PainConference-AddictionandPain
Addiction & Pain
What is addiction?
• Compulsive use despite harm
Addiction
• 1° chronic neurobiological disease
• Development & manifestations influenced by:
– Genetic
• Drug disposition
• Stress responsivity
– Environmental
• Drug-induced neurochemical changes
– Psychosocial
• Psychopathology
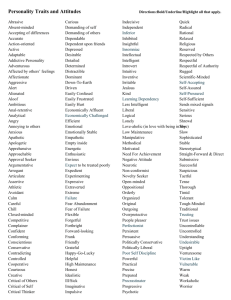
• Personality traits
Anatomic Pathways
• Mesocorticolimbic : pleasure, reward, motivation
– Prefrontal cortex
• Memory, emotnal processing, impulse control, decisn making
– Ventral pallidum
• Craving, seeking, relapse
– Basolateral amygdala
• Associative learning, emotional memory
– Ventral tegmental area
• Reinforcement, reward = priming circuit
– Nucleus accumbens
• PFC NAc VP = motor memory circuit
Neurotransmitters
• NAd
• 5OH-T
• ACh
• Glutamate
• GABA
• Enkephalins
• Cannabinoids
Principles of Opioid Management
• Have a clear diagnosis
• Identify/manage pyschiatric illness
• Identify/manage psychological distress
• Long acting opioids only
• Limited supply
• Frequent visits
• Regular monitoring (blood, urine)
• Emphasis on wellness & behavioural change
U.D.T.
• Purpose – check compliance, other meds
• Use prophylactically, nonpunitively, randomly
• Philosophical opposition = problem
• Basic panel
• Drug not there – testing issue or diversion
• Is sample own, fresh, human?
The Spectrum
• Recreational users
• Chemical copers
• Substance abusers
• Addicted
‘Wanting More’
• Tolerance
• O.I.H.
• Pseudoaddiction
• Disease progression
• Withdrawal
• Aberrant behaviour
• Diversion
Opioid Withdrawal
• = the cost of opioid dependence
– Anxiety, insomnia, irritability, restlessness
– Nausea & vomiting, abdominal cramping
– Myalgias, arthralgias, bone pain
– Tremor, myoclonic jerks
Pseudoaddiction
• ‘Drug-seeking’ 2° to inadequate analgesia
• Reassess
– Diagnosis
– Drug
– Dogma
Recognising the Drug Seeker
• Time
• Patience
• Awareness
• Monitoring
• Sense of humour
Recognising the Drug Seeker
• History
– Forging/altering/losing/hoarding prescriptions
– Doctor shopping
– Stealing/borrowing
– Unsanctioned escalation
– Injecting oral preparations
– Using polysubstances
– Preoccupation with opioids
– Insistence on certain forms/routes
Recognising the Drug Seeker
• Examination
– Intoxicated/withdrawing
– Poor habitus/hygiene (bumble bee teeth)
– Track marks
– Cellulitis/abscess
– Injuries from falls
– Abnormal illness behaviour
– Pupils
– LOC
Triaging Management
• Level 1 = 1° care
– No past / current hx of concern
– Environment safe
• Level 2 = shared care
– Past hx substance abuse
– Environment potentially unsafe
– Past / current hx psychiatric disorder
• Level 3 – specialist care
– Current substance abuse
– Psychopathology