IPS Opioid Manual 1.06
advertisement

Indiana Pain Society Best Practices Opioid Prescribing Manual
for Chronic Intractable Non-malignant Pain v1.06
Philosophy – EBM, Diversion/SA overlap, Tight vs Loose control, Venue
and population adjustments
Infrastructure
Patient Selection
High Risk Patients (prior SA, benzos, illicits, COPD, sleep apnea, obesity)
Patient Monitoring- reports from family/police/friends/anonymous,
UDS, saliva, blood testing, pill counts, INSPECT, surrounding states, VA,
psych, watching ambulation
Specific medications
Dosing and dose escalation
Controlling your patient population
Side effect mitigation
Harm reduction: benzodiazepines, opioid hyperalgesia, sedation
Optimum withdrawal and tapering protocols
The violent and disruptive patient
INFRASTRUCTURE
KEY ELEMENTS:
*Everyone employed in the clinic knows the rules and enforces
them uniformly
*Patients are given a copy of the clinic rules in advance of any
prescribing
*Patients receive informed consent for opioids including risks and
benefits/alternatives before prescribing chronically
*After hour emergency treatment must be addressed in advance
*Ability to monitor patients with INSPECT, drug screens, and pill
counts must be arranged before initiating prescribing.
*Follow-up intervals must be dosage and health appropriate but
should not exceed 2 months for schedule II controlled substances
COMMUNICATION
*Notifying current prescribers of opioids of your intent to provide
chronic prescribing and the opioid agreement with patient
*Notifying physicians of record of patient discharge for substance
abuse/diversion/hostility or conversion to non-narcotic therapies for
same
*Prominent notations made in your medical record in capital
letters when there is substance abuse/diversion, and placed in a readily
discoverable location in the record
PATIENT SELECTION
KEY ELEMENTS:
*INSPECT must always be queried prior to any initial prescribing.
For patients that claim to be receiving opioids currently from a
physician or provider, INSPECT must corroborate this prior to initial
prescribing.
*Prior records should be obtained directly from previous
prescribers listed in INSPECT for at least 6 months
*Substance abuse screening test should be obtained but with
recognition of its limited value
*Identifiable pathology noted whenever possible
*Extensive history obtained along with targeted physical exam
*Referral for PT/OT/specialists when appropriate
*Other methods of pain control that have been tried and failed
must be documented
*Opioids should not be the first medication tried for pain control
*Plan for prescribing (long term/short term) should be employed
with any practice limits noted (due to risk factors)
High Risk Patients
KEY ELEMENTS THAT MUST BE HANDLED:
*High Risk substance abuse/diversion- prior history of substance
abuse/diversion, illicit drug use history, alcohol abuse history, failed
UDS or substance abuse in other practices, admitted sharing of drugs
*High Risk overdose- Prior suicide attempts, prior overdose
history, severe COPD, morbid obesity, use of multiple sedating drugs at
night, use of asymmetric dosing of opioids at night, benzodiazepines>
tricyclic antidepressants or carisoprodol, daytime sedation, hepatic
dysfunction, high dose opioids, history of substance abuse (aberrant
dosing)
*High Risk disruptive to the medical practice- personality
disorders, hostile and belligerent nature of patient, carrying weapons
into the clinic, discusses past physical acts of violence without
prompting
Patient Monitoring
KEY ELEMENTS:
*Indiana INSPECT
*Toxicology monitoring (UDS, Saliva, Blood, Hair, GC/MS, LC/MS,
MS/MS, collection issues and doping, false negatives, false
Positives, cutoff value utility)
*Pill counts
*Office visit behavior
*Self reporting
*Police reports of DUI, illicit drug arrests, diversion arrests
*Non-identifiable source reports
*Family and friend reports
Specific Medications
Dosing and Dose Escalations
Controlling Your Population
*Pre-emptive control via patient selection/advertising/reputation
of the clinic/referral based practice
*Patient specific script writing
*Follow up intervals
*Action and reaction oriented practice
*Opioid agreements
*Opioid consent
*Pill counts
*Urine drug screening and interpretation
*Oral drug screening and interpretation
*Blood drug screening and interpretation
*Hair drug screening and interpretation
*INSPECT interpretation and limits
Side Effect Mitigation
*Anticipate constipation and prescribe for this with opioids
*Nausea
*Sedation
*Confusion
*Myoclonic events
*Edema
Harm Reduction
*Establishing dose limits for specific patients
*Establishing medication form for specific patients
*Taking charge of risks: polypharmacy and what the prescriber
can do about it
*Taking action when there is substance abuse or diversion
*Forbidden prescribing
Optimum Withdrawal and Tapering Periods
The Violent and Disruptive Patient
*Graded levels of response to diffuse and contain threat level
*Pre-defined protocol specific to the office/proximity to police, etc
*Security measures
I. PREFACE
Chronic pain affects nearly 100 million citizens in the US or approximately 1/3 of the population
according to the Institute of Medicine (2011). Chronic pain is defined as an unpleasant sensory
perception that persists longer than 3 months continuously. Frequently chronic pain exists for years
or for a lifetime. While the initiating event typically involves an acute pain event, chronic pain may
also develop spontaneously in the absence of a definable acute pain event. The pathophysiology of
acute and chronic pain are dissimilar. Acute pain involves a nociceptive insult typically involving an
inflammatory response that transmits pain along c and A-delta nerve fibers to the spinal cord where
the lateral spinothalamic tracts or bulbothalamic tracts carry the signal to the thalamus and
subsequently into other areas of the brain. There may be significant modification of the pain signal
along its pathway, and the signal is modified by environmental imprinting, culture, depression,
chronic anxiety, and emotion. Chronic pain occurs when there is a partial disconnect between the
initiating signal and the response, with pain perception continuing to exist long after the
inflammation or injury has healed. The signal modifications are more severe and may result in overt
amplification or lack of physiological inhibition of perceived pain. Furthermore, there may be loss of
discrimination between other pain signals and other sensory inputs. Touch, pressure, or
proprioception may be misinterpreted as pain by the spinal cord or brain resulting in allodynia and
hyperpathia. Functionally this produces an apparent hypersensitivity state where even mild nonpainful sensory input may be perceived as severe pain. Because of guarding, there is less activity and
loss of range of motion across many joints throughout the body, with subsequent muscle contracture,
and the production of severe muscle strain, enthesopathies, or tendonopathies when the patient
engages in an obligatory action in order to prevent falls or engages in any substantial increase in
physical activity. Such loss of activity may contribute to the development of other pathologies such
as obesity leading to hypertension, diabetes, and coronary artery disease, each further diminishing
activity. Osteoporosis may worsen due to diminished activity leading to fractures and anatomical
aberrations in posture and gait. Ultimately, the patients develop isolation from friends and family,
loss of job and reduction in social status, financial destruction, and ultimately may exist in a hell here
on earth. Some engage in suicide or suicide attempts. They seek cures from one healer after another,
exhaust their savings, and may lose their homes and families. Their misperception of chronic pain as
a simple nociceptive condition that is a mere extension of acute pain is unfortunately reinforced by
physicians that make the same error, and view chronic pain as an anatomical abnormality that
should be treated with surgery, injections, or physical therapy, frequently resulting in treatment
failure in reduction of the perception of pain or significant functional improvement. Patients are so
desperate that they will continue seeking more and more ill suited treatments. Opioids are
frequently prescribed as part of the treatment of chronic pain and may reflect one of the accepted
methods of treatment of chronic pain. They are prescribed by some well-meaning physicians and
prescribers, however opioids administered in the absence of sufficient patient or prescriber
education regarding the possible outcomes of opioid use including opioid induced hyperalgesia,
substance abuse, addiction, criminal behavior, overdose, and death, may be disastrous. In some
situations, opioid prescribing for chronic pain patients may become more of a problem than is
warranted by the beneficial effects of the treatment. Physicians and providers prescribing opioids to
chronic pain patients are frequently duped by those that are attempting to obtain these medications
for nefarious purposes and often have offices that are poorly equipped to appropriately monitor
these patients that require a significant degree of increased vigilance to prevent substance abuse and
diversion. Unlike other prescription medications, opioids are frequently shared drugs in our society
and result in a significant number of deaths in those without prescriptions for the medications, have
a substantial dollar value when sold on the street, and are intimately linked to criminal behavior and
a high rate of substance abuse. Prescribers of opioids may not want to engage in the messy issues of
discharging patients, arranging for addiction treatment, or confronting patients for aberrant use of
medications. All too often, these prescribers will perpetuate problem behavior of patients by
referring to one pain specialist after another when patients have engaged in substance abuse or
criminal diversion of medications. Physicians and providers prescribing opioids frequently lack the
training in appropriate use of long term opioid prescribing in chronic opioid maintenance therapy
(COMT), mistaking the acute pain relieving effects of opioids as directly transferrable to COMT.
The license to prescribe opioids does not necessarily in and of itself impart sufficient
knowledge or education to do so. The massive prescribing increase of opioids in the US over the past
decade has resulted in a very high death rate from opioid prescribing. Much of the prescribing is
injudicious prescribing for poorly defined reasons but also reflects insouciance of physicians and
providers to perform appropriate monitoring of patients for compliant use and the lack of sharing of
these medications. Prescribers of opioids for COMT must have higher expectations of patient
compliance and adherence to therapeutic plans than for patients not receiving opioids. The offices of
such prescribers must reflect this reality in the insistence of the use of pill counts, drug screens,
INSPECT report generation, frequent face to face follow ups, and employing reduction of opioid
prescribing in the face of substance abuse, intractable or dangerous side effects, or when
polypharmacy becomes a significant risk factor. Furthermore, physicians and prescribers must have
the training to know when to refuse to prescribe opioids or to force patients to make medication
choices for their own safety.
It is the purpose of this manual to reflect these truths, providing a method for judicious
opioid prescribing, and laying out the requirements for good medical practices to be employed by
prescribers in this state. It is expected this manual will be referenced by the State Board of Medicine,
State Board of Nursing, State Board of Pharmacy, State Board of Podiatric Medicine, State Board of
Dentistry, State Board of Physician’s Assistant Committee, State Attorney General, County
Prosecutors, DEA, State Police, Drug Investigative Divisions of City and Police and Sheriff
Departments. Physicians that are unwilling to engage in the due diligence in opioid prescribing and
monitoring are practicing substandard care should expect action from one of the above authorities to
correct or prohibit aberrant prescribing behaviors. As a fundamental basis for this manual, the
Indiana Pain Society developed standards of care for pain management delivery in this state in 2010
and part of those standards include opioid management. Section 5 of these standards include a
broad outline for selection criteria, follow up frequency, abuse detection, and exit strategies. This
manual expands on these standards to delineate the best practices in pain medicine to reduce
substance abuse and diversion, while providing a safer method of delivery of pain care. The keys to
reduction in patient mortality, morbidity, and drug diversion focus on adequate control over the
prescribing process and monitoring by the physician or provider, communication between
physicians and providers, the presence of deterrents to continued aberrant patient behaviors, and
adequate communication between hospitals/coroners/law enforcement with prescribers.
IPS OPIOID STANDARDS OF CARE
5. Opioid Treatment For Chronic Pain
a. Preface and Fundamental Concepts
STANDARD 5.1.1 Opioid treatment may be initiated in medically and psychologically appropriate patients
that have tried and failed other conservative treatments, and after a substance abuse screening tool or
substance abuse history survey result has been evaluated for appropriateness of prescribing opioids.
STANDARD 5.1.2 Opioids should not be the only therapy employed in pain control efforts in chronic nonmalignant pain
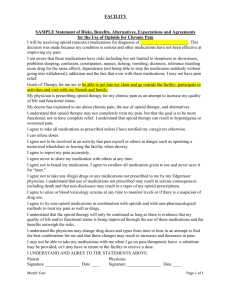
STANDARD 5.1.3 An opioid agreement will be signed by the patient prior to the prescribing of any opioids
when long-term opioid prescribing is anticipated or in any case, after 3 months of the patient taking opioids
at least weekly. This agreement makes clear the policies of the clinic, the responsibilities of the patient
being prescribed chronic opioids, the possible consequences of substance abuse or drug diversion, and
may include the required consent for opioid use as outlined in Standard 3.1.4.
STANDARD 5.1.4 Opioids may be prescribed only for the legitimate medical purpose of reduction of pain or
improvement of function unless addiction is being actively treated under a Drug Enforcement Agency special
license.
b. Referral to Other Consulting Physicians and Psychologists
STANDARD 5.2.1 Referral to other specialists may be required of the patient as a part of the continuation of
opioid therapy.
c. Follow-up Frequency
STANDARD 5.3.1 Patients receiving initiation or continuation of opioid therapy should be seen at least every
4 weeks until the patients compliant behavior and therapeutic efficacy are established. Subsequently,
patients receiving more than 120mg a day morphine (or equivalent) or less must be seen in follow-up at
least every 8 weeks or less under normal circumstances. Patients receiving 180mg a day or more morphine
(or equivalent) must be seen in follow-up at least every 6 weeks or less under normal circumstances.
d. Substance Abuse Detection Tool Employment
STANDARD 5.4.1 Patients receiving chronic opioids must have an INSPECT report generated at least every
6 months.
STANDARD 5.4.2 Urine, blood, or saliva levels of the prescribed substances and illicit substances are a
critical part of chronic opioid therapy management and for assuring patient compliance. These tests should
be employed in cases of suspected substance abuse or drug diversion, and randomly at reasonable
intervals.
e. Drug Diversion and Substance Abuse
STANDARD 5.5.1 Patients will be monitored by the opioid prescriber for substance abuse and diversion,
and will take decisive action to eliminate these issues in their patient population. Identified substance abuse
may include referral to an addictionologist, co-management with a psychiatrist or psychologist, use of more
frequent follow-ups, or referral to a drug treatment center. Drug diversion must be treated with cessation of
prescribing of controlled substances.
f. Cessation of Prescribing Opioids
STANDARD 5.6.1 Sudden cessation of opioid prescribing should not be used in patients with known
symptomatic coronary artery disease and should not be used in general unless there is evidence of drug
diversion, use of illicit drugs, or obtaining opioids from other sources.
STANDARD 5.6.2 When opioids are no longer to be prescribed due to substance abuse or diversion, the
physician will offer referral to a drug rehabilitation center or addiction treatment center. Gradual weaning
may be employed if there has been substance abuse but no drug diversion or illicit substance use.
STANDARD 5.6.3 The prescriber may withdraw opioid treatment at any time for failure to achieve adequate
pain relief, excessive or life threatening side effects, substance abuse, addiction, or drug diversion without
discharging the patient from their practice. There is no obligation of the prescriber to continue opioid
treatment in such situations.
STANDARD 5.6.4 The withdrawal of opioids due to addiction, substance abuse, or diversion will be
prominently noted in the medical record and will be communicated to all known currently treating physicians
and prescribers of record and those identified by INSPECT as prescribing opioids recently.
STANDARD 5.6.5 It is inappropriate to refer a patient to another physician or back to their primary care
provider for continued opioid therapy for pain when the patient has engaged in substance abuse, drug
diversion, or exhibits signs of addiction. In such situations patients should be withdrawn from opioids for at
least 6 months prior to re-engaging opioids, and then only under tight control with addictionology comanagement if available, otherwise with psychological counseling as an on-going part of the opioid
treatment program.
II. PHILOSOPHY
The use of opioids for the treatment of chronic pain is controversial given the societal cost of
increased morbidity, mortality, opioid related crime in obtaining and selling these medications, and
the lack of highest quality evidence based medicine studies to support its continued use. Yet there
exists a curious dichotomy regarding the treatment of non-malignant compared with the noncontroversial treatment of malignant pain, whether currently active or quiescent, with chronic
opioids. Opioids are universally accepted for the treatment of malignant pain, no matter how long
the malignancy persists, and with little regard to issues of substance abuse or diversion, ostensibly
because the treatment will have a finite endpoint of death due to malignancy or in some cases, due to
the opioids themselves. The contrary is true for chronic non-malignant pain treatment, where there
are significant medical concerns regarding substance abuse, diversion, overdose, death related to the
opioids, and lack of high quality evidence based medicine for opioid use, yet in reality the only
difference in the two types of pain or their treatment is the existence of a finite endpoint (albeit quite
nebulous in malignancy). The presence of malignancy is afforded the erroneous tacit assumption
that the occurrence of most pain is due to the malignancy, and therefore opioid treatment is justified.
On the other hand, chronic non-malignant pain may have no specific identifiable cause and produce
perceived pain that is equally severe to that of malignant pain, yet is frequently dismissed by
physicians. This gets to the crux of the matter regarding chronic pain: there is no objective method
of measurement of pain, and all pain is entirely subjective. It is therefore the belief system of the
treating physician or practitioner, colored by their background training and specialty, shaped by
experience with patients, and tempered by the presence of overlapping substance abuse issues that
determines the degree and manner of treatment of pain of different types. It is the purpose of this
manual to define the best practices for opioid treatment of pain to minimize the risks to patients.
First of all, operational definitions must be understood for use of this manual. These
definitions may not reflect the terminology used by the DSM III, IV, or V since these are all different
from one another regarding opioid use and abuse. We prefer the more commonly understood term
“substance abuse” to the more benign “substance misuse” since we believe that substance abuse is
not at all benign.
Opioid: a controlled substance operating on the mu, kappa, or sigma opioid receptor as an
agonist to produce analgesia.
Substance abuse: overuse of a prescribed controlled substance or use in a manner not
consistent with prescribing directions that has the potential to result in drug overdose, use of
an unprescribed or prohibited drug/chemical, or failure to secure the medication to prevent
loss or theft. Since it is not possible for a physician to distinguish between overuse of a prescribed
opioid with the patient running out early, theft, loss, or sale of a controlled substance, the presence of
any of these is termed substance abuse. This definition is predicated on the insistence of the
physician that the medication be used as directed, the mandatory securing of the medication,
cessation of specific controlled substance prescribed by others previously, and cessation of alcohol or
other prohibited substances. For example, the failure to stop taking hydrocodone prescribed by a
physician 3 months previously when instructed to stop all prior opioids constitutes substance abuse.
However if the physician fails to inform the patient they must stop prior opioids, then this constitutes
a less than adequate communication by the physician and is not substance abuse. A patient taking a
prn medication scripted in a manner to allow use of an entire month’s supply in 7 days is not
substance abuse- it is poor physician practice. Snorting or huffing of an opioid in all instances is
substance abuse as is the use of illicit drugs or concomitant use of alcohol. Patients having their
medications stolen is substance abuse since they have failed to provide adequate security for the
medication and such lapse has caused their prescription medication to become available out on the
street. Substance abuse may or may not be a criminal act in Indiana, depending on the offence. For
instance, the overuse of opioids is not a crime, but overuse of opioids then claiming to have had the
medications stolen constitutes subterfuge in order to obtain controlled substances and is a class D
felony under Indiana Code 35-48-4-14 that states “A person who knowingly or intentionally acquires
possession of a controlled substance by misrepresentation, fraud, forgery, deception, subterfuge,
alteration of a prescription order, concealment of a material fact, or use of a false name or false
address commits a class D felony. However the offense is a class C felony if the person has a prior
conviction.” The use of illicit drugs while receiving prescription controlled substances under this
definition constitutes substance abuse but is also a felony for possession under IC 35-48-4-6 and IC
35-48-4-7. A patient receiving simultaneous multiple scripts for opioid narcotics from several
physicians is substance abuse, but is only a felony if the physician has an opioid agreement signed by
the patient that specifically prevents such behavior or if the patient falsely denies in questioning that
they have not obtained opioids from any other source.
Drug diversion: selling, giving away, trading of a prescribed controlled substance, use of a
false name, false medical information, calling in to a pharmacy their own controlled
substances, stealing or manufacturing controlled substance prescription forms, or altering a
script are all forms of drug diversion. Larceny, theft, importing, possession with intent to sell
are also drug diversion. Drug diversion is always a crime and is responsible for more than 50% of
the deaths from opioids since more than half those who die from opioid overdose do not have a
prescription for the medication (giving away or selling a controlled substance is a Class B felony
under IC 35-48-4-2). Drug diversion by obtaining through fraud, forgery, deception, or subterfuge is
a felony under IC 35-48-4-14 and several other state and federal statutes. Drug sharing in this
country is out of control and results primarily from pain patients receiving legitimate prescriptions
who then share or sell these drugs to others. It is particularly common in families, but also friends or
coworkers frequently give away part of their supply of opioid narcotics as though they were Tylenol.
From a strictly legal standpoint, snorting or huffing or IV use of a prescribed drug constitutes drug
diversion but is rarely prosecuted.
Drug addiction: Engaging in repetitive compulsive substance abuse or drug diversion in order
to obtain controlled substances used for non-medical purposes or use in a route of
administration not prescribed. Snorting or IV use of a drug is drug addiction whereas one time
overuse of opioids is not. Repeated engagement in substance abuse or obtaining non-prescribed
opioids constitutes drug addiction.
PRESCRIPTION OPIOID OVERDOSE DEATHS AND MORBIDITY IN THE US
Accidental drug overdoses have increased by a factor of 3 time in the US and 6 times in Indiana over
the past 9 years. The main source (90%) of prescription opioids entering the population is from
physician prescriptions written for pain control, however subsequent sharing of these medications is
rampant with over 50% of prescription opioid related deaths occurring in those without a
prescription for the medication. Over 50% of opioid related deaths are in patients receiving
benzodiazepines. The number of non-fatal overdoses, admissions for drug rehabilitation, emergency
room visits, and crime related to opioid prescribing is skyrocketing in both Indiana and the US.
Physicians contribute to this epidemic of deaths and morbidity by:
1. Providing opioids when they are not justified or without clinical evidence of any pathology
2. Prescribing excess numbers of tablets of opioids making it easier to share drugs with others
3. Prescribe methadone for chronic pain in situations when this may not be appropriate (eg.
Emergency department staff initiating methadone for chronic pain, methadone maintenance
treatment facilities prescribing methadone for chronic pain, physicians prescribing
methadone without training or education about the unique pharmacokinetics and
pharmacodynamics of the medication, etc)
4. Prescribe opioids in high doses when patients are receiving benzodiazepines, using alcohol
or cocaine
5. Prescribing benzodiazepines when there is no medical justification and with no
psychometric testing or psychologist/psychiatrist evaluation AND prescribing
benzodiazepines long term without justification
6. Prescribe opioids injudiciously when there are concomitant diseases that may result in
respiratory depression including COPD, sleep apnea, liver or renal dysfunction
7. Failure to modify prescribing of opioids or sedating substances when the patient exhibits
signs or symptoms of oversedation, incoherence, respiratory depression, etc
8. Prescribing opioids for patients with recent substance abuse or drug diversion history or
with current significant psychological disorders including drug addiction
9. Prescribing with insufficient education or training of the prescriber
10. Fail to adequately educate patients about controlled substance laws and the proper use of
their medications
11. Fail to take definitive action when substance abuse, diversion, or addiction are detected
12. Fail to adequately monitor patients for appropriate use of the medications
13. Failure to require personal responsibility of the patient with respect to securing and use of
the medications
14. Failure to communicate initiation, progress, aberrancies, and termination of opioid
therapies with others treating the patient
15. Failure to interact with law enforcement when felony activity is occurring
AXIOM 1.01 A PHYSICIAN PRESCRIBING CONTROLLED SUBSTANCES HAS A DUTY TO
PRESCRIBE IN A MANNER CONSISTENT WITH ACCEPTED MEDICAL USES AND MUST MONITOR
PATIENTS FOR SUBSTANCE ABUSE, DIVERSION, DEPENDENCY, AND ADDICTION, AND TAKE
DEFINITIVE ACTION TO ELIMINATE THESE ISSUES.
CONTROL ISSUES IN PATIENTS BEING PRESCRIBED OPIOIDS FOR CHRONIC PAIN
It is a given that massive sharing of opioids is one of the major contributors of morbidity and
mortality in our society. Urine drug testing may be suggestive that either drug sharing or substance
abuse is occurring. The 2011 nation Quest laboratory urine drug test data demonstrates only 37% of
patients receiving opioids for chronic pain are compliant with the medication prescribing. While a
small minority of these results may be due to inadequate staff reporting of the medications taken at
the time or poor prescribing instructions that may permit accelerated doses when taken as direct, the
majority of the cause is substance abuse or diversion. Of the nearly 2/3 of patients that were non
compliant, 40% had none of the prescribed drug detected, 32% had additional undisclosed
controlled substances, and 28% had different controlled substances other than those prescribed.
Patients with none of the controlled substances found in the urine may be engaging in sharing,
substance abuse, drug diversion, be due to poor physician prescribing, or may be acceptable if the
patient uses medications only intermittently for pain. Of course in the latter situation, the pill count
should demonstrate an excess of prescribed medicine in most cases. The use of additional or
different controlled substances is substance abuse (failing to cease using older controlled substance
prescriptions, use of illicits) or diversion (trading for other medications). Tight controls on the
patient population through repeat urine drug testing, pill counts, INSPECT query, and working with
other physicians to reduce substance abuse in these patients have been useful in reducing aberrant
urine drug screen results. But what is too tight of control? Is cessation of all opioid prescribing in a
75 year old otherwise compliant female who lost 5 tablets in her sink a reasonable response?
III. INFRASTRUCTURE
KEY ELEMENTS:
*Everyone employed in the clinic knows the rules and enforces
them uniformly
*Patients are given a copy of the clinic rules in advance of any
prescribing
*Patients receive informed consent for opioids including risks and
benefits/alternatives before prescribing chronically
*After hour emergency treatment must be addressed in advance
*Ability to monitor patients with INSPECT, drug screens, and pill
counts must be arranged before initiating prescribing.
*Follow-up intervals must be dosage and health appropriate but
should not exceed 2 months for schedule II controlled substances and 6
weeks for high dose opioids
Prior to prescribing of opioids for chronic non-malignant pain, the prescriber must have an
operational infrastructure developed and implemented in the clinic or hospital setting. The elements
of such operational infrastructure include:
1. The opioid agreement is a document to be presented, read, and signed by the patient and
serves as the clinic rules, uniformly enforced and reiterated by all staff, physicians, and
prescribers. If the agreement is not uniformly enforced, patients may use this information to
engage in litigation against the physician should discrimination be suspected, therefore the
agreement should have a little maneuvering room built in for the physician. This document
should be revisited yearly as a reminder to patients these rules are in force. The opioid
agreement generally includes text that is designed to control the more egregious patient
behaviors, especially those that are associated with substance abuse or drug diversion. A
copy of a pro forma opioid agreement is included in the appendix of this document.
Typically the opioid agreement includes several or all of the following elements:
a.
The patient understands they have no implicit or explicit rights to opioid treatment
initiation or continuation. Opioid treatment is predicated solely on the prescriber’s
judgment that the therapy is appropriate, medically indicated, and is not contraindicated
by the patient’s history, response to the opioids, nor abuse of opioids
b. Follow up appointments are necessary to obtain controlled substance refills
c. No refills during nights, weekends, or holidays
d. It is the responsibility of the patient to assure the controlled substances are secured in a
lock box, safe, or other secure area at all times
e. Lost or stolen medications are not replaced
f. The patient will take the medication as prescribed without variation, and if there are any
significant side effects will notify the clinic
g. Overuse of medication will not be replaced by early refills or substitution of other opioid
medications. Overuse may result overdose or death and may require the patient to
undergo painful withdrawals when they run out of medication.
h. Unless prescribed by a physician for post surgical pain immediately after surgery or
dental procedures, all opioids will be prescribed by this clinic. Patients may not fill
prescriptions given to them by other physicians except for post-surgical/dental
procedure pain
i. The patient will notify the clinic before starting any new prescriptions for Valium,
diazepam, Klonopin, clonazepam, Xanax, alprazolam, Restoril, temazepam, Ativan,
lorazepam, Soma, carisoprodol, or Seroquel. The use of these medications may be
hazardous when combined with opioids.
j. The patient will not share, sell, give away, or trade any opioid or controlled substance to
anyone, including spouses, children, and parents. The police or DEA may be notified if
patients are engaging in any of the above behaviors as these constitute felonies under
Indiana law and cessation of prescribing may occur. The patient will notify the
physician if they have accumulated an excess of a given medication.
k. The patient will not obtain any controlled substance (including opioids, Valium,
Klonopin, Xanax, Soma, Adderall, Ritalin, Dexedrine, Vivanase, etc) or Ultram (tramadol)
from anyone other than a physician and only after approval of the clinic.
l. The patient is not authorized to use any old remaining supply of opioids or other
controlled substances of a different type or strength.
m. The patient may not attend a methadone clinic, Suboxone clinic, or obtain opioids or
controlled substances from the Veterans Administration Hospitals or Clinics.
n. The patient may not use any alcohol within three days of the last dose of opioid narcotic.
o. The patient may not use any illicit drugs (including marijuana, hashish, cocaine, ecstasy,
methamphetamine, etc) while a patient at the clinic.
p. The patient may have opioid and controlled substance prescribing terminated or be
discharged from the clinic if they are involved in a DUI arrest, DUI conviction, drug
overdose due to overuse of prescribed medication or use of alcohol/other drugs in
combination with the prescribed medication, use of illicit drugs, running out of
medications early, sharing or selling or trading medications with others, or engaged in
threatening or hostile behavior towards any of our staff in order to obtain controlled
substances
q. Patient monitoring is an integral part of our program and may include patient visits
during which time no opioids will be prescribed, mandatory pill counts, mandatory
urine or salivary or blood drug screens, INSPECT state controlled substance electronic
query, and discussion of your behavior or situation with other physicians, providers,
2.
3.
4.
5.
6.
pharmacists. Failure to fully participate in our mandatory monitoring program may
result in cessation of controlled substance prescribing or dismissal from our clinic.
r. If dismissed from the clinic for overuse of controlled substances, use of illicit controlled
substances, DUI, drug overdose, etc, you may be referred to a substance abuse treatment
center. You may seek another physician to treat you by calling the county medical
society or local hospital.
s. If dismissed from our clinic or had controlled substance prescribing terminated, all
physicians, providers, and pharmacists of record may be notified of the dismissal or
prescribing cessation.
An opioid consent must be included as a part of the treatment with opioids and may be
incorporated into the opioid agreement. Elements of the opioid consent include:
a. Discussion of the benefits and risks of the opioids including possible development of
addiction, substance abuse, or drug dependence that may require treatment or cessation
of the use of opioids.
b. Discussion of the risks of opioids including drug overdose and death, respiratory arrest
or compromise, unconsciousness, severe sedation or cognitive impairment, severe
constipation that may require surgery, changes in hormone levels, urinary retention,
itching, organ injury, development of opioid induced hyperalgesia, etc.
c. Discuss the risk of opioids combined with other opioids, benzodiazepines, alcohol,
cocaine, antidepressants, Soma, Seroquel, or other sedating medications or illicit drugs
d. Discuss the increased risks of using opioids in patients with sleep apnea, moderate or
severe COPD or other forms of respiratory depression, obesity, severe psychiatric
disease, liver or kidney disease
e. Alternative treatment options
After hours availability for consultation. Part of the infrastructure as part of the continuum
of care when prescribing opioids includes availability (when feasible) of an emergency
treatment plan for patients that develop complications from opioids. It is preferable to have
an after hours message to patients and other physicians that will permit emergency contact
of the prescribing physician via an electronic call forwarding service, medical exchange, or
paging. Physicians may impose the caveat that only true emergencies may use this service
or otherwise the patients risk discharge. When feasible, emergency departments and other
physicians should be able to contact the physician or a representative after hours to obtain
medical information that may be electronically or physically available to the physician.
Urine, salivary, or blood drug testing should be established with a vendor or in-house prior
to the implementation of an opioid prescribing program for chronic pain. The limitations of
the different type of tests should be known to the prescriber, and these are discussed later in
this manual. Drug monitoring analysis must be performed at least once a year randomly on
all patients.
Mandatory pill counts may be implemented with a 24 hour notice to the patient and may be
performed at the pharmacy where the patient filled the medications or in the physician’s
office. A pill counting platform surface and spatula are available and should be washed
between pill counts to avoid cross contamination of pills. Pill counts are especially useful
when a patient is suspecting of diverting a substance and are best performed half way
through the refill cycle since by that time, diverters have long since sold or traded the vast
majority of their medications. Pill counts are useful in patients engaging in overuse of
medications, “binging” early on after a refill, or in situations where the prescriber receives
information the patient is abusing the medications.
INSPECT is an essential feature of monitoring. Not only is it invaluable in the pre-emptive
assessment of patients to determine if they are candidates for opioid therapy given the
number of different physicians or dosing of medications received, but also assists in the
continuing monitoring of patients for multiple prescribers of opioids simultaneously (doctor
shopping). Doctor shoppers may be abusing the medications but may just as well be selling
the medications. INSPECT must be checked at least twice a year as per Indiana
standards. There are other monitoring programs in surrounding states not yet linked to
INSPECT at the time of the writing of this manual (such as KASPER, the Kentucky program),
7.
8.
however Indiana physicians may request password access to those systems. This is
especially important in physicians practicing near borders of other states where patients
may be doctor shopping across state lines.
Follow up intervals for patient visits depend on the severity of concomitant medical issues,
polypharmacy with multiple sedating medications, compliance with medication use
instructions, recent overdose or aberrancies in behavior, and dosage of the medications.
Patients who appear confused, sedated, disoriented should have more frequent follow up
visits for physician evaluation of the patient’s mental and sedation status. In any case,
patients with schedule II or III medications should be seen at a minimum every 12 weeks
under normal circumstances while those receiving 120mg equivalent of morphine must be
seen every two months while those receiving 180 mg equivalent of morphine must be seen
minimally every 6 weeks, even if being prescribed 3 month mail in scripts due to insurance
considerations. The follow up is not simply a time to write prescriptions but is necessary
due to changing physiology that may not be recognized by the patient (pulmonary, cardiac,
renal, hepatic dysfunction), to re-assess the appropriateness of prescribing (checking for
substance abuse and drug diversion), to assess for significant side effects and to treat
(severe constipation, sedation, respiratory depression), and to re-evaluate the current
medication therapy in light of other medications that may be prescribed or changed by other
physicians or providers. The failure to adequately monitor patients in a timely manner is a
major contributor to morbidity and mortality. Mortality rate is directly related to the dosage
of medication being prescribed suggesting there is no such thing as a “stable patient” on high
dose opioids. The risk of death in patients receiving over 100mg a day morphine equivalents
is 2 times that of low dose and over 200mg is 3-9 times the risk of low dose opioids in
published studies. American physicians can no longer ignore the increased risk by claiming
it is inconvenient for them to have adequate follow up and monitoring in patients receiving
high dose opioids. Monitoring for substance abuse is particularly important at high doses.
Patients taking 30 mg a day oxycodone may double their dose for one day without sequelae
but those taking 240 mg a day might overdose and die with a similar doubling of the dose.
The constant reinforcement to patients to take medications as prescribed and discussing the
reasons and statistics with them is an important factor in prevention of substance abuse and
subsequent overdose. Finally, changes in patient status simply cannot be assessed at three
month intervals due to potential changes in hepatic or renal function, changes in psychiatric
status (may be related to opioid induced hypogonadism), changes in pulmonary status or
development of endocrine disorders, assessment for subjective and objective shortness of
breath, and for the effects of other medications that may be added by other physicians that
could prove fatal in combination with high dose opioids due to combined sedative effect,
drug interactions due to hepatic enzymatic inhibition.
An adequate way to communicate to other physicians and providers is necessary in order to
provide information about substance abuse, drug diversion, significant side effects, etc. This
may be via electronic medical record, faxed notes, dictated letter, or other means of
permanent record entry into another physician or provider’s records.
IV. PATIENT SELECTION
One of the most difficult aspects of opioid prescribing for chronic pain is patient selection.
The criteria for who are not candidates for long term (>3 months) opioid prescribing are easier to
define than those who are appropriate candidates.
ABSOLUTE CONTRAINDICATIONS- These patients pose an extreme legal and medical risk to the
physician’s practice. Opioids should not be employed or should be withdrawn.
Patients that have not tried two or more other non-opioid medications/interventions and
failed
Patients with a history of criminal behavior of prescription drug theft, script theft, selling or
trading prescription opioids, calling in their own prescriptions, extortion or attempted
extortion for drugs at any time in the past
Use of cocaine/methamphetamine/heroin/LSD in the past 12 months or presence of these
drugs in urine drug or saliva analysis; treated for alcoholism in the past year
Snorting, huffing, or IV injections of prescribed medications anytime in the last year
Patients that refuse to provide a HIPAA medical release of old medical records directly to
you from past physicians or providers
Records from prior prescribers that have been redacted
Patients that refuse a pill count or urine or saliva drug test without just cause
Significant substance abuse or drug diversion in the past year
Recent admission to a hospital for patient induced drug overdose
Concurrently receiving suboxone or methadone for the treatment of addiction
True allergy to the drug
No medical indication for the use of opioids, patient refuses any medical diagnostic workup
for their pain condition, and patients that refuse all interventions other than opioids
History of violent behavior towards other physicians, providers, or office staff
RELATIVE CONTRAINDICATIONS- These patients must have modification of opioid regimen to
opioids with less abuse potential/overdose potential/side effect potential with very tight monitoring
if opioids are to be continued.
INSPECT reveals multiple frequent unexplained prescribers or pattern of doctor shopping
Significant COPD with hypoxia, significant respiratory difficulty, severe sleep apnea
Morbid obesity
Significant uncontrollable recurrent constipation
Significant uncontrolled urinary retention
Unconsciousness or severe sedation
History of DUI while taking opioid analgesics
High dose opioids while taking benzodiazepines of any kind
Occasional alcohol use during opioid prescribing without sequelae
Presence of THC on more than one UDS if not being prescribed marinol or equivalent
High scores for potential substance abuse on the ORT, SOAP, or other screening tests
Substance abuse with sequelae (legal, medical organ injury or intubation, ICU stay, etc)
Repeated substance abuse without sequelae demonstrating a control problem with the
medications
Patients with changing history or nebulous medical indications for opioid use or in patients
without further medical diagnostic workup for their condition
Failure to follow opioid agreement
Patients without the mental capacity to take medications as prescribed or lacks insight as to
CAUTIOUS USE- requires further evaluation in order to continue prescribing the medications
Significant hepatic or renal disease (opioid should be selected based on minimizing the
effects of the liver or kidneys on medications
Hypotension
Overuse of medications without significant sequelae once every two years
Destitute yet can afford cash payment for expensive medications
Presence of THC on single drug screen if not being prescribed marinol or equivalent
Family report of sedation, selling of medication, or untoward side effects
Extreme caution if opioids are to be prescribed at all then use only limited doses in patients
with diagnoses of fibromyalgia or chronic widespread pain, chronic low back pain without
sufficient diagnostic workup, non-specific abdominal pain without any diagnostic work up,
chronic pancreatitis, TMJ, fractures from years ago that continue to cause moderate to
severe daily pain, migraine or tension headaches, Lyme disease without any lab findings,
Reiter’s syndrome, interstitial cystitis especially without corroboration with cystoscopy,
irritable bowel syndrome, chronic pelvic pain without any findings, pre-menstrual or severe
ovulatory pain with a negative workup, arachnoiditis, chronic myofascial pain, thoracic
outlet syndrome, RSD or CRPS without any corroborative clinical findings, piriformis
syndrome, chronic coccygodynia, bursitis or tendonitis, polymyalgia rheumatic, chronic
fatigue syndrome, chronic pain syndrome undifferentiated
APPROPRIATE CANDIDATES FOR OPIOIDS- Query and Document the following elements:
Those not at risk by above criteria
Had an adequate medical diagnostic workup that may include radiological studies,
EMG/NCV, laboratory studies demonstrating some pathology that correlates with pain or
with chronic pain syndromes the ability to reproducibly describe the pain with consistency
History and focused physical exam with appropriate findings
Appropriate mental acuity to take medications as prescribed and insight to understand the
hazards of substance abuse/diversion
Patient focus on overall improvement and not on medications
Lack of symptom amplification, hypochondriasis, histrionic personality, somatization
disorders, severe untreated depression, excess anxiety
INSPECT query demonstrates no aberrant behavior
Past physicians notes (obtained direct, not via patient presenting these) should demonstrate
no aberrancies or have aberrancies adequately explained
No history of illicit drug use of cocaine, LSD, methamphetamine, heroin, etc or alcohol abuse
in the past year
Screening abuse questionnaire scores sufficiently low
Presence of security measures to eliminate others having access to the medications
Failed multiple other therapies that may include:
1. Physical therapy with demonstrated adequate effort
2. Group exercise, tai chi, yoga, zumba
3. Non-opioid medications (multiple classes or medications)
4. Psychological counseling, biofeedback, progressive relaxation
5. Chiropractic
6. Acupuncture
7. Interventional injection therapy
8. Neuroablative techniques
9. Neuromodulation techniques
It should be noted screening questionnaires all have significant false negative results. It is very
unlikely a patient with any significant history of substance abuse, drug diversion, overdose, etc will
reveal these damaging facts on a screening questionnaire, therefore these questionnaires have
limited clinical value
APPROPRIATE CANDIDATES FOR CONTINUED PRESCRIBING OF OPIOIDS
Drug testing shows results consistent with prescribed medications, lack of illicit drugs, lack
of unprescribed controlled substances
Lack of development of any of the absolute or relative contraindications
Following clinic rules
V. HIGH RISK PATIENTS
Risks may be stratified into the categories of inherent medical risks (due to their latent medical
state), dynamic medical risks (due to changing medical state), iatrogenic risks (polypharmacy, high
doses), and legal risks (family litigious, patient litigious, violence risk, drug sharing)
LATENT MEDICAL RISK: Medicaid, prior history of substance abuse, COPD, sleep apnea, baseline
hypotension, morbid obesity,
DYNAMIC MEDICAL RISKS: changes in hepatic or renal function, use of illicit drugs or alcohol
IATROGENIC RISKS: polypharmacy, overprescribing, poor prescribing habits or instructions
LEGAL RISKS: families threatening litigation due to opioid prescribing
- Medicaid populations. This group has the highest substance abuse rate and drug diversion rate of
any social service program or insured patients and predictably has a very high overdose rate from
both prescribed and un-prescribed opioids. Drug sharing among this population is endemic and drug
diversion by selling the prescriptions in order to supplement meager or non-existent incomes is
significantly problematic. In Washington State, the death rate from prescription opioid overdoses is
30.8/100,000 for the Medicaid population compared with 4/100,000 for the non-Medicaid
population, a risk factor of 5.7 (MMWR Weekly Oct 30, 2009/58(42);1171-1175) . In Washington
State, the Medicaid population died predominately from methadone overdoses vs other opioids.
Ironically, the Medicaid population may have been forced into taking this more dangerous drug by
restrictions in state Medicaid budgets that pushed patients into using this very expensive but more
lethal opioid. Indiana also has restrictions on the usage of the most tamper resistant opioids that
force physicians into prescribing a larger number of short acting tablets or into prescribing
methadone, a much more hazardous drug. The substance abuse + illicit drug use rate for Medicaid in
Kentucky is twice that of the insured population and three times the rate of Medicare patients.
- Prior History of Substance Abuse. One study (JAMA Dec 10, 2008, p2613) demonstrated of those
that died from prescription drugs, 78% had a history of substance abuse, 63% had diverted nonprescribed drugs, 22% had used nonmedical route of administration (snorting, IV, etc), 21 % had 5 or
more physicians prescribing controlled substance in the past year prior to their death, 17% had a
prior overdose history, alcohol contributed to death in 17%, illicit drugs contributed to death in 16%.
Therefore it is critically important to obtain records from prior physicians, especially family
physicians, and do due diligence in the background checks. Frequently the opioid screening tests
(SOAP, ORT, etc) are not useful tools in obtaining this information due to substance abuser
prevarication in order to obtain prescription medications. Physicians that tell or imply to patients
that the results of the screening test will not influence medication management are themselves guilty
of prevarication.
- Polypharmacy. The single greatest contribution of physicians to death of patients is prescription of
opioids to patients that are receiving other controlled substances or respiratory depressants, mostly
benzodiazepines. Whereas single drug deaths are uncommon (22%), polypharmacy deaths involving
benzodiazepines is found in half or more of those with opioid related deaths in Marion County
coroner data, West Virginia, and Miami death data. Benzodiazepines are the second most common
drug found in drug related deaths whereas opioids are the most commonly found drugs. Respiration
is controlled principally through medullary respiratory centers with peripheral input from
chemoreceptors and other sources. Opioids produce inhibition at the chemoreceptors via mu opioid
receptors and in the medulla via mu and delta receptors. While there are a number of
neurotransmitters mediating the control of respiration, GABA is the major inhibitory
neurotransmitters. Benzodiazepines facilitate the inhibitory effect of GABA at the GABA receptor,
thereby amplifying the degree of respiratory depression produced by the opioids. Like opioids,
benzodiazepines may shift the CO2 response curve to the right in addition to flattening the curve, but
also may suppress the oxygen dependent respiratory drive. IV studies have shown the addition of IV
benzodiazepines to IV opioids can increase the hypoxia rate from 50% to 90% and the apnea rate
from 0 to 50% (Murray, Opioids and Benzodiazepines in Critical Care Clinics 11(4) 1995) .
Benzodiazepines are frequently prescribed for chronic pain patients for somewhat nebulous
indications and only rarely after formal psychometric testing. Frequently patients are retained on
benzodiazepines for many years without ever having these removed or any assessment of
effectiveness. Some patients have no idea why they are taking the drug and some began receiving the
drug years before for an acute anxiety issue associated with a time limited stressful condition. The
indiscriminate prescribing of benzodiazepines combined with opioids leads to a potentially deadly
situation. There is also significant morbidity associated with combined benzodiazepines and opioids
including disorientation, slurred speech, frequent falls, etc.
In DAWN 2009 data on emergency room visits for drug issues demonstrated virtually the same
number taking opioids as benzodiazepines with significant overlap. It is therefore recommended
patients either be weaned off benzodiazepines, converted to a non-respiratory depressing nonbenzodiazepine anxiolytic (hydroxyzine, buspirone, SSRIs, etc), or that high dose opioids (more than
120mg morphine equivalent per day) be avoided.
Other commonly prescribed but problematic drugs leading to disorientation, falls,
fragmented thinking, etc include Soma (carisoprodol), Lyrica, Neurontin, and Seroquel.
-Overprescribing. Excess prescribing of opioids beyond what is medically necessary enables drug
sharing and the development of hoarding of medications that may be used for overdose or stolen.
This is particularly true with short acting opioids such as hydrocodone, oxycodone, and
hydromorphone but also with the intermediate acting methadone. Overprescribing frequently
occurs in:
Postoperative situations where patients may be given 40-100 tablets of opioids with refills
in order to avoid inconveniencing the physician with telephone calls about post operative
pain
ER situations where patients fake acute pain situations in order to obtain more opioids. ERs
may prescribe 1-2 weeks worth of short acting medications when maximally 3 days should
be prescribed
Chronic non-malignant pain where patients are given large amounts of short acting
medications (5-10 per day) without medical or financial justification for such high pill counts
and are given refills for up to 6 months on schedule III hydrocodone or codeine products.
Patients are rarely asked by prescribers how many tablets they use a day or how many pills
the patient has remaining, simply rewriting the scripts for large quantities that may be easily
shared or sold. Prescribers frequently will give refills or write multiple scripts for nonrefillable opioids for their convenience or for the convenience of patients without deference
to reasonable use amounts, pharmacokinetics and half lives of the medications, or adequate
follow up intervals.
3 month mail in scripts of high dose opioids are particularly problematic if the patients are
unreliable or have claimed loss of these high amounts of opioids. Some pharmacies will
deliver all three months supply at one time causing the patient to have massive numbers of
pills available for abuse or sale. In these situations, prescribers frequently fail to follow up at
intervals less than the 3 months scripting even though high dose opioids clearly have a much
higher risk of overdose, over-sedation, or death associated with them.
-Inappropriate Initiation of Opioids for COMT There are certain situations that are contraindicated
in the prescribing of opioids for COMT. Emergency departments should not initiate sustained release
opioids or methadone in any patient not already receiving these medications. Prescribers that do
not have opioid agreements with their patients and lack the infrastructure or appropriate monitoring
capability for COMT or who have not initiated the process to obtain old patient records should not
initiate opioid therapy as a treatment for chronic intractable pain. Methadone treatment facilities
with a prescriber inadequately trained in the treatment of chronic pain should not prescribe
methadone as a treatment for chronic pain alone in the absence of documented addiction treatment.
-Poor Script Writing Prescribers of controlled substances frequently write prn scripts for opioids at
intervals that permit patients to overdose or use excessive medications. For instance, a script
intended to last a month of Percocet 90 tablets is written for a patient with the instructions “1-2 PO
Q4H prn” Using these instructions, the patient may take 12 percocet per day (may be enough to
induce overdose) and will cause the patient to run out of medications in a little over 7 days.
Appropriate script writing would include a maximum number per day, in this case 3 per day if the
patient has chronic intractable stable pain. In cases of acute post operative pain, the script should
not be written for 90 tablets since that is too high a number for post operative pain. 20-30 tablets
without refills on a script (in the case of schedule III) would be appropriate. Too high a number of
pills written with sloppy instructions may actually delay the discovery of post operative
complications of hematoma or infection since pain associated with these conditions would be
masked by the escalated and massive use of opioids.
- Alcohol Use. Alcohol use is very common in the non-pain and pain population. Many pain patients
have used alcohol for years to dull the impact of chronic pain. Most current users will not admit to
their alcohol use. Alcohol activates the inhibitory GABA receptor to suppress respiration but also
acts to decrease the excitatory effect of A-glutamate at the NMDA receptors, thereby further
amplifying respiratory depression. In Marion County, alcohol is found as the third most common
drug associated with prescription drug deaths. One study found an odds ratio of 2.8 for daily alcohol
use as a predictor of prescription drug abuse (SUBSTANCE USE & MISUSE Vol. 39, No. 1, pp. 1–23,
2004 Gender and Other Factors Associated with the Nonmedical Use of Abusable Prescription Drugs)
-Addiction to illicit drugs For those that have had admission to hospitals for substance abuse
treatments, those with a dependency on opioids had a 5.7 times higher death rate than nonsubstance abusing individuals. Similarly, methamphetamine use was associated with a 4.67 fold risk,
marijuana 3.9 fold risk, alcohol 3.8 fold risk, and cocaine 3.0 fold risk. These deaths were not
specifically related to the drug (not examined) and may have been due to lifestyle risks associated
with drug use. (14) Those with a past history of substance abuse with smaller dose medications
(hydrocodone) frequently continue the abuse and overuse of large dose medications (oxycontin)
with sometimes fatal results. Another study (SUBSTANCE USE & MISUSE Vol. 39, No. 1, pp. 1–23,
2004 Gender and Other Factors Associated with the Nonmedical Use of Abusable Prescription Drugs)
found an odds ratio of 9.5 as a predictor for prescription drug substance abuse in those that had
engaged in illicit drug abuse in the past year.
- Sleep apnea, COPD, obesity Obesity (Body mass index known as BMI >30) is epidemic in our
society with approximately the same number of obese as with chronic pain. The obesity rate in the
US has demonstrated a steady, increase in rate that appears to be accelerating. In 1960, the obesity
rate was 12%; by 1971-75 it was 16.0%; by 1980 it was 16.7%; by 1994 it had increased to 23.3%
(NHANES data) and today 27.5 of adults in the US are obese. 73.4% of males in Indiana are obese or
overweight and overall, 30.2% of Indianans are obese. Indiana obesity has increased by 50% over the
past 15 years and the combined overweight/morbid obesity levels are now 2/3 of the population
according to the CDC (32). Obesity occurs more frequently in the chronic pain population whose
activity levels are substantially lower than those without chronic pain, yet their food intake is
unchanged. Obesity is related to sleep apnea (33), and it is shown 2/3 of those with BMI of 35 or
over have significant sleep apnea. Increasing weight is associated with a decreased functional
residual capacity (oxygen reserve in the lungs) and increasing upper airway obstruction. Methadone
maintenance opioid addict patients that gained 25% or more in body weight had a significant
increase in obstructive sleep apnea episodes (J Addict Med. 2011 Jun;5(2):141-7.) Non-obese
obstructive sleep apnea with chronic opioid use is associated with a apnea-hypopnea index (AHI) of
44 compared to normal non-sleep apnea non opioid patients have an AHI of 5. Furthermore the
respiratory pattern of sleep apnea patients taking opioids is different. The inspiratory efforts during
an obstructive event is diminished and the pauses in breathing are more pronounced. CPAP or Bipap
alone did not alter the severity of these events. (Lung. 2010 Dec;188(6):459-68. Epub 2010 Jul 24.)
Opioids and benzodiazepines may further worsen these conditions in the sleeping patient. Sleep
apnea is associated with greater periods of hypoxia (low oxygen state) at night making use of opioids
or especially opioids plus benzodiazepines far more hazardous. It has been shown taking opioids
leads to triple the number of central apneic episodes at night vs those without opioids (Pain Manag
Nurs. 2012 Jun;13(2):70-9. Epub 2010 Nov 19.)
% Indiana Obesity
32
30
28
26
24
22
20
18
16
14
12
The increased sedentary nature of the obese causes reduction in exercise capacity, thereby further
reducing cardiovascular and pulmonary reserve. It also appears that opioids are associated with the
production of sleep apnea. Up to 85% of patients using opioids were found in one study to have
sleep apnea. (37)
Severe COPD may lead to ablation of the CO2 medullary drive for respiration and dependence on the
O2 drive. Because opioids may further ablate these respiratory drive mechanisms, oxygen
dependent COPD patients may be at much higher risk of respiratory arrest with opioid use.
-Hepatic or Renal Dysfunction. The levels of most opioids rise significantly in the blood of those
with liver or kidney dysfunction. Those with these conditions need to have the dosages adjusted
downward or switch to an opioid that is not significantly affected by these issues (buprenorphine).
However many patients will develop hepatic or renal dysfunction and not know it or fail to tell their
physician prescribing opioids at the time this is discovered. Overdose may occur using normal or
same long term dosing of an opioid medication in the presence of hepatic or renal dysfunction.
Methadone is particularly sensitive to hepatic dysfunction causing prolongation of an already long
half life of the drug. Fentanyl is one of the least sensitive drugs to changes in hepatic metabolism.
Renal disease may cause the accumulation of active metabolites.
-Psychological Disorder History. The risk of substance abuse and overdose deaths is higher for
those with certain psychiatric disorders. Clinical depression leads to an increase risk ratio of 1.2-4.3
while anxiety disorders lead to a risk of 1.2-3.0 (39). A prior history of a suicide attempt may be a
significant risk factor to consider in opioid prescribing. Prior non-medical use of opioids or
persisting non-medical usage of opioids is associated with suicidal ideation, but current medical use
of opioids is not. (J Stud Alcohol Drugs. 2012 Mar;73(2):178-84.)
-Pregnancy The risk of inducing neonatal abstinence syndrome (NAS) is very high in late term
patients in methadone substitution programs (MSP). Compared to the non-MSP mothers (n = 88) the
MSP group (n = 44) had a higher incidence of smoking (6.8 non-msp vs. 84.1 % msp), alcohol
consumption (10.2 nonmsp vs. 34.1 % msp). The MSP group had a higher relative risk (RR) of
premature delivery [RR = 2.5, 95% confidence interval (CI) 1.66-3.88] and had lower birth weight
babies (adjusted RR = 2.2; 95% CI 1.31-3.71) with smaller head circumferences (adjusted RR 1.9;
95% CI 1.06-3.38). NAS occurred in 27 % (95% CI 15.0-42.8) of the MSP group. (Arch Gynecol
Obstet. 2012 Oct;286(4):843-51. Epub 2012 May 15.) Although the incidence of NAS appears to be
higher in those receiving methadone in a MSP, it also occurs with prescription opioids. In a study
observing both illicit and prescription drug use during pregnancy, these resulted in a lower mean
birth weight, longer birth hospitalization, were more likely to be born preterm, experience feeding
problems, and have respiratory conditions (all P<.001) { Obstet Gynecol. 2012 May;119(5):924-33.}
The incidence of NAS in the US increased from 1.2 to 3.4 per 1000 live birth from 2000 to 2009 with
an average charge of $53,000 for hospital treatment during 2009. (JAMA. 2012 May 9;307(18):193440. Epub 2012 Apr 30.) This syndrome may result in hospitalization in the ICU for the neonate for
months in an attempt to control withdrawal induced seizures.
-Hostile or Violent Behavior Patients with personality disorders or a past history of violence may
exhibit explosive outbursts in a pain clinic setting. While frustration may beset many in the chronic
pain population, the hostile or violent patients pose a direct and real threat to the lives and health of
the staff, physicians, prescribers, and other patients. Numerous examples exist of physicians or their
staff being killed by those disgruntled patients that felt they had no choice other than to express
themselves in a violent manner. For this reason, patients that have had prior violent outbursts,
assaulted or entrapped a physician or staff, made threatening statements or actions, engaged in
destruction of property, or created a threatening or unfriendly environment through their
interactions with other patients in the lobby, parking lot, or other locations, should not be accepted
as a patient in a pain clinic. It is imperative the past records of physicians be directly available from
past treating physicians or ERs and these records scrutinized for evidence of hostile or threatening
behavior. Patients that carry firearms into the clinical against clinic rules may place the staff and
prescribers at higher risks. Threats of violence made by any pain patient should be taken seriously
and immediate action involving law enforcement is required.
-Patients Receiving Methadone Those receiving methadone for pain control or for addiction are at
a particularly high risk with methadone resulting in 30% of all deaths from opioids even though it is
prescribed as 3% of all opioids. It is critically important that patients showing up positive for
unexpected methadone in clinical lab monitoring tests have all opioid prescribing discontinued and
that patients who are being prescribed methadone be titrated slowly upwards rather than using
equivalency charts to guide prescribing. Methadone has exponentially increasing side effects as
opposed to linear increases seen with other opioids. Special education about methadone should be
employed in patients receiving methadone.
-Other factors: Incarceration for sale or illegal use of drugs, prior overdose with opioids, high dose
opioid use
-Legal risks: Prescribing excessive amounts of opioids or in an injudicious manner leading to
overdose and death may have legal consequences. Several physicians have been charged throughout
the US with homicide or voluntary or involuntary manslaughter in 2011 and 2012 after patient
deaths have occurred ostensibly linked to opioid prescribing. Several surviving families have sued
for overdose deaths over the past decade. Risks to medical licensure, DEA licensure also exist in the
case of overdose death or injury due to overdose. Under treatment of pain is also a cause of action in
the legal system and may be an issue with medical boards due to chronic pain treatment position
statements of the Federation of State Medical Boards.
VI. PATIENT MONITORING: Pharmaco-vigilance
Close patient monitoring is critically important in maintaining control of the patient
population but also to provide adequate pain control care. Lack of patient monitoring is one of the
primary enabling mechanisms of substance abuse and diversion
A. Patient Follow-up Interval
This has been previously addressed, but in general, a dose related and behavior related
appropriate follow up interval is necessary. While it may be inconvenient for physicians to
monitor patients at appropriate intervals, it remains an integral part of the due diligence
required to write prescriptions for controlled substances. The interval of appropriate
follow up visits is independent of the patients insurance mandated prescription intervals
(eg. 3 month scripts). The appropriate follow up is not merely a perfunctory administrative
requirement but is a valuable tool in determining changes in clinical status that may
otherwise not be noted.
INSUFFICIENT PATIENT FOLLOW-UP:
Patient routinely drops by the office to pick up prescriptions without a formal inperson evaluation by a prescriber
Prescriptions are routinely called in to the pharmacy, faxed to the pharmacy, or
mailed to the pharmacy or patient without a corresponding in person face to face
encounter with the prescriber or an agent with prescribing authority
Use of a video link to perform a follow up visit
Follow up evaluation without the prescriber (or agent with prescribing authority)
and patient being physically present in the same room
Any interval longer than 3 months in follow up visits for Schedule II controlled
substances under normal circumstances
Any interval longer than 2 months for Schedule II opioids more than 120mg
morphine equivalent under normal circumstances
Any interval longer than 6 weeks for Schedule II opioids more than 180mg
morphine equivalent under normal circumstances
One year follow ups for patients that receive refillable opioids monthly or every
other month, particularly, if the patient is taking 30mg of morphine equivalent or
more every day.
Any longer than 1 month follow up for methadone receiving patients
B. Documentation Elements of a Follow up Visit
After review of the current medication list from all prescribers, the minimum
elements of documentation for routine follow up visits include:
Physical behavior/level of consciousness, observed sedation, lucidness of
thought, speech pattern
Degree of pain and effectiveness of medication management
Reported side effects from the medication
Reported, observed, suspected, or imputed substance abuse or diversion
Specific medications prescribed quantity and dosage
Further plans for testing, interventions, new medications or devices, and
referrals
New diagnoses or continuation of current diagnoses
INSPECT results at least every 6 months
Results of lab testing including toxicology studies
C.
Patient Questionnaire and Attestation
As part of compliance monitoring, it is useful to have patients sign an attestation
form on each visit that they have not received any opioids or narcotics from anyone
else and are taking only the medications currently prescribed. This effectively
becomes a legal document in cases where the patient is shown to be engaging in
substance abuse via INSPECT or clinical laboratory monitoring. This attestation in
such cases documents attempted subterfuge or deception in order to obtain
controlled substances, which is a felony offense. In cases where discharge of the
patient or conversion to non-opioid therapy is required due to such substance
abuse, this attestation documenting the patient’s prevarication serves as a potent
reason for such discharge or conversion to non-narcotic therapy. The attestation
may be included in a larger self assessment follow up document that may include
patient assessment of their functionality, pain control, psychiatric state, new pain
issues, demographic and insurance changes, etc.
D. Indiana INSPECT and PMP Programs
The Indiana INSPECT program is one of a growing number of prescription
monitoring programs (PMP) in the US and is one of the most rapidly accessible
programs in the country. To register online, use the link
https://extranet.pla.in.gov/pmpwebcenter/NewRegistration.aspx
Once you have registered, you may engage in searches on your patients. After
logging in, by encoding in the first and last name of the patient, then entering date of
birth, and checking the certification box (all indicated by blue arrows), a search
typically requires approximately 23 seconds.
This form permits additional search parameters such as city, zip, etc but they
usually are not necessary. Expanded search options include searching other years,
or expanding the search to include other selected states (slows the entire process
substantially). INSPECT is working to expand coverage into border states through
cooperative agreements. The inspect report initially generates a response page that
has information about whether or not the report can be automatically generated,
needs manual processing by INSPECT, or found no information. The response page
also lists other prescribers of controlled substances found during the search period.
On the response page is a blue link that will generate the actual report in a pdf
format.
The parameters returned by an INSPECT query in the final report include: date of
the prescription, date filled, drug and dosage, # units, # days supply, prescriber ID,
pharmacy where filled. The default search is for the past year, but past years may
also be selected when an in-depth analysis is needed. INSPECT SHOULD ALWAYS
BE USED WHEN INITIALLY PRESCRIBING CONTROLLED SUBSTANCES TO A
PATIENT AND EVERY 6 MONTHS THEREAFTER FOR CONTINUED PRESCRIBING OF
OPIOID CONTROLLED SUBSTANCES. The failure to do so is considered
substandard care by the Indiana Pain Society.
An additional feature now available is the “User Led Unsolicited Report”. After the
initial search query is submitted, at the bottom of the initial response page will be a
screen that lists other physicians and providers that have prescribed opioids. By
checking the boxes adjacent to their names, a copy of the INSPECT final report will
be automatically sent to these other prescribers of controlled substances. This is a
powerful and easy way to stop doctor shoppers and will help prevent drug
diversion. The red arrow below shows the boxes you may check in the initial
response.
The INSPECT queries are useful to:
Pre-screen patients prior to being seen in a medical practice as to
appropriateness of future opioid therapy or whether the patients are
candidates for being part of a medical practice
Pre-screen surgical patients to assist in anticipation of post operative pain
control needs, and planning for post operative analgesia
Engage in continuing monitoring of patient’s compliance with clinic
prescribing rules and state laws (works best in conjunction with a follow up
attestation by the patient as discussed in a previous section)
Rule out doctor shopping and provides the names of other prescribers that
may be contacted by your office to notify them of doctor shopping behavior
of the patient
Determine other controlled substances being prescribed by others that may
interact with opioid prescribing (esp. benzodiazepines)
Examine refill intervals of medications to assure patients are not filling
scripts early (common)
Observe number of tablets filled. Less than full script filling may suggest
the patient has financial limitations preventing purchase of full amount,
pharmacy supplies that are inadequate, or insurance limits on amounts
The INSPECT queries are accurate the vast majority of the time however there are a
few limitations of INSPECT:
INSPECT is not in real time therefore recently filled scripts (esp less than 7
days old) may not appear in INSPECT
The system is dependent on accurate coding by point of sale pharmacies.
Some pharmacies will enter the wrong prescriber’s name on occasion and
this can cause a significant problem for patient’s that are then accused of
doctor shopping. To avoid this misunderstanding, first look at the scripts
you wrote for the patient in the same date range for comparison.
Multiple patients residing in the same household may require the INSPECT
program to manually process the seach. The link to the manual search will
be sent as a email but there is a significant delay of up to 72 hours. The
email link does not specify in the email message which patient is being
manually processed therefore it is necessary to open all links to find a
specific patient. Furthermore, if a staff member is querying INSPECT, the
email link is sent to the prescriber’s personal email provided on signing up
to INSPECT, therefore the manual queries may not be available .
INSPECT only works for scripts filled in Indiana or via mail in pharmacies
(eg. Express Scripts). Patients that take their scripts across the border to fill
are not encoded as part of the INSPECT database. Other states link to the
INSPECT system as an optional search, however as a matter of protocol,
prescribers should insist that patients fill their scripts via mail in pharmacy
or in state in order to continue opioid prescribing unless there are
extenuating circumstances.
The software and hardware being used, like any computer program, is not
without occasional glitches. At times the prescriber’s ID inside the INSPECT
system may be transposed with another prescriber’s ID, then all
prescriptions written for controlled substances will appear as written by
someone else. This requires a call to INSPECT.
Occasionally INSPECT will return a null dataset in spite of a long history of
obtaining controlled substances. Usually this is due to inaccurate
information being provided on entry of data by the querying person, such
as being off one year or one day on a birthdate or misspelling a name or use
of a sobriquet in place of the formal official first name. Sometimes a recent
change of name will not be encoded or use of a new address instead of an
old address will return a null dataset. For this reason, it is best to start a
query with only the first and last name and date of birth as the only data
queried. Hyphenated names are sometimes not encoded into the INSPECT
database and therefore separate queries under each hyphenated last name
may be necessary.
As the amount of data encoded into the INSPECT database increases and as
more users query the database, the acquisition speed of report returns may
suffer.
E.
Clinical Laboratory Monitoring-Toxicology Screening
Clinical laboratory monitoring (CLM) for the detection of illicit drugs, prescribed controlled
substances, unexpected controlled substances, and the absence of prescribed controlled
substances is a critically important feature of any chronic opioid maintenance (COM)
program. The biological source is important because the detection limit time is variable. For
example, in terms of longevity of detection, hair>urine >saliva>blood. Each specimen
source has different test interferences, handling, and utility.
There are also several techniques used for analysis this that are discussed below, each with
their own limitations.
DETECTION METHODS:
1. Enzyme assay- this is the most common method used in dipstick detection of drugs.
2. TLC
3. GC/MS
4. LC/MS
5. GC/MS/MS or LC/MS/MS
The "cutoff values" for enzyme methods are typically set for opioids at 150-1000ng/ml
meaning anything below these levels will show up as negative on the test. GC/MS on the
other hand has detection limits down to 1ng/ml or less. The S/N ratio becomes problematic
at around 0.2-0.5ng/ml. Therefore GC/MS can report levels far far lower than the enzyme
methods. However some of the commercial companies will set their levels of positivity using
GC/MS artificially high, around 100 ng/ml so as not to confuse the physicians. Their
machines will detect much lower levels but they will not report anything below this level
because of the potential for erroneous interpretation. Levels below 100ng/ml must be
interpreted in the context that human metabolism may lead to specific opioids showing up in
low levels (or more accurately, 1.5% of the peak value of specific drugs such as
morphine:hydromorphone) or low levels may show up because the manufacturers of the
medications themselves may contaminate the opioid with other opioids in small quantities
in the shell of the drug or pharmacy pill preparation counters may contain residual of other
opioids thereby contaminating the medication via handling or physicians performing pill
counts in their offices on surfaces contaminated with other opioids from prior pill counts
may contaminate the patients medications. Most physicians do not know these things,
therefore simply make the tacit assumption the patient intentionally took a non-prescribed
drug when in fact they may have the drug in their system from any one of the above reasons,
and for this reason some drug testing manufacturers will report as "negative" any value
below 100ng/ml. Others will report the actual value, but will set a "cutoff" value for
positivity at 100ng/ml and report the value but will also call it negative. Others report all
the way down to 2ng/ml and call it positive if any drug is detected. These differences make
it not only confusing for physicians but invoke inconsistency in reporting the lower values
from one lab to the next. The values below 100ng/mg are usually quite accurate, but it is
their interpretation that is subject to question.
F.
Pill Counts
Pill counts may be implemented as part of the prescriber’s compliance program
however notification should be given in advance that such is a requirement for
continued therapy. Pill counts may be routine (having the patient bring all their
controlled substances with them to the follow up appointment), random (patient
selected for a random pill count), or targeted (suspicion of overuse or selling of the
medications). The targeted pill counts are best used from 1-2 weeks after the
patient fills the prescription since if they are selling all or part of the medication, it is
usually very soon after prescription filling. A reasonable amount of time (eg. 24
hours) should be used for the patient to show up at the office or the prescribing
pharmacy for a pill count. Generally, as long as the pill counts at a pharmacy are not
frequent, the pharmacies will cooperate.
Pill counts may be useful when:
There is a past history of substance abuse via overuse or current suspected
overuse
Suspicion of selling the medications or giving them away
Clinic receiving reports by friends or family of patient overuse or selling
Patient appears confused about the prescribing instructions
A negative result for a prescribed controlled substance on a clinical lab
monitoring test (eg. UDS) and the patient claims they take less than
prescribed (if true, prescribing should be adjusted downwards)
INSPECT shows early refills but patient claims they are taking the
medications as prescribed
Pill counts should be performed in the office using a pill counting plastic or
washable platform and spatula. The pills should not be physically touched by the
staff and only placed on a washed platform to avoid cross contamination with other
opioids (cross contamination may show up in clinical laboratory monitoring). The
staff must be assured that the pills, patches, or capsules presented are of the correct
identity, therefore should double check the imprint on the pill with a standard pill
identifier database. In cases where there are multiple imprinted numbers, a call to
the pharmacy is preferable to assure they actually dispensed these medications
since some patients having pill counts will try to buy enough or borrow enough of
the same pill from others to get by the pill count.
A significant deviation from expected vs actual pill count of >25% suggests the
patient has lost control over their use or security of the pills or that they are selling
the medications. If substance abuse is suspected, tighter controls (more frequent
follow up visits, fewer pills prescribed with each prescription, changing to a less
abusable medication, etc) may be employed however if selling or giving away the
medication is suspected, then discontinuing medication prescribing would be
appropriate.
Limitations on pill counts:
Patient may be able to repurchase off the street the pills necessary to
complete the count
Old pills mixed in the same bottle as new pills proves problematic since
they may come from different suppliers and have different identity marks
Cross contamination of the pills on the pill counting platform possible
Fragmentation of pills may occur
Pharmacies may not be cooperative requiring the patient to travel back to
the clinic.
Angry or hostile family or friends may pilfer part of the patient’s supply
then call in to the clinic to report they are selling the meds knowing this will
trigger a pill count. The patient may be falsely implicated via a pill count.
However in any case, this would suggest loss of security or control over the
medications by the patient.
G. Reports from Police and Law Enforcement
Police and other law enforcement reports on patients allegedly engaging in drug
diversion or substance abuse issues are very much appreciated, and should be taken
seriously. Some action should occur to verify the patient is using the medication as
prescribed after receiving such reports.
H. Reports from Documented Sources
Documented source reports such as newspaper reports of DUI, medical reports, or
callers/writers identifying themselves in reports of drug diversion, substance abuse,
addiction, or dependency should be taken seriously and require verification and
action. Failure to act to prevent further drug diversion in such situations places the
physician’s DEA and medical license at risk and may subject the physician to
criminal charges. Continuing unmodified prescribing of opioids in cases of
substance abuse, addiction, or dependency place the patient at risk of overdose and
death and risks the physician’s medical license. Reports from hospitals detailing
overdoses or alleged overdoses, must be examined and there should be serious
reconsideration as to whether these patients should continue on opioids or on a
much lower dose. Reports from drug rehab centers should elicit serious
consideration for cessation of opioid prescribing to these patients.
Modification of medication, dosage, frequency of prescribing or follow up visits, and
increased monitoring through clinical lab monitoring tests/pill counts/INSPECT
may be employed. In cases where there is indeed evidence of diversion, it may be
appropriate to stop all prescribing of controlled substances. See the later section on
“controlling patient population”
I. Reports from Undocumented or Anonymous Sources
Occasionally a prescriber will receive anonymous phone calls about a person
overusing or selling medications. Every attempt should be made to obtain as much
information as possible about the person making the call, especially if they are
hostile to the prescriber for continued prescribing. It should also be documented
specifically what medication is being sold. Others will call in to notify the prescriber
of patient oversedation or overuse of medication.
In any case, it is important to step up monitoring of the patient in such situations
without necessarily confronting the patient about their phantom accuser. Those
who make such accusations may be have their own motives for doing so including
retribution for having their request refused to be given some of the patient’s
medications, angry spouses or boyfriends/girlfriends who extract revenge on the
patient by attempting to have their pain medication discontinued, or other more
nefarious reasons. While such anonymous reports should not automatically be
discounted, they also do not require discontinuation of medication prescribing.
Attempts to verify the accusations independently should be employed.
J. Behavior of Patients in the Office, Waiting Room, Parking Lot, Outside the Office Setting
Observation of patient behaviors outside the exam room may be an important clue
in patients that are not legitimate or have ulterior motives. Patients that walk
across the parking lot carrying their cane, then use the cane once they are inside the
clinic are highly suspect as those that use walkers or canes in the office but appear
to ambulate perfectly without assistance at Walmart. Also, reports from patients in
the waiting room about those that would try to sell them medications or have
overheard conversations that the patient may be selling or trading or giving away
the medications makes the patient a target for additional compliance monitoring.
Patients seen giving their medications to others in the parking lot in exchange for
money or other medications require reporting to the police of the commission of a
crime and cessation of opioid prescribing. Finally, those that claim to be disabled or
are always in severe pain in the office yet are working full time under the radar for
cash are suspect for their motives in using the medications prescribed. Disabled
patients or those with extremely limited function or positive Waddell’s signs
observed engaging in vigorous physical activity should trigger substantial suspicion.
Patients that report 100% relief of pain with their medications and capable of all
activities are suspicious for potential drug diversion since these values do not
correspond to those of patients in chronic intractable pain.
Patients on physical exam that exhibit sedation, slurring of speech,
confusion, motor incoordination, balancing difficulties, or changes in sensorium may
be overmedicated with opioids, a combination of opioids with other medications, or
with other medications.
K. Patient Self Reporting
Patients may on occasion admit to overuse of medications without authorization by
the prescriber, use of illicit drugs, use of the medications in a route not prescribed,
obtaining medications from other physicians in the absence of an acute pain or
surgical situation, obtaining unprescribed medications from others, or register
concern that they may be “addicted” or have lost control over their use of the
medications. It is important that there be documentation of some action taken
when these situations occur and the action taken will vary dependent on the
seriousness of the patient self reporting, the repetitive nature of the infraction, and
the outcome of excessive usage or misuse of the medications. The action may be
admonishment to take the medications as prescribed, a discussion of the
responsibility according to the opioid agreement the patient signed to take the
medications as prescribed, tightening controls over patient opioid use by requiring
more frequent follow-up visits, switching to long acting opioids with fewer available
dosages, employment of more frequent toxicology testing, cessation of prescribing
of controlled substances (usually with weaning), or referral to a substance abuse
treatment facility. It is inappropriate and substandard care in such
circumstances to refer the patient to another physician for opioid prescribing
for the purpose of treatment of chronic pain.
VII. Specific Medications
VIII. Dosing and Dosage Modification
IX. Controlling Your Patient Population
X. Side Effect Mitigation
XI. Harm Reduction
XII. Planned Opioid Withdrawal Methods
XIII. Violent and Disruptive Patients
Opioid prescribing is inherently linked to patient misbehavior that may translate
into volatile and unpredictable situations. Prescribers have been killed by patients
that were suddenly cut off from opioids due to their own substance abuse or
diversion. Within the clinic, there should be available several means of both
avoidance of escalation of situations to the point violence occurs and dealing with
the violent/disruptive patients or their families. Disagreements between patients
and staff of a clinic may occur for several reasons: financial, substance abuse, errant
pill counts, obtaining opioid medications from multiple prescribers simultaneously,
violation of directives of the prescriber or conditions for prescribing opioids,
violation of opioid agreements, etc. The patient in such situations fears withdrawal
from medications, being blacklisted by physician entries in the medical record, and
being without pain treatment. More nefarious concerns may also be part of the
patient behavioral response such as if they are operating a criminal enterprise with
interruption of opioid supply resulting in devastating financial loss to them but also
potential physical harm or death to the patient or their families.
Some basic rules for diffusing a potentially volatile situation include:
Do not permit the staff over the telephone to berate patients by telling them
it is their own fault or that they should have known better. The staff should
repeat the response in a calm non-emotional manner once only, then invite
the patient to come in for an office visit to further discuss the issue. If the
patient continues to belabor the point, the staff should offer an appointment
time, and if the patient is unwilling to make an appointment, then the staff
should indicate they have done all they are permitted to do under the clinic
operating rules, and that the patient will need to arrange an appointment,
and the staff will gladly take their call in the future when they are ready to
make that appointment.
Do not confront the patient about these issues in a waiting room or within
earshot of other patients
Take the patient to an isolated room to discuss the issues in private with
staff or the prescriber
Listen to the patient’s explanation without interruption, then ask simple
probing questions to determine the degree of the infraction. Sometimes the
patient has a rational and verifiable reason for their actions or a problem
that can only be solved with prescriber intervention.
Speak in a controlled and non-emotional voice, expressing sympathy for
their situation, but that opioid prescribing agreement, Indiana law, medical
licensing board actions, and/or this controlled substance prescribing
manual prevent latitude in opioid prescribing
Give the patient several alternatives and have them make the decision
regarding the alternatives. If they cannot make up their mind in the clinic,
ask them to call the clinic with their decision. Such alternatives may include
cessation of opioid prescribing, weaning from opioids over a month (if
medically prudent), referral to a substance abuse treatment center,
modification of treatment to non-oral or extended release medications only
or to non-opioid therapy, etc.
Once the patient has indicated that they are transferring care in anger or
due to the lack of obtaining opioids, the prescriber is responsible for
emergency treatment only until that transfer occurs. If the patient indicates
they intend to transfer care and are receiving medications from your clinic,
then you may elect to cover the medications until transfer is made. If the
patient has been off an opioid medication due to overuse or loss for a
period of time of many days to weeks, then they have already gone through
withdrawal and continued prescribing of opioids may not be indicated if
transfer to another prescriber is imminent. Illicit drug use with a positive
clinical laboratory testing may not be an indication for continued opioid
prescribing since the patient has a demonstrated capacity for acquiring
their own street drugs. In such situations, use of withdrawal medications
only in limited quantities may be indicated.
If all else fails and the patient becomes hostile and threatening, pushing,
shoving, spitting upon, or assaulting staff in any way, the patient is
instructed to leave the premises immediately, the police should be
immediately called, and a clinic-wide alert given. On rare occasions, it may
be necessary for the staff to respond in a definitive manner to protect life of
the staff of the clinic, or thwart further injury. In such situations, it may be
necessary for a graded response of the staff to occur. Having an array of
interventions to use may help diffuse the situation or interrupt an assault or
entrapment. Some of these include the use of martial arts, pepper spray,
taser, CO2 BB gun, or firearm. Appendix B lists some of the available
deterrents that may be employed in a medical clinic situation. Physical
restraint of the patient should be limited to situations where the patient has
caused significant injury to others or is risking physical violence to others
or themselves and refuse to leave the clinic. The Castle doctrine law in
Indiana gives the right to employ reasonable force in the workplace under
certain conditions, specifically to protect themselves or a third person from
what the person reasonably believes to be the imminent use of unlawful
force or criminal trespass or criminal interference. However, deadly force
may be used and the person does not have a duty to retreat if the person
reasonably believes that deadly force is necessary to prevent serious bodily
injury to themselves or any third party. This right extends to the persons
automobile.
IC 35-41-3-2
Use of force to protect person or property
Sec. 2. (a) A person is justified in using reasonable force against another person to protect the person or a
third person from what the person reasonably believes to be the imminent use of unlawful force. However, a
person:
(1) is justified in using deadly force; and
(2) does not have a duty to retreat;
if the person reasonably believes that that force is necessary to prevent serious bodily injury to the person or
a third person or the commission of a forcible felony. No person in this state shall be placed in legal jeopardy
of any kind whatsoever for protecting the person or a third person by reasonable means necessary.
(b) A person:
(1) is justified in using reasonable force, including deadly force, against another person; and
(2) does not have a duty to retreat;
if the person reasonably believes that the force is necessary to prevent or terminate the other person’s
unlawful entry of or attack on the person’s dwelling, curtilage, or occupied motor vehicle.
(c) With respect to property other than a dwelling, curtilage, or an occupied motor vehicle, a person is
justified in using reasonable force against another person if the person reasonably believes that the force is
necessary to immediately prevent or terminate the other person’s trespass on or criminal interference with
property lawfully in the person’s possession, lawfully in possession of a member of the person’s immediate
family, or belonging to a person whose property the person has authority to protect. However, a person:
(1) is justified in using deadly force; and
(2) does not have a duty to retreat;
only if that force is justified under subsection (a).
APPENDIX B: DETERRENTS
Given the unpredictable and sometimes volatile interactions with those
engaged in substance abuse and drug diversion, a clinic may be equipped
with deterrents against physical harm to the staff or prescriber or other
patients.
1.
2.
3.
4.
5.
Pepper spray. This readily available low cost deterrent must be used
at close range but is often effective to temporarily blind the assailant. It
is more effective than mace.
Stun gun. These devices come in a variety of shapes and may be
concealed in an outer case made to appear to be a flashlight, cellphone,
etc. Unfortunately, they require physical contact with the assailant and
may be batted away before deployment.
Taser. A taser is a device that uses a CO2 cartridge to fire a set of
electrodes into the skin that deliver a high voltage electric charge that
incapacitates the assailant. These may be fired through clothing and do
not require direct contact. Unless the assailant is taking bath salts, PCP,
or high dose methamphetamine, the device is extremely effective at
incapacitation. Most of the non-police issue devices permit sustained
charge delivery.
Pellet and BB Guns. These generally are ineffective in stopping an
assailant. In order to penetrate completely they require unexposed
skin, a situation that is unlikely to occur in an assailant situation in a
medical clinic. Although there are some high powered BB guns with a
high capacity magazine, the cost is prohibitive compared to a firearm.
Firearms. In order to stop most people, at least a 9mm or 380 handgun
is needed. A 22ga handgun has only a diameter of 5.6mm bullet and is
frequently too small to stop an assailant although if it penetrated a vital
organ may do so but this would take time. Immediate stopping power
is found in the larger diameter guns such as a 9mm, 380, 40 caliber, 44
caliber handguns. A subcompact 380 semi-automatic is frequently
carried by judges in courtrooms and is easily concealable. There are
also physically very small pistols that are very reliable. Typically
shotguns and rifles are too unwieldy to be used in close quarters but a
pump action shotgun is a deterrent simply because of the well
recognized sound made when loading the shell.