Identification of Enterobacter aerogenes by Different Microbiological
advertisement
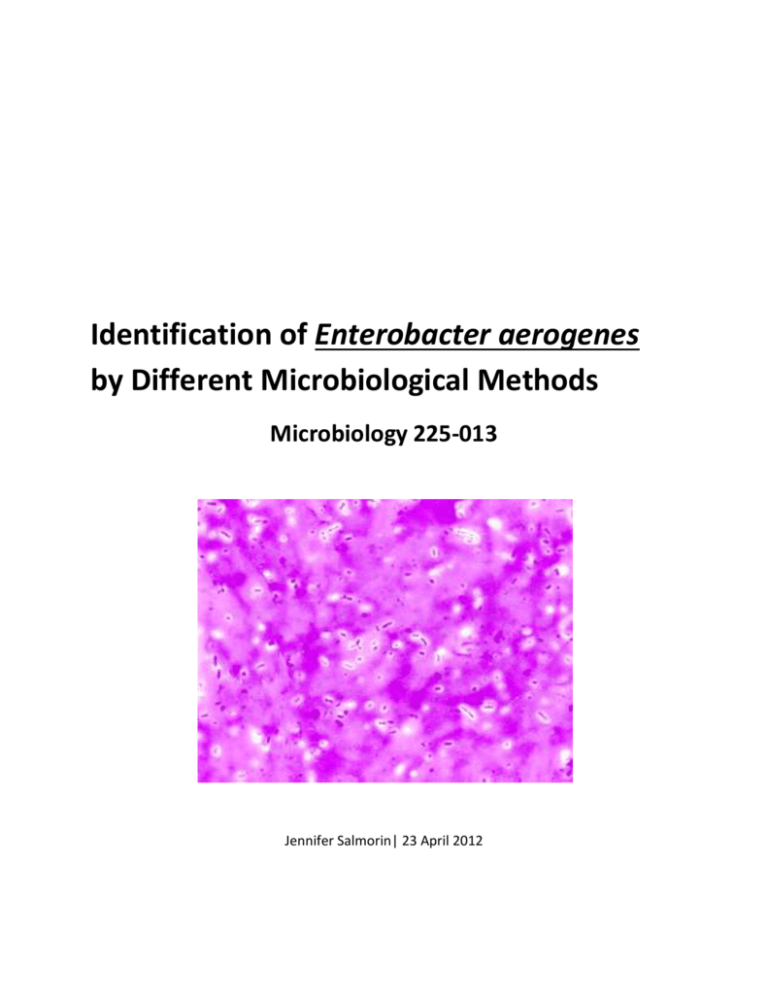
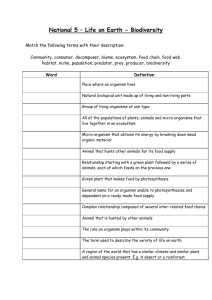
Identification of Enterobacter aerogenes by Different Microbiological Methods Microbiology 225-013 Jennifer Salmorin| 23 April 2012 Title: Identification of Enterobacter aerogenes by Different Microbiological Methods Abstract: Given an “unknown” culture in a TSA agar slant, the class objective was to identify the unknown organism by using various laboratory procedures and experiments that would assist in arriving at an educated conclusion regarding the Genus species. The first procedure involved preparing a Gram’s stain to identify if the organism was gram positive or negative and determine the cell morphology. After examining the stained organism under the microscope under the oil immersion lens (100X), the organism’s cell shape could be identified as gram positive or negative. The organism was identified as a gram negative, based on its red stain, and bacilli, based on the rod shape. A streak plate was also prepared by inoculation and incubation to display the colony pattern of the organism. After identification of the gram negative bacilli, the lactose fermentation test was performed to determine the bacteria’s ability to ferment lactose. After inoculation and incubation of the lactose broth, the organism was determined to be lactose positive due to its yellow coloring after the addition of a phenol red indicator. Once this test was complete, and the result identified, the indole and H2S test was performed simultaneously to determine the organism’s ability to produce indole and reduce sulfur into H2S, respectively. A SIM deep was inoculated with the organism and incubated for 48 hours. After incubation, a Kovac’s reagent was added to the SIM deep, and a negative result was found for both tests (yellow for indole test and no black precipitate present for H2S test). After this result was determined, and the organism narrowed down to two, a final methyl red test was performed to test for the acid end products from glucose fermentation and to ultimately identify the organism. A glucose broth was inoculated with the organism and 48 hours after incubation, a methyl red indicator was added to determine the identity of the Genus species. The test result was negative due to the yellow coloring of the broth after the addition of a methyl red indicator. The Genus species was therefore identified as an Enterobacter aerogenes. Introduction The Enterobacter aerogenes are most commonly identified as hospital acquired infections, also known as nosocomial infections. This gram negative bacteria is a rod shaped (bacilli) and exists in soil, water, dairy products, as well as resides in the natural flora in the gastrointestinal tract of animals and humans alike (2). 2 Below is a view of the bacteria under a microscope using a Gram’s stain (2): The majority of these infections are attributed to accidental transfer of bacteria to the patient during surgery or transfer of infection through urethral catheters. They are opportunistic pathogens that infect patients with compromised immune systems (2). They are responsible for various infections that include bacteremia, lower respiratory tract infections, skin and softtissue infections, urinary tract infections, endocarditis, intra-abdominal infections, and more (1). Fifty percent of septicemia and seventy percent of urinary and intestinal infections are caused by these bacteria. A major characteristic of these bacteria is that they are extremely resistant to β-Lactam antibiotics, fluroquinolones, chloramphenicol, tetracycline, and kanamycin; this is due to the mutations that encode porins and membrane efflux pumps that pump out the antibiotics before they have a chance to destroy the bacteria (2 and 3). The resistance of these bacteria to antibiotics and other drugs has lead to outbreaks of infections in intensive care units in Belgium, France, Austria, and the United States (2). There are several ways to avoid the infection of Enterobacter aerogenes. Many of these methods are left up to healthcare providers caring for patients in a hospital setting. One way is to assure that all instruments used during surgical procedures are sterile. Another way to reduce the spread of these bacteria is removing catheters and venous needles and tubing and placing them in new locations (2). Avoiding third generation cephlasporins is also crucial because resistant strains can produce (1). 3 Materials and Methods Gram Staining Materials (5): Inoculating loop, glass slides, Bunsen burner, Distilled water. Crystal Violet (Hucker’s) — Solution A of crystal violet (90% dye content) was made by dissolving 2.0 g of crystal violet in 20 ml of 95% ethyl alcohol. The solution B was made of 0.8g Ammonium oxalate in 80 ml of distilled water and finally the solution A and B was mixed together. Gram’s Iodine — Iodine 1.0g, Potassium iodide 2.0g was dissolved in 300 ml of distilled water. 95% Ethyl alcohol — Ethyl alcohol (100%) 95.0 ml and 5 ml of distilled water. Safranin — Safranin O 0.25 ml, Ethyl alcohol(95%) 10 ml and 100 ml of distilled water. The Gram’s reagents were aliquoted in small dispensing squeeze bottles for laboratory use. Lactose Fermentation Test Materials (4): Lactose broth with phenol red (pH 7.3): Trypticase: Sucrose: Sodium Chloride: Phenol red: 10.0 g 5.0 g 5.0g 0.018 g The media was aliquoted in 5ml per test tube and autoclaved at 15 lbs pressure for the minimum of 15 minutes. Indole Production Test / Hydrogen Sulfide Test Materials: SIM Agar Deep (4): Peptone Beef extract Ferrous ammonium sulfate Sodium thiosulfate Agar 30.0 g 3.0 g 0.2 g .025 g 3.0 g 4 Kovac's reagent: (per liter) (6) p-Dimethylaminobenzaldehyde Amyl Alcohol Hydrochloric acid 50.0g 750.0 ml 250.0 ml Other Materials (8): Bunsen burner, inoculating needle, test tube rack and glassware marking pencil Methyl Red Test Materials: MR-VP Broth (3): Peptone Dextrose Potassium phosphate 7.0 g 5.0 5.0 g Methyl Red Indicator (9): Methyl Red .10 g Ethanol, 95% 300 mL Distilled water to make 500mL Other Materials (8): Bunsen burner, inoculating loop, test tubes, and glassware marking pencil Experiments An agar slant containing an unknown organism with an associated number, 9, was received in the lab. Flow charts were distributed to track the experiments performed for the organism. Gram’s Staining: A differential staining technique called Gram’s staining was performed to identify whether the bacterial cells were gram positive or negative, as well as to determine the shape of the cells. First, a smear of the organism was made on a clean glass slide by aseptic technique. This technique involved placing a drop of distilled water onto a slide and then transferring the 5 organism onto the glass with a sterile inoculating loop. The smear was air-dried and then heat fixed by quickly passing through the Bunsen burner flame. The smear was flooded with crystal violet for one minute. After a minute was up, the crystal violet was washed off with tap water. Next, the smear was thoroughly rinsed with Gram’s iodine mordant for one minute and then the Gram’s iodine was washed off with tap water. The slide was then gently decolorized with 95% ethyl alcohol by slowly dripping the alcohol onto the slide until it ran mostly clear. Once again, the slide was washed with tap water. The slide was then counterstained with safranin for 45 seconds and then washed with tap water. The slide was blotted dry with bibulous paper and examined under oil immersion under the microscope (10). Microscope Observation: After completion of the Gram’s stain procedure, the slide was observed under an Olympus CX21/31 binocular microscope under the oil immersion objective (100X) to determine whether the organism was gram positive or gram negative, as well as to identify the cell’s shape and morphology. Lactose Test: A lactose broth was inoculated with the organism using aseptic techniques and incubated at 37 degrees Celsius for 36 to 48 hours. After 48 hours, a phenol red indicator was added to the broth and the culture was examined for lactose fermentation (11). MacConkey (MAC) Agar Plate and Trypticase Soy Agar (TSA) Plate Streak: The unknown organism was streaked with an inoculating loop using aseptic techniques to show colonization in both a MAC plate as well as a TSA plate. After the first streak in the upper quadrant of both the TSA and MAC plates was made, the plate was rotated 90 degrees and streaked again once the loop was re-flamed. It was then rotated another 90 degrees and streaked again after re-flaming the loop. It was rotated another 90 degrees and streaked for a final time (12). Indole/ Hydrogen Sulfide Test: The indole and hydrogen sulfide tests were able to be performed simultaneously. A SIM deep agar was stabbed with an inoculating needle containing the organism using aseptic technique. The tube was incubated for 48 hours at 37 degrees Celsius. After 48 hours of incubation, the tube was removed and ten drops of Kovac’s reagent was added to the culture. It was examined for color change at the top of the culture for indole production (13). It was also examined for black coloration along the stab line to determine if it was motile and if it had any H2S production (14). 6 Methyl Red Test: An MR-VP broth was inoculated with the organism using aseptic technique. The tube was incubated for 48 hours at 37 degrees Celsius. Five drops of methyl red indicator was added to the culture and the color was examined for glucose fermentation (13). Results and Discussion/Conclusion The Gram’s stained slide displayed pinkish-red stubby rods when observed under the oil immersion lens (100X) of the microscope. This microscopic observation indicated that the organism was a gram negative bacilli (4). Following the Gram Negative Bacilli flowchart, a lactose test was performed next. After performing the lactose test, a phenol red indicator was added, and it was determined that the organism was negative for lactose fermentation due to the red coloring (or no change in color) (11). Next, the indole and hydrogen sulfide production tests were performed simultaneously in the same tube. After 48 hours of incubation, ten drops of Kovac’s reagent was added to the culture. It was examined for color change at the top of the culture (where the Kovac’s reagent was added) for indole production (13). After the addition of the Kovac’s reagent, the coloring remained yellow (no color change occurred). This indicated that the substrate tryptophan was not hydrolyzed and tested negative for indole production. The same tube was also examined for black coloration along the stab line to determine if it was motile and if it had any H2S production. The absence of black coloration indicated that the organism was non-motile and that no sulfur was reduced into hydrogen sulfide (H2S), resulting in a negative reaction (14). Finally, a methyl red test was performed to identify the presence or absence of glucose fermentation. After inoculation and incubation, a methyl red indicator was added and the culture turned from red to yellow, indicating a negative result for glucose fermentation (13). Once this test was completed and the results examined, it was determined that the unknown organism was Enterobacter aerogenes, according to the Gram Negative Bacilli flowchart. 7 References 1. Medscape.com. 2010. Medscape Reference: Drugs, Diseases & Procedures. 7 January 2010. <http://emedicine.medscape.com> 2. MicrobeWiki.edu. 2011. MicrobeWiki Kenyon College. 22 April 2011. <http://microbewiki.kenyon.edu> 3. ASM.com. 2004. Antimicrobial Agents and Chemotherapy: Successive Emergence of Enterobacter aerogenes Strains Resistant to Imipenem and Colistin in a Patient. 28 November 2004. <http://aac.asm.org> 4. Cappucino, J.G. and Sherman Natalie. ‘Appendix 3 of Microbiology: A Laboratory Manual’. Ninth Edition, Benjamin Cummings, 2011. 5. Cappucino, J.G. and Sherman Natalie. ‘Appendix 5 of Microbiology: A Laboratory Manual’. Ninth Edition, Benjamin Cummings, 2011. 6. Open Wet Ware.com. 2010. Enzyme Tests. 30 March 2010. <Openwetware.org> 7. Cappucino, J.G. and Sherman Natalie. ‘Appendix 5 of Microbiology: A Laboratory Manual’. Ninth Edition, Benjamin Cummings, 2011. 8. Cappucino, J.G. and Sherman Natalie. ‘Experiment 24 of Microbiology: A Laboratory Manual’. Ninth Edition, Benjamin Cummings, 2011. 9. FDA.gov. 2001. Bacterial Analytical Manual. January 2001. http://fda.gov 10. Cappucino, J.G. and Sherman Natalie. ‘Experiment 10 of Microbiology: A Laboratory Manual’. Ninth Edition, Benjamin Cummings, 2011. 11. Cappucino, J.G. and Sherman Natalie. ‘Experiment 22 of Microbiology: A Laboratory Manual’. Ninth Edition, Benjamin Cummings, 2011. 12. Cappucino, J.G. and Sherman Natalie. ‘Experiment 2 of Microbiology: A Laboratory Manual’. Ninth Edition, Benjamin Cummings, 2011. 13. Cappucino, J.G. and Sherman Natalie. ‘Experiment 24 of Microbiology: A Laboratory Manual’. Ninth Edition, Benjamin Cummings, 2011. 8 14. Cappucino, J.G. and Sherman Natalie. ‘Experiment 25 of Microbiology: A Laboratory Manual’. Ninth Edition, Benjamin Cummings, 2011. 15. Cappucino, J.G. and Sherman Natalie. ‘Experiment 4 of Microbiology: A Laboratory Manual’. Ninth Edition, Benjamin Cummings, 2011. 9