PPT
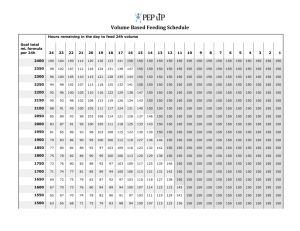
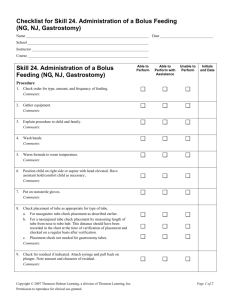
advertisement

Practical and emotional issues of tube feeding: Research into the Parent Perspective Laurie Eyles Specialist Dietitian Project Background Increasing patient numbers and complexity + Increasing pressure on limited resources + Inequity between adult and paediatric services + Risk that patients on HETF could be lost to follow up Need to investigate current position Project Aim and Objectives Identification Identificationofofall all patients patients Definition of current model of care To define the current service provision for children and young people at home on tube feeding and identify any service improvements necessary Supplies and equipment processes Audit of best practice statements Investigation of patient/parent experience Patient and parent experience: postal questionnaire • 163 questionnaires sent, 58% response rate • 95% of respondents were parents of child/young person on HETF • 8 questions asked to ascertain: – Adequacy of training on HETF – Optimal modes of delivering HETF training – Level of professional support for HETF – Location of follow up – Key areas for improvement Patient and Parent Experience Q. What level of information about HETF were you given to begin with? 5% About right Not enough 95% Patient and Parent Experience Q. What would be the best way for you to get information on HETF? Other 1 Mode of information Other children/parents 18 Video/DVD 23 Website 26 Written Booklet 49 In Person 84 0 10 20 30 40 50 Number of respondents 60 70 80 90 Patient and Parent Experience Q. Who would you contact with any tube feeding problems? Other 3 Health Professional GP 10 Company nurse 35 Hospital nurse/doctor 36 Dietitian 36 Community Nurse 73 0 10 20 30 40 50 Number of respondents 60 70 80 Patient and Parent Experience Q. What level of health professional support do you get for tube feeding? 13% About right Not enough 87% Patient and Parent Experience Q. How would you like to be reviewed? Other 1 Location of review School 5 Local hospital 13 email 15 GP Practice 17 Telephone 37 Home visit 46 Specialist hospital 47 0 5 10 15 20 25 30 Number of respondents 35 40 45 50 Patient and Parent Experience More time to go over things Easier access to dietitians One supplier for all products Better communication with parents More dietetic input What is the one thing the NHS could do to support you with home tube feeding? Support group for the whole family Nurseries and schools need more information on why tube feeding is needed More support for oral feeding programmes Regular monitoring Have someone available to visit at short notice to avoid hospital visit Patient and Parent Experience • Questionnaire provided excellent basis for generalisation of the population but we wanted to know more! • Issues further explored through “parent stories” • Seven parent stories, one to one interviews • Recorded and transcribed • Themed together with questionnaire Parent Stories Theme 1: Supplies and equipment “It would be helpful for parents to have one supplier or contract for supplies. When my child was first tube fed, everything came from Homeward, now supplies are limited and you have to contact Homeward for some and Vygon for others and CCNs for others etc. It’s a bit of a hassle. It would be easier if there were one point of contact” “Make deliveries easier. With lots of different OPD appointments it’s not possible to stay in all day for a delivery” “We never know who to contact to sort out supplies, keep getting passed on to a different person for different things and it takes ages” Parent Stories Theme 2: Communication “I was given mixed messages, consultant told me to stop feeding her myself and use the nasogastric tube only….then 2 hours later a nurse told me that was wrong and I should continue to breast feed her…..I didn’t know what to do for best” “We were told confusing messages…one doctor told us to stop our son’s feed but our GP gave us different advice….what was the right thing?” “We want people to realise that we get very stressed keeping our children alive (thankfully) in this manner and we need to be understood and supported well. It’s very scary at first!” “When everything is going well, you don’t hear from anyone” Parent Stories Theme 3: Decision Making “Nasogastric feeding was discussed, but we weren’t given the choice….it was distressing but we understood that he needed it” “It was shock to hear he needed a PEG, we didn’t understand it. We wanted someone to sit down with us with pictures, complications…..by just reading about it we were unable to understand…it would help if it was more practical, less theory” “He was originally on a specialist feed which was going well, then when he was sent home it was changed…..no-one told me why. I tried to tell the nurses that he wouldn’t tolerate this new feed but no-one would listen. It wasn’t until he had lost lots of weight that I could get someone to listen to me” The Way Forward Recommendations using parent experience: 1. Have a designated key professional to contact for all tube feeding issues, who: • • • Is easily contactable Can deal immediately with problems or liaise on families behalf Has specialist knowledge of the needs of a tube fed child 2. Review entire supplies and equipment procedure and make it simple. 3. Regular community support at a venue suitable for the family 4. Involve families in each stage of the decision making process 5. Recognise the knowledge and expertise that families can offer. One final thought…. “I would like all professionals….doctors, nurses, dietitians, speech and language therapists, health visitors to understand…to wonder what to do when your child vomits, when the tube falls out and you have to run to hospital, be woken up in the middle of the night and feel the grief and the pain and the emotion and the suffering that the parents go through. Then one day they will listen to the parents, not all parents are wrong – take the parent’s experience” Parent Questions? Contact: laurie.eyles@nhslothian.scot.nhs.uk