Carbapenem resistant organisms in haemodialysis patients who
advertisement

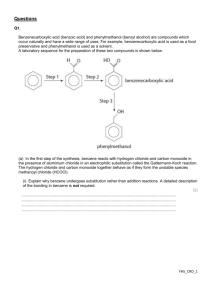
P145 CARBAPENEM RESISTANT ORGANISMS IN HAEMODIALYSIS PATIENTS WHO HAVE HAD DIALYSIS TREATMENT ABROAD: A SINGLE CENTRE EXPERIENCE MPM Graham-Brown, R Bell, Sarah Taylor, Tracey Cox, Flora Luscombe, Coral Wimbury, Heather Chamberlain, G Warwick John Walls Renal Unit, University Hospitals of Leicester NHS Trust Introduction Enterobacteriaceae are a large family of bacteria that are common amongst the normal flora that colonise the gastrointestinal tract. They are one of the commonest causes of opportunistic urinary tract infections, intra-abdominal and bloodstream infections. Enterobacteriaceae and other bacterial species are known to develop resistance to carbapenem antibiotics, and are grouped together as carbapenem resistant organisms (CRO). There is growing reliance in hospital medicine on carbapenem antibiotics to treat serious infections caused by drugresistant gram-negative bacteria (including Enterobacteriaceae), and the emergence of CRO is a worrying development. Over the last few years a number of warnings have been issued highlighting the need to screen patients returning to the UK following hospital treatment in countries with a high prevalence of CRO. Haemodialysis (HD) patients who receive dialysis abroad are all potential carriers of CRO even if they have been treated as outpatients. In our main haemodialysis unit (capacity 168), we have a large population of SE Asian patients who make frequent visits to India and Pakistan. We have introduced strict screening (by stool sampling or rectal swabs) for CRO carriage for all returning HD patients with isolation, containment and cleaning procedures in excess of those suggested by national guidelines. This has implications for patients, staff dialysis scheduling and resources. We have reviewed the results of screening these patients. Methods We reviewed all prevalent HD patients who returned to dialysis at our unit over 12 months from December 2013 having spent time dialysing at centres abroad and within the UK. We reviewed the compliance with CRO screening policy, the numbers of CRO positive swabs, where patients had been, details of their time at other units where possible and compliance with infection prevention policies in positive cases. Results From December 2013 to December 2014, 34 HD patients dialysed at ‘foreign’ units. 4 of these units were within the UK and 30 were abroad. Patients were abroad for an average of 43 days (range 4-159). 29 of the 34 patients received their care exclusively as an outpatient, with 5 requiring inpatient care abroad. 3 patients had CRO positive rectal swabs on return and all of these had received inpatient care whilst abroad. Two patients had been treated in India and one in Mauritius. None of the patients who received their care as an outpatient had positive swabs. We have not identified any invasive CRO infections. All returning patients were screened according to our policy and isolated appropriately, but this required implementation of expensive, labour intensive isolation policies, including triple cleaning of isolation rooms after dialysis with Chlor-Clean, steam clean and hydrogen peroxide fog. These policies were at the suggestion of infection prevention and microbiology colleagues and were over and above national recommendations. Conclusions Carriage of CRO in returning HD patients is potentially an increasing problem. There is little data on the efficacy of screening policies and the utility of isolation. Whilst our limited experience might suggest that only patients who have received care abroad in a hospital are at high risk of acquiring CRO carriage, we need more information and a larger sample to confirm these findings. The introduction of national reporting would allow a more reliable estimate of the risk to outpatient haemodialysis patients and a proportionate response in terms of isolation and cleaning regimes.