ELECTRONIC SUPPLEMENTARY MATERIAL Quality assessment
advertisement

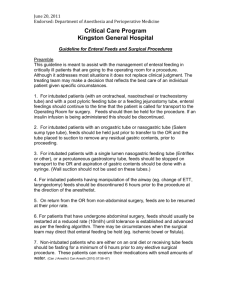
ELECTRONIC SUPPLEMENTARY MATERIAL Quality assessment of the studies included in the literature review Table S1: Quality assessment table of included articles from the literature review. A modified version of the Newcastle Ottawa Quality Assessment Scale (as detailed in methods section) was used to score each article on specific criteria for ‘selection’ and ‘exposure’ criteria, with each being awarded a maximum of three stars. Title of study First Author Date of Publication Technique/s for NET localization Selection (3) Exposure (3) 1 A controlled comparison of traditional feeding tube verification methods to a bedside, electromagnetic technique [20] Kearns P 2001 EM, Aus, Asp, pH *** *** A multicenter, prospective study of the placement of transpyloric feeding tubes with assistance of a magnetic device [61] Boivin M 2000 Mag *** *** A new technique for placement of nasoenteral feeding tubes using external magnetic guidance [62] Gabriel S 1997 Mag *** *** A new technique for post-pyloric feeding tube placement by palpation in lean critically ill patients [42] Sekino M 2012 Aus ** *** A novel method for insertion of post-pyloric feeding tubes at the bedside without endoscopic or fluoroscopic assistance: A prospective study [67] Slagt C 2004 Aus/ECG *** *** A novel technique for post-pyloric feeding tube placement in critically ill patients: A pilot study [68] Young R.J 2005 EM ** *** A randomized study of a pH sensor feeding tube vs a standard feeding tube in patients requiring enteral nutrition [26] Botoman VA 1994 pH *** *** 1 A simple aspiration test to determine the accuracy of oesophageal placement of fine-bore feeding tubes [69] Ward M 2009 Asp ** *** A simple indicator of correct nasogastric suction tube placement in children and adults [63] Rulli, F. 2007 Illum * - A team-based protocol and electromagnetic technology eliminate feeding tube placement complications [5] Koopmann M 2011 EM ** *** An evaluation of the Cortrak Enteral access system in our intensive care [56] Dolan M 2012 EM * ** Bedside placement of pH-guided transpyloric small bowel feeding tubes in critically ill infants and small children [27] Dimand, R. 1997 pH * *** Bedside postpyloric feeding tube placement: A pilot series to validate this novel technique [28] Gatt M 2009 pH ** *** Bedside sonographic control for positional enteral feeding tubes: A controlled study in intensive care unit patients [64] Gubler, C. 2006 UltraS * ** Bedside sonographic-guided versus blind nasoenteric feeding tube placement in critically ill patients [40] Hernandez_Socorro, C. 1996 Blind *** *** Capnometry and Air Insufflation for Assessing Initial Placement of Gastric Tubes [45] Elpern, E. H. 2007 Cap, Aus *** *** Colorimetric capnography to ensure correct nasogastric tube position [46] Meyer, P. 2009 Aus/CO2, CO2, Aus *** *** Comparison of four bedside indicators used to predict duodenal feeding tube placement with radiography [21] Welch SK 1994 Aus, pH, Asp, other *** *** Confirmation of nasogastric tube placement by colorimetric indicator detection of carbon dioxide: A preliminary report [47] Thomas B 1998 CO2 ** *** 2 Confirmation of nasogastric tube position by pH testing [29] Taylor SJ 2005 pH *** ** Confirmation of transpyloric feeding tube placement by ultrasonography [65] Greenberg M 1993 UltraS ** ** Confirming Nasogastric Tube Position in the Emergency Department pH Testing Is Reliable [31] Stock A 2008 pH ** - Determination of a practical pH cutoff level for reliable confirmation of nasogastric tube placement [30] Gilbertson HR 2011 pH ** *** Determining Feeding Tube Location by Gastric and Intestinal pH Values [32] Phang JS 2004 pH *** *** Does the use of an enteral feeding tube with a pH-sensitive tip facilitate enteral nutrition? [33] Ireton-Jones C 1993 pH ** ** Effectiveness of pH Measurements in Predicting Feeding Tube Placement [34] Metheny N 1989 pH ** *** Effectiveness of the auscultatory and pH methods in predicting feeding tube placement [16] Turgay AS 2010 pH, Aus *** *** Effectiveness of the auscultatory method in predicting feeding tube location [38] Metheny, N 1990 Aus * *** Electrocardiogram-guided placement of enteral feeding tubes [52] Keidan I 2000 ECG * ** Electromagnetic guided feeding tube insertion: Enhancing patient safety [70] Karmally, Z 2011 EM * ** Electromagnetic sensor guided nasojejunal tube placement in critically ill patients [71] Elliot, S 2010 EM * ** Feasibility and safety of the placement of nasoduodenal feeding tubes by nurses with the assistance of an electromagnetic guidance system (Cortrak) Mathus-vliegen, E 2009 EM * *** 3 [72] Gastric tube placement in young children [36] Ellett M 2005 CO2, pH, Birub ** ** Guiding nasoenteral feeding tubes into the distal duodenum with magnets: Results from 161 intubations [73] Gabriel, S 1998 Mag *** ** Hold that x-ray: aspirate pH and auscultation prove enteral tube placement [39] Neumann M 1995 Aus, pH *** *** Implementation of an electromagnetic imaging system to facilitate nasogastric and post-pyloric feeding tube placement in patients with and without critical illness [57] Windle EM 2010 EM ** *** Increasing the safety of blind gastric tube placement in pediatric patients: the design and testing of a procedure using a carbon dioxide detection device [41] Gilbert RT 2012 CO2 ** ** Indicators of postpyloric feeding tube placement in children [22] Gharpure V 2000 Asp, pH, Bilrub, Enz *** *** Indicators of Tube site During Feedings [23] Metheny N 2005 Asp *** ** Intestinal placement of pH-sensing nasointestinal feeding tubes [35] Berry S 1994 pH * ** Jejunal tube placement in critically ill patients: A prospective, randomized trial comparing the endoscopic technique with the electromagnetically visualized method [43] Holzinger, U 2011 EM * ** Magnetic detection to position human nasogastric tubes [74] Tobin, R 2000 Mag ** ** Magnetically guided nasoenteral feeding tubes: a new technique [75] Gabriel, S 2001 Mag *** ** 4 Methods to test feeding tube placement in children [24] Westhus N 2004 pH, Enz, Asp, Asp + pH *** ** Nasoenteral feeding tube placement by nurses using an electromagnetic guidance system (with video) [58] Mathus-Vliegen E 2010 EM ** * Nasointestinal tube placement with a pH sensor feeding tube [76] Heiselman D 1993 pH * ** Noninvasive Verification of Nasogastric Tube Placement Using a MagnetTracking System: A Pilot Study in Healthy Subjects [77] Bercik P 2005 Mag *** - Nonradiographic assessment of enteral feeding tube position [78] Harrison M 1997 Aus *** ** pH and concentration of bilirubin in feeding tube aspirates as predictors of tube placement [79] Metheny N 1999 Bilrub + pH *** * pH and concentrations of pepsin and trypsin in feeding tube aspirates as predictors of tube placement [80] Metheny N 1997 Enz + pH *** ** Placement of nasoenteral feeding tubes using external magnetic guidance [59] Gabriel S 2004 Mag ** ** Placement of nasoenteral feeding tubes using magnetic guidance: retesting a new technique [60] Ozdemir B 2000 Mag ** ** Placement of nasointestinal ph-sensing feeding tube: A prospective evaluation [81] Jimenez E 1998 pH *** ** Prospective randomised comparison study of two methods of jejunal placement of enteral feeding tubes in critically ILL patients: Endoscopic versus electromagnetic visualised method [44] Holzinger U 2009 EM * - Rapid Placement of Transpyloric Feeding Tubes: A Comparison of pHassisted and Standard Insertion Techniques in Children [82] Moore L 1996 pH ** *** 5 Report on the development of a procedure to prevent placement of feeding tubes into the lungs using end-tidal CO2 measurements [48] Burns M 2001 CO2 ** ** Serum paracetamol concentration: an alternative to X-rays to determine feeding tube location in the critically ill [83] Berger M 2003 Other ** * Small bowel feeding tube placement using an electromagnetic tube placement device: Accuracy of tip location [84] Rivera R 2011 EM ** *** Successful placement of postpyloric enteral tubes using electromagnetic guidance in critically ill children [85] October, T. W 2009 EM * *** The effectiveness of ultrasonography in verifying the placement of a nasogastric tube in patients with low consciousness at an emergency center [66] Kim, H. M 2012 pH, Aus, UltrS *** ** The use of carbon dioxide monitoring to determine orogastric tube placement in premature infants: a pilot study [49] Ellett M 2007 CO2 * ** The use of the Cortrak Enteral Access SystemTM for post-pyloric (PP) feeding tube placement in a Burns Intensive Care Unit [86] Hemington-Gorse, S. J 2011 EM - * Transpyloric feeding tube placement in critically ill patients using electromyogram and erythromycin infusion [53] Levy H 2004 ECG *** *** Ultrasound to confirm gastric tube placement in prehospital management [87] Chenaitia H 2012 UltraS *** *** Use of a colorimetric carbon dioxide sensor for nasoenteric feeding tube placement in critical care patients compared with clinical methods and radiography [50] Munera-Seeley V 2008 CO2 * ** Use of a noninvasive electromagnetic device to place transpyloric feeding tubes in critically ill children [54] Kline, A. M 2011 EM *** *** Use of a pressure gauge to differentiate gastric from pulmonary placement Swiech K 1994 other ** *** 6 of nasoenteral feeding tubes [88] Use of an electromagnetic placement device for enteral feeding tubes reduces nursing time and financial burden [89] Kenar J 2010 EM * * Use of capnometry to verify feeding tube placement [51] Araujo-Preza, C. E 2002 CO2 * *** Verification of an electromagnetic placement device compared with abdominal radiograph to predict accuracy of feeding tube placement [55] Powers J 2011 EM ** ** Visual Characteristics of Aspirates from Feeding Tubes as a Method for Predicting Tube Location [25] Metheny N 1994 Asp *** * 1. Abbreviations for the techniques are shown here: 7 Abbreviation Full name of technique EM Electromagnetic methods Aus Auscultation/insufflation Asp Aspirate: Visual inspection pH Aspirate: pH testing Bilrub Aspirate: Bilirubin testing Enz Aspirate: Enzyme testing (pepsin, trypsin) Mag External magnet guidance Illum Illumination using fibre optic UltraS Ultrasound/sonography Blind Blind insertion CO2 Capnography / Capnometry (colourmetric indicator of end-tidal CO2) ECG Electrocardiographic tracing and Electromyography Bilirub + pH Combined: Bilirubin and pH Enz + pH Combined: Enzyme and pH Aus/ECG Combined: Auscultation and ECG Aus/CO2 Combined: Auscultation and Capnography / Capnometry 8 other vacuum effect (a change from 40mL of aspirated air to <= 10mL after 60 mL of air instillation), paracetamol concentration, Pressure gauge Determining global appropriateness of methods to confirm NET tip location Methods The global appropriateness and applicability of available methods to confirm NET tip location were also evaluated. To do this the performance characteristics of each method were appraised against the needs and requirements of a representative ‘global user base’. Identifying the ‘global user base’: In order to determine the requirements for a successful global solution, a panel of stakeholders were selected to represent those involved in each stage of the process to confirm the NET tip location; from development to employment. In addition, this panel was comprised of users with various social, economic and geographic perspective. This panel consisted of experienced surgeons with familiarity working in developed and developing nations, two manufacturers / designers with an extensive background in medical device design and marketing, two dieticians and one nurse. Determining user requirements: The users’ requirements for a successful global solution were obtained by a formal interview process. Each member of the user panel was asked to discuss their experience with various methods, the advantages and disadvantages of the methods they had used and the most important requirements for a successful method. From the interviews performed, a list was compiled of all stated requirements for a method to detect NET tip location. Weighting the importance of user requirements: Once a full list of requirements had been created, the stakeholders ranked them by importance, from their perspective. This required them to assign a score of importance from 0 (not important at all) to 10 (the most important) to each of the requirements. The 9 stakeholders were then allowed to include additional comments at the end of the survey relating to any adaptations or improvements they would like to see in a new method to confirm NET tip location. Evaluating the global appropriateness of methods: In order to score the global appropriateness of each method a House of Quality (HOQ) matrix was employed [12, 13]. This is an evaluation matrix that allows the requirements of the user to be mapped against the physical performance characteristics of the method, so that its appropriateness as a technique can be directly determined. A schematic of a HOQ matrix (Figure S1) indicates the key input and output sections of this analysis. User input sections are populated using data derived from user interviews and the importance ranking exercise as described above. The reviewer input sections can be completed by using literature or the results from a trial, or in the case of a new concept, the design specifications, and results from concept stage testing. The interaction matrix sections are completed by moving through each of the performance characteristics and looking for any interaction / correlation (positive or negative) with any of the other performance characteristics, and / or the user requirements, e.g. the performance characteristic of price per disposable tube is negatively correlated to the user requirement of low cost per tube and positively correlated to the performance characteristic of durability of the tube. The completed top of house and inside house matrices can be used to determine which performance criteria are the most interrelated and have the strongest connection to the user requirements. This is done for each performance characteristic with a weighted sum of how many points of interaction they have with other performance characteristic (top of house) and user requirements (inside house). The weighting is based on the strength of correlation as shown in Table S2. Thus the key output from this HOQ matrix is the weighted importance of the performance characteristics for a NET tip location method. The importance weightings are the combination of the weightings of the user requirements and the interaction matrices. These weights allow the review of current methods from the perspective of the ‘global user base’ and can inform a targeted approach to designing a new or improved method. 10 Figure S1: Schematic of House of Quality matrix Key: ‘Top of house’ Interaction matrix (Performance characteristics) User input Reviewer input Analysis output ‘Inside house’ Interaction matrix (User requirements – performance characteristics) Competitive analysis Importance weightings User requirements Performance characteristics Target performance values Importance weightings 11 Table S2: Weightings and symbol for the matrix correlation indicators for House of Quality analysis. Inside house Top of house Matrix Description Positive correlation Strong positive correlation Negative correlation Strong negative correlation Strong relationship Moderate relationship Weak relationship Weighting 1 2 1 2 3 2 1 Symbol + ++ -Θ Ο ▲ Table S3: Stakeholder requirements and ranking of importance Stakeholders Stakeholder requirement High successful placement rate Low risk to patients Universal language suitability/suitable for illiterate users Clinician (Developing nation experience) General surgeon Dietician Manufacturer/ Designer Ranked Average 8.0 10.0 9.0 9.0 9.0 6.0 10.0 10.0 9.0 8.8 9.0 8.0 9.0 8.0 8.5 12 Low learning curve/training required Viable cost of materials Low Price Viable cost for manufacturing Minimal maintenance required Durable tube Comfort not reduced Relevant design expertise available Ease of use (ergonomic) Friendly design for visually impaired operator 9.0 9.0 7.0 9.0 8.5 8.0 8.0 9.0 8.0 8.3 9.0 8.0 8.0 8.0 8.3 8.0 8.0 7.0 8.0 7.8 9.0 7.0 8.0 7.0 7.8 9.0 7.0 10.0 5.0 7.8 7.0 8.0 9.0 6.0 7.5 8.0 6.0 8.0 7.0 7.3 6.0 8.0 7.0 8.0 7.3 8.0 7.0 7.0 7.0 7.3 13 Friendly design for audiologically impaired operator Non-perishable product Sterile/can be sterilised Reliable supply of materials Minimal extra disposables required (beyond tubes) Low/no power requirement FDA/appropriate certificate/approval obtained Low environmental impact Time for development High product packing density 8.0 7.0 7.0 7.0 7.3 9.0 7.0 8.0 4.0 7.0 6.0 7.0 10.0 5.0 7.0 8.0 5.0 8.0 6.0 6.8 8.0 5.0 6.0 8.0 6.8 9.0 6.0 4.0 7.0 6.5 5.0 7.0 6.0 6.0 6.0 4.0 6.0 4.0 7.0 5.3 5.0 2.0 6.0 4.0 4.3 5.0 2.0 6.0 4.0 4.3 14 Low patent presence of similar technology 0.0 1.0 15 8.0 6.0 3.8 Table S4 The results of the ‘top of house’ interaction matrix analysis, ranking the most interrelated performance criteria. Performance criteria Level of interrelation Success rate (Specificity, sensitivity) 9 Market size (number of tubes, $$ for devices) 8 Lifetime of disposable 8 Size 7 Cost per tube for disposables 7 Cost for non-disposable components 7 Approved/certificated 7 Power supply (V) 6 Patient discomfort/pain rating during procedure 6 Size of visual indicators 6 Lifetime of non-disposable portion (time before required maintenance/disposal) 6 Duration of procedure 5 Weight 5 Toxicity of materials 5 Training required 4 Predicted rate of use of disposables (per patient) 4 16 No words - uniformly recognisable symbols only 4 No Audible only alarms/signals 3 Lead time on products 2 17 Table S5: The results of the ‘inside of house’ interaction matrix analysis, ranking the most interrelated performance criteria with user requiremen. Performance criteria Level of interrelation Cost per tube/disposables 34 Lifetime of non-disposable portion (time before required maintenance/disposal) 29 Success rate (Specificity, sensitivity) 27 Cost for non-disposable components 26 Market size (number of tubes, $$ for devices) 25 Lifetime of disposable 25 Power supply (V) 25 Toxicity of materials 25 Predicted rate of use of disposables (per patient) 23 Training required 20 Approved/certificated 16 Duration of procedure 12 No words - uniformly recognisable symbols only 12 Size 11 Size of visual indicators 10 18 No Audible only alarms/signals 10 Patient discomfort/pain rating during procedure 9 Weight 9 Lead time on products 8 Table S6: The ‘House of Quality’ performance criteria ranked by average importance to stakeholders Stakeholders Performance criteria Cost per tube/disposables Success rate Cost for non-disposable components Lifetime of nondisposable portion Lifetime of disposable Predicted rate of use of disposables (per patient) Power supply (V) Toxicity of materials Training required Clinician General surgeon Dietician Manufacturer / Designer Ranked Average 10.1 8.3 9.3 9.8 9.5 8.9 9.6 9.3 9.6 9.1 8.6 8.1 8.0 8.2 8.2 8.9 7.8 7.7 7.8 7.9 8.2 8.0 7.3 8.1 7.8 7.0 7.1 5.9 5.8 6.6 6.5 6.5 6.5 7.0 6.4 6.4 6.0 6.3 6.9 6.1 6.3 6.7 6.7 6.2 6.2 19 Market size (number of tubes, $$ for devices) Approved/certificated No words - uniformly recognisable symbols only Patient discomfort/pain rating during procedure Duration of procedure Size Size of visual indicators Weight Lead time on products No Audible only alarms/signals 5.1 4.2 5.3 5.0 6.1 4.7 6.1 4.4 5.6 4.6 3.8 3.7 3.3 3.8 3.7 2.6 2.8 2.6 2.5 2.3 2.4 3.5 3.2 2.5 2.5 2.0 1.5 3.3 3.0 2.7 2.2 2.2 2.5 3.0 2.9 2.8 2.5 2.5 2.0 3.1 3.0 2.7 2.4 2.3 2.1 2.2 2.0 1.8 2.1 2.0 20