ICU Data Collection Sheet Instructions
advertisement

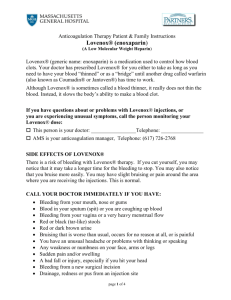
ICU Round Sheet Instructions Circle Yes or No-Place completed forms in the Trauma Manual ICU Day-# of total days in ICU Intubated Method- Either Nasal, Oral or Trach Low Tidal Volume/Plateau Pressure- Usually patients with ARDS, ask MD if confused Daily Sedation Holiday- Has the Propofol or other sedation withheld (every 12 hours) and patient allowed to “wake-up?” Ask the nurse. Daily Weaning Assessment- Was the Patient assessed by Nursing or Respiratory for ventilator weaning? (Pressure support, tubecompensation to obtain a tidal volume of 300-400 cc, watch the patient’s RR, O2 sats, VS for 30 minutes, Rapid Shallow Breathing Index (RSBI), Peep decrease, or Weaning parameters (NIF)) Gross Circuit Contamination-Is there visible contamination in the circuit (not counting condensation). Continuous Subglottic- Is the ETT a Hi/Lo ETT vs Regular ETT tube? Suction at 20 mmHg-Is the Hi/Lo ETT connected to continuous suction at 20 mmHg? Visually inspect. HOB @ 30° or greater- Is the HOB at 30° or greater (look at railing on bed)? Place an * if patient cannot medically raise their bed to 30°. Nutritional Evaluation-Is there a Nutritional evaluation (look under the Orders section, and then look under consults)? Insulin Protocol Initiated-Is the Insulin Protocol started? You must first look at the patients “Patient Care orders” to see if the Insulin Protocol was ordered. Insulin Protocol Followed- Look at the Diabetic Record. Just look at the last 24 hours (or last 4 Blood glucoses if on Q6hr schedule). -Blood glucose every 6 hours, If successive values greater than 120 mg/dl, then change blood glucose to every 4 hours. -If Sliding scale Insulin Protocol has been used for 12 hours and blood glucose levels remain greater than 140 mg/dl, initiate Critical Care Insulin Infusion Protocol and Notify MD -Change Blood Glucose to AC & HS when patient tolerating PO GI Prophaylaxis-Is Pepcid or Nexium ordered? Lovenox Initiated-Is Patient on Lovenox? Lovenox Appropriate-Does the patient have a medical reason to NOT be on Lovenox? Ex. Recent trauma (usually 24-48 hrs), head bleed, splenic injury, recent surgery, planned surgery for that day, MD stated do not start Lovenox, etc. SCDs-Are the patient’s SCDS on (You must look at the patient)? DVT Prophylaxis-Is the patient on Lovenox or SCDS or both? Invasive Device Protocol followed-Field IV’s should be D/C’d within 24 hours. Peripheral IV sites should be D/C’d every 4 days. Dressings should be changed whenever visible soiling is present. Central lines should be D/C’d every 14 days. Central line dressing change every 7 days. Ask the nurse for the dates on the IV starts or use the IV documentation in Cerner. Visually inspect all invasive devices for S/S of infection. Foley? How long?-Does the patient have a foley? How long has it been in? PT/OT ©-Has PT/OT been consulted (look under Orders, then under Physical Medicine)?