial routs
• Reduced postoperative opioid requirement
• SE: Sedation, Bradycardia, hypotension
Dexmedetomedine:
• Superselective α2 agonist: α2:α1 binding 1620:1
• Supraspinal, Spinal & Peripheral action
• No respiratory depression
NMDA Antagonists
Ketamine:
NMDA receptor antagonism theoretically reduces central sensitisation, hyperalgesia and opioid
tolreance
Currently role in postoperative pain relief is uncertain
Insignificant difference in pain
Clinically insignificant opioid sparing
Psychomimetic side effects – hallucination, nighmares
Neuraxial Analgesia: Epidural Analgesia
Superior to systemic opioids
Efficacy determined by
Catheter-incision site congruency
Choice of analgesic drugs
LA+Opioid
36
Rates of infusion
Duration of epidural analgesia
At least 2-4 days
Type of pain assessment
Dynamic Vs Rest
Recommended catheter insertion sites
Location of incision
Examples of surgical procedure
Congruent
epidural
placement
Thoracic
Lung reduction, Radical mastectomy
Toracotomy, thymectomy
T4-T8
Upper Abdominal
Cholycystectomy, esophagectomy, gastrectomy,
hepatic resection, whipple’s
T6-8
Middle Abdominal
Cystoprostatectomy, nephrectomy
T7-T10
Lower Abdominal
AAA repair, Colectomy, TAH, Radical prostatectomy
T8-T11
Lower Extremity
Femoral-Popliteal bypass, THR, TKR
L1-L4
Local Anaesthetics comparison Opioids:
Local Anaesthetics
Act on spinal nerve roots,dorsal root ganglion or spinalcord itself.
High incidence of motor block
Hypotension
Sign
Significant failure rate due to regression and inadequate analgesia
Opioids:
Site of action:Lipophilic: systemicHydrophilic: spinal
Cathetre-Site congruencynot essential
No motor blockade
No hypotension
Analgesia superior to systemic opioids
Differences between lipophilic and hydrophilic
opioids
Property
Lipophilic Opioids
Hydrophilic Opioids
Common Drugs
Fentayl, Sufentanyl
Morphine, Hydromorphone
Onset of
analgesia
Rapid (5-10 min)
Delayed (30-60min)
Duration of
analgesia
Shorter (2-4 Hrs)
Longer (6-24 hrs)
CSF Spread
Minimal
Extensive
37
Site of action
Spinal ± Systemic
Spinal
Side Effects
Lower nausea and vomiting, pruritus
Early respiratory depression
Nausea & vomiting, pruritus
Early (<6 Hr) and Delayed (> 6 Hr)
respiratory depression
Local Anaesthetic-Opioid Combinations
Additive Effect
Superior analgesia, including dynamic pain relief
Limits regression of sensory blockade
Decreased LA dose requirement
Analgesia superior to IV PCA with opioids
Adjuvants:
Clonidine: 5-20 μg/Hr Dose dependent hypotension, bradycardia
Epinephrine conc. Of 2.5 μg/ml
Ketamine Theoretically useful in attenuating central sensitisation
Hypotension
0.7 – 3 % with epidural LAs
Epidural Analgesia: Adverse Effects
Motor Block
2 – 3 % with epidural LAs
More with cathetre-incision incongruence
Resolves within 2 hours of stopping infusion
If persistant, think of Spinal hematoma/abscess, cathetre migration
Nausea &
vomiting
20 – 50 % with single dose neuraxial opioid
45 – 80 % with continuous opioid infusion
Dose depdndent. Due to cephalad migration
Less with fentanyl than morphine
Treated with Naloxone, Ondansetrone, Droperidol, Metoclopramide, Dexamethasone
Pruritus
60% with Opioids; 15-18 % with LAs
Due to cephalad migration and activation of trigeminal nucleus. ?? Itch centre
Treated with Naloxone, Droperidol
Respiratory
Depression
Incidence 0.1 – 0.9 % with opioids
Equivalent to systemic administration of opioid
Early < 6 hr, Delayed > 6 hr
Delayed depression with Morphine. Due to cephalad spread
Risk Factors: Increasing dose, increasing age, concomitant sedatives, prolonged and extensive
surgery, thoracic surgery
Treatment: Naloxone 0.5 – 5 μg/kg/hr
Urinary
Retention
Higher than with systemic opioids
10 – 30% with epidural Las
Higher with higher infusion rates of LA
Benefits: (LA based epidurals)
Better attenuation of stress response to surgery
Earlier return of GI function without contributing to bowel dehiscence
Decreased postoperative pulmonary complications
38
Decreased incidence of postop MI with thoracic epidural
Better postop analgesia
Risks:
Higher incidence of spinal hematoma with LMWHs
Infections: Meningitis, Spinal Abscess (1/10000 with catheter < 4 days)
Superficial cellulitis: 4-14 %
Catheter migration: Intrathecal, Intravascular, subcutaneous
Drug
Dosing
Comments
Clonidine
15-45 μg
Improves quality of blockade
Epinephrine
0.1-0.6 mg
Prolongs motor block & urinary retention
Neostigmine
6.5 – 50 μg
Motor blockade
Nausea & vomiting
Opioid
Dose
Fentanyl
5-25 μg
Sufentanyl
2-10 μg
Morphine
0.1-0.3 mg
Diamorphine
1-2 mg
Pethidine
10-30 mg
Peripheral Regional Analgesia
Pain control superior to systemic opioids
Fewer side effects compared to systemic opioids
Fewer neurologic and infectious complications compared to neuraxial block
Prolonged duration
Single injection and continuous catheter techniques
Indications of peripheral Nerve Blocks
Pain control superior
to systemic opioids
Fewer side effects
compared to systemic
opioids
Fewer neurologic and
infectious
complications
compared to neuraxial
Pain control superior to systemic opioids
Fewer side effects compared to systemic opioids
Fewer neurologic and infectious complications compared to neuraxial block
Prolonged duration
Single injection and continuous catheter techniques
39
block
Prolonged duration
Single injection and
continuous catheter
techniques
Pain control superior to
systemic opioids
Fewer side effects
compared to systemic
opioids
Fewer neurologic and
infectious complications
compared to neuraxial
block
Prolonged duration
Single injection and
continuous catheter
techniques
Pain control superior to systemic opioids
Fewer side effects compared to systemic opioids
Fewer neurologic and infectious complications compared to neuraxial block
Prolonged duration
Single injection and continuous catheter techniques
Peripheral Nerve Block
Indication
Lumbar plexus
Surgery of knee
Femoral Nerve
TKA, ACL repair, femoral neck fracture, saphenous vein stripping, muscle biopsy of anterior, medi
thigh
Sciatic Nerve
AK amputation (combined with lumbar plexus block
Ankle replacement, arthrodesis
Calcaneal osteotomy
Achilles tendon repair
Popliteal Fossa
BK amputation (combined with saphenous nerve block)
Ankle surgery: Triple arthrodesis, Achilles tendon repair
Foot surgery: Bunion surgery, Transmetatarsal amputation
Paravertebral Block:
Suited for thoracic, breast surgery, VATS, cholecystectomy, nephrectomy etc
Used to treat rib fracture pain
Potential space, contains anterior and posterior ramus of the spinal nerve root with white and
grey rami communicantes
Single injection or continuous catheter technique
Comparable to thoracic epidural blockade
No hypotension, PONV, urinary retention
Other Techniques:
Rectus Sheath Block
Transversus abdominis plane block
Placement of continuous wound catheter
Continuous intra-articular infusion of LA
Periarticular soft tissue injection of LA
Intrapleural or Intraperitoneal Analgesia
40
Complications:
Intravascular injection
Unintentional neuraxial spread
Scalene block
Lumbar plexus block
Paravertebral block
Nerve Damage
Incidence 1:10000 – 1:30000
Significant nerve damage 1:1 00 000
Direct injury, hematoma, infection, ischemia
>90% recover within 1 week
92 -97% within 4-6 weeks, 99% within 1 year
Slide (28) 32 So what does pain management look like at BHS
The follow
•
•
•
Are statistics from our APS & Operational statistics
Our PACU APP
And a discussion of the drugs, & how they’re used currently @ BHS & those around the
corner
Slide (29) 33 BHS Statistics
Slide (30) 34 Some Innovation in care
Different ways of administering L.A.
Adjunctive therapies
Old drugs used differently
– Gabapentin : Used pre operatively: Opioid sparing effect during the first 24 hours
after a single 300 to 1,200 mg dose of gabapentin, administered one to two hours
preoperatively, ranged from 20 percent to 62 percent (2)
New: Adjunctives ie Capsaicin cream (used for centuries in the east)
Narcotics Different routes Topical
Old :Narcotic’s Buprenophine patch (<3D:7D/S/C Fat to metablosie Heat 25 - 50%
increase/pressure increase, 3 week site rotation
APP doing
New Targin: Oxycodone/Narloxone (10/5mg) oral
Tapentadol: Oxycodone/Noradrenaline oral
Slide (31) 35 APP BHS
Slide (32) 36 Some Adjunctives Pharmogolygt
Anticonvulsants: Gabapentin
•
Ideally if anticonvulsants are considered they are best admninstered preoperatively (6)
41
•
Gabapentin binds to the alpha-2 delta sub-unit of the presynaptic voltage gated-calcium
channels responsible for the inhibition of the calcium influx.(2)prevents release of
excitatory neurotransmitters in Pain Pathway
Pregablin is similar to gabapentin but has a superior pharmacokinetic profile its many potential actions
such as reducing opioid requirements, prevention & reduction of opioid tolerance, improvement
of the quality of opioid analgesia, decreased respiratory depression, relief of anxiety, and gastric
sparing make it an attractive drug to consider for control of pain in the post operative period
–
Slide (33) 37
Magnesium :30–50 mg/kg,
•
•
•
•
•
•
•
•
– followed by 7–15 mg/kg/h IV
– In the Peripheral Nervous System it interferes with the release of neurotransmitters
at all synaptic junctions & potentiates the action of local anesthetics(3)
Peripheral nervous system: interferes with the release of neurotransmitters at all synaptic
junctions & potentiates the action of local anesthetics.[40]
At the neuromuscular junction, magnesium concentrations of 5 mmol/L cause significant
presynaptic neuromuscular blockade and enhance the action of the nondepolarizing muscle
relaxants.[40]
It can precipitate severe muscle weakness in patients with Eaton-Lambert syndrome, patients
with myasthenia gravis, or patients pretreated with a small dose of a defasciculating agent.[40]
Magnesium prolongs the action of depolarizing neuromuscular blocker drugs (e.g.,
succinylcholine); administration before the use of succinylcholine prevents the release of
potassium provoked by the neuromuscular blocking drug (see Chapter 29).
Magnesium has several important pharmacologic actions.
Its route of elimination is renal, and any patient who is oliguric or in a reduced urine
output state requires downward dosing adjustment of magnesium therapy.
Magnesium should be regarded as a cardiovascular drug, first and foremost, with
calcium antagonistic and antiadrenergic properties that may be accompanied by
minimal myocardial depression.[40] (millers)
Slide (34) 38
NSAID’s Cox 2 :
Recent research indicates that, in addition to peripheral blockade of prostaglandin synthesis,
central inhibition of cyclooxygenase-2 may play an important role in modulating nociception.
Although nonspecific NSAIDs provide analgesic efficacy similar to coxibs, their use has been
limited in the perioperative setting because of platelet dysfunction and gastrointestinal toxicity.
Coxibs may be a safer alternative in that setting. Both coxibs and traditional NSAIDs may
contribute to a dose-dependent increase in cardiovascular toxicity and impaired osteogenesis
benefits of coxibs include improved quality of analgesia; reduced incidence of GI side effects & no
platelet inhibition (note Cox 1 & 2: Ketorolac )
Paracetamol
Is antipyretic & analgesic but has little, if any, anti-inflammatory action.
Its analgesic action is believed to be inhibit COX-3. At the spinal cord level, it also antagonize
neurotransmission by NMDA, substance P, and nitric oxide pathways IV 100 ml: 10 mg/ml @
15/60min; Onset of action <5 -10/60, peak at 1- 2hrs (6hrly order)
42
Slide (35) 39
Central alpha2 agonist Clonidine: Its sedative, pro-anesthetic, and pro-analgesic effects ability
to blunt the central sympathetic response by as yet unknown mechanism(s). It also minimizes
opioid-induced muscle rigidity, lessens postoperative shivering, causes minimal respiratory
depression, and has hemodynamic stabilizing effects(2)
Slide (36) 40
L.A. Some innovations in care
Different ways of administering: Intavenous LA: acts a membrane stabilizer (reversibly block the
Na channels of the lipid membranes & prevent sudden influx of sodium ions into the axon,
blocking depolarization & the action potential. (2009 Mosby: Marx: Rosen’s emergency medicine)
Increase Regional LA use: continuous or intermittent bolusing (new research suggest higher
efficacy than continuous infusion Epidural PCA & TAP; femoral; wound; elastomeric pump e.t.c
PAIN BUSTER device elastomeric pump. An elastomeric pump is a device that has a distensible
bulb inside a protective bulb with a built-in filling port, delivery tube, and bacterial filter LA and anti
inflammatory medication use
Acupuncture (2) perioperative acupuncture might be a useful adjunct for acute postoperative pain
management. However, there are issues with
applicability and generalizability of the procedure
Different ways of administering
R&D LA: basically two overarching approaches for prolongation of local anesthetic action. One is
the use of novel delivery techniques for existing drugs. In an endeavor to “make old drugs new”
[51], liposome or polymer encapsulation of local anesthetics are being formulated. The second
approach is the development of novel, extremely long-acting local anesthetics; road toward
achieving this goal may be long and winding, due to problems of these drug delivery systems,
such as shelf life,aggregation, leakage, and toxicity (2)
Slide (37) 41
New Narcotics preparations
Targin: Oxycodone/Narloxone (10/5mg)
Tapentadol: Narcotic (oxycondone/ tramadol):centrally acting analgesic; an agonist at μ-opioid
receptor & a norepinephrine reuptake inhibitor
18-fold affinity- μ opioid receptor compared to morphine;
2 -3 less potent than morphine improved
G/I tolerability compared to classical opioids.
Dose unchanged in renal impairment. No Hepatoxicity IR oral: 50, 75 & 100 mg 4-6/24 <daily
dose 600-700 mg
Contraindicated: severe bronchial asthma, paralytic ileus,pt’s on (MAOI): SSRI’s, selective
norepinephrine reuptake inhibitor SNRI, tryptans or, tricyclic antidepressants
Side effect: Serotonin syndrome include:mental status changes such as hallucinations, coma,
autonomic instability such as tachycardia, hyperthermia, and neuromuscular abnormalities such as
hyperreflexia and incoordination.
.Slide (38) 42
Narcotics used topically
•
Different routes Topical
– Old :Narcotic’s Buprenorphine /fentanyl patch
43
Slide (39) 43
New Adjunctive drugs
Capsaicin (8-methyl-N-vanillyl-6-nonenamide) acts as a TRPV-1 agonist TRPV1 receptor markedly
reduced in inflammatory conditions & is present on unmyelinated C fiber endings in the periphery.
Activation of the TRPV receptors releases high intensity impulses & releases substance P, which results in
the initial phase of burning. Continued release of substance P in the presence of capsaicin leads to the
depletion of capsaicin and a subsequent decrease in C fiber activation.
Slide (40) 44 Latest research Adjunctive not seen in action
Neostigmine (2,4), & recently, adenosine
Neostigmine, a cholinesterase inhibitor, has been reported to possess analgesic properties when
doses of 10–200 g were administered in the subarachnoid (not seen used)
or epidural spaces epidurally administered neostigmine(1 g/kg) produced more than 5 h of pain
relief after knee surgery (249). Neostigmine (10 g/kg) also enhanced epidural local analgesia (4)
Drugs on the horizon:Prialt,(ziconotide) IT only non opioid (used Uk & USA),
IT only non opioid (used Uk & USA),
Prialt,(ziconotide) (used in UK/ USA 2007), Rx pain associated with cancer, AIDS and
neuropathies. Based on a compound found in the poison of the South Pacific cone snail, it controls
pain in a new way -- by blocking the calcium channels in nerve cells that transmit pain signals -- &
may have broad implications for the future of pain management. Benefits; Non narcotic +/- 1000
stronger than morphine, non addictive Side Effects: ONLY Intrathecal high risk of side effecting,
hallucinations and even psychosis in vulnerable people.
Slide (41 45 Advances In Organisational Aspects Of Post operative Pain Control
–
–
–
–
–
Surgery Type i.e.Laparoscopic surgery, anterior hip replacement
Pre/interoperatively maximized use of L.A. & NMDA receptor antagonists agents
CBT pre hospitalization education
Early rehabilitation
Use of alternative therapies i.e. Acupuncture, meditation, mindfulness
concepts(although presently not strongly supported – research occurring in this area)
Slide (42) 46 Just to mention any thing not already mentioned in summary
44
45