LIVER PATHOLOGY-Gohara
advertisement
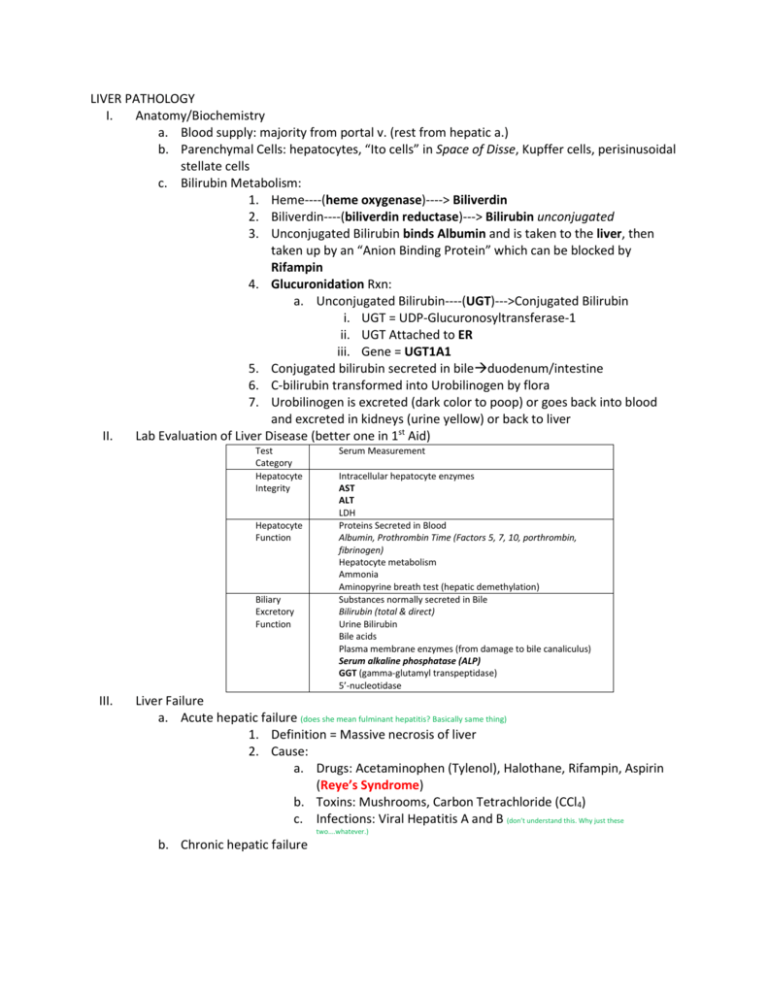
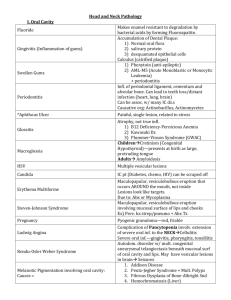
LIVER PATHOLOGY I. Anatomy/Biochemistry a. Blood supply: majority from portal v. (rest from hepatic a.) b. Parenchymal Cells: hepatocytes, “Ito cells” in Space of Disse, Kupffer cells, perisinusoidal stellate cells c. Bilirubin Metabolism: 1. Heme----(heme oxygenase)----> Biliverdin 2. Biliverdin----(biliverdin reductase)---> Bilirubin unconjugated 3. Unconjugated Bilirubin binds Albumin and is taken to the liver, then taken up by an “Anion Binding Protein” which can be blocked by Rifampin 4. Glucuronidation Rxn: a. Unconjugated Bilirubin----(UGT)--->Conjugated Bilirubin i. UGT = UDP-Glucuronosyltransferase-1 ii. UGT Attached to ER iii. Gene = UGT1A1 5. Conjugated bilirubin secreted in bileduodenum/intestine 6. C-bilirubin transformed into Urobilinogen by flora 7. Urobilinogen is excreted (dark color to poop) or goes back into blood and excreted in kidneys (urine yellow) or back to liver II. Lab Evaluation of Liver Disease (better one in 1st Aid) Test Category Hepatocyte Integrity Hepatocyte Function Biliary Excretory Function III. Serum Measurement Intracellular hepatocyte enzymes AST ALT LDH Proteins Secreted in Blood Albumin, Prothrombin Time (Factors 5, 7, 10, porthrombin, fibrinogen) Hepatocyte metabolism Ammonia Aminopyrine breath test (hepatic demethylation) Substances normally secreted in Bile Bilirubin (total & direct) Urine Bilirubin Bile acids Plasma membrane enzymes (from damage to bile canaliculus) Serum alkaline phosphatase (ALP) GGT (gamma-glutamyl transpeptidase) 5’-nucleotidase Liver Failure a. Acute hepatic failure (does she mean fulminant hepatitis? Basically same thing) 1. Definition = Massive necrosis of liver 2. Cause: a. Drugs: Acetaminophen (Tylenol), Halothane, Rifampin, Aspirin (Reye’s Syndrome) b. Toxins: Mushrooms, Carbon Tetrachloride (CCl4) c. Infections: Viral Hepatitis A and B (don’t understand this. Why just these two….whatever.) b. Chronic hepatic failure 1. Cause: Cirrhosis = Endstage liver damage characterized by disruption of the normal hepatic parenchyma by bands of fibrosis that separate parenchymal nodules. a. Cirrhosis Etiology, Pathogenesis, and Clinical Features (1st Aid, Pathoma) c. Clinical Features 1. Jaundice—scleral icterus; increased serum bilirubin 2. Hypoalbuminemia—edema 3. Hyperammonemiahepatic encephalopathy (from elevated ammonia) 4. Hyperestrogenemia a. Palmar erythema (local vasodilation) b. Spider angiomas c. Hypogonadism & Gynecomastia in Males 5. Coagulopathies 6. Hepatorenal syndrome (Renal failure due to liver failure) a. IV. V. VI. VII. HOW? = Portal HTN triggers systemic arterial vasodilation leading to decreased perfusion of the kidneys despite RAAS activation (pre-renal azotemia) Hereditary Hyperbilirubinemias a. Increase in UC-Bilirubin —absent or decreased activity of UGT1 enz 1. Crigler-Najar Syndrome Type I a. Absent activity; fatal 2. Crigler-Najar Syndrome Type II a. Decreased activity; Autodominant 3. Gilbert’s Syndrome a. Decreased activity b. Increase in C-Bilirubin—impaired biliary excretion of bilirubin 1. Dubin-Johnson Syndrome 2. Rotor Syndrome Infectious Hepatitis (A, B, C, D, E) a. Clinical Course i. Incubationpreicteric phasesymptomatic/ictericconvalescence (recovery) b. Carrier State i. No clinical symptoms but infectious to others; can dx with serology/lab values c. Morphology 1. Drop-out necrosis 2. Periportal necrosis 3. Fatty change (in Hep C) 4. Ballooning degeneration Hepatitis A a. ssRNA virus (naked icosahedral) b. Incubation: up to 6wks c. Fecal-oral transmission d. Mild, self-limiting e. DX: IgM Ab in acute phase; IgG Ab later indicating immunity Hepatitis B a. Hepadnaviridae = dsDNA virus (enveloped) b. incubation: up to 6months VIII. IX. X. XI. XII. XIII. c. Parenteral transmission d. Outcomes 1. Subclinical disease with remission (majority) 2. Acute hepatitis 3. Chronic hepatitis (carrier or chronic cirrhosis) 4. Fulminant hepatitis e. Predispose to Hepatocellular Carcinoma f. Markers 1. HBsAg: + = you have it (except window) 2. HBsAb: protective (you defeated it, or are immunized) 3. HBeAg: + = you’re infectious 4. HBcAb: IgM (acute), IgG (chronic or resolved) 5. HBV-DNA: same as HBeAg; indicates infectivity Hepatitis C a. Flaviviridae = ssRNA (enveloped) b. incubation: up to 6months c. parenteral and close contact transmission d. Outcomes 1. Recovery 2. Chronic heptatitis (majority) 3. Fulminant (rare) e. DX: PCR for HCV RNA in acute phase for 1-3wks; HCV Ab after 3-6wks Hepatitis E a. Water borne infectionHigh mortality among pregos! b. DX: PCR for HEV RNA; IgM & IgG Ab’s Hepatitis D a. Co-infection with acute HepB (looks like HepB alone) b. Superinfection in chronic HepB carrier (looks like acute hepatitis in previously unrecognized HBV carrier) c. DX: IgM & IgG Ab’s, HDV RNA, HDAg in Liver Chronic Viral Hepatitis a. Definition = symptomatic or serological evidence of continuing or relapsing hepatic disease > 6months (+histologic documentation) Fulminant Hepatitis a. Definition = (acute liver failure) when hepatic insufficiency progresses from onset of symptoms to hepatic encephalopathy within 2-3 weeks Autoimmune Hepatitis a. Indistinguishable from viral hepatitis b. Tx = anti-inflammatory drugs c. Assoc with autoimmune disease 60% of the time (but most autoimmune diseases are associated with other autoimmune diseases) d. Classification 1. Type 1 Ab’s—Associated with HLA-DR3 a. Anti-ANA Ab b. Anti-Smooth muscle Ab (SMA) c. Anti-actin Ab (AAA) d. Anti liver & pancrease Ab’s (SLA/LP) 2. Type 2 Ab’s a. Anti-KLM-1 (kidney-liver-microsome-1) i. A.k.a. Anti-LKM-1 ii. Binds to CYP2D6! b. Anti-Liver Cytosol-1 (ACL-1) XIV. XV. XVI. Metabolic Liver Diseases a. Non Alcoholic Fatty Liver Disease (NAFLD), Steatohepatitis-Steatonecrosis (NASH) i. Principle cause of Cryptogenic Cirrhosis (unknown cause) ii. Two Hit Hypothesis—Pathogenesis 1. (hit 1) Hepatic Fat accumulation + (hit 2) Hepatic Oxidative Stress 2. Lipid Peroxidation Reactive Oxygen Species Cell damage b. Hemochromatosis i. Excess Fe leads to deposits/free radical damage of organs including liver ii. Deficiency of Hepcidin (no longer can stop release of Fe into blood from Macrophages nor Intestinal cell) iii. Mutation of HFE gene on chrom 6 1. Cysteine Tyrosine Mutation on AA 282 = C282Y iv. Clinical Fx’s (“Bronze Diabetes”) 1. Joint pain 2. Bronze Skin 3. Diabetes 4. Erectile dysfunction/atrophy of testicles 5. Arrhythmias (& CHF) v. Hemosiderosis = Fe deposition in tissues due to transfusions; see iron in Kupffer cells; NO cirrhosis c. Wilson’s Disease d. Alpha-1 Antitrypsin Deficiency i. Results in hepatitis/cirrhosis and emphysema (esp. PiZZ genotype) ii. PAS+ cytoplasmic inclusions in liver iii. Hepatitis presents neonatally or late onset Intrahepatic Biliary Disease a. Secondary Biliary Cirrhosis i. Extrahepatic biliary obstruction (gallstone, biliary stricture, chornic pancreatitis, carcinoma of pancreatic headj ii. Sx’s = Pruritis, jaundice, dark urine, light stools, hepatosplenomegaly iii. Lab = increase in C-bilirubin, cholesterol, bile acids and ALP iv. Histo: bile ductular proliferation with surrounding PMNs and portal tract edema b. Primary Biliary Cirrhosis—autoimmune i. Labs & Sx’s same as secondary; + anti-mitochondrial IgM Ab ii. Histo: See dense lymphocytic infiltrate in portal tracts + granulomatous destruction of bile ducts c. Primary Sclerosing Cholangitis i. Inflammation of bile ducts (both inside and outside liver) ii. Labs & Sx’s same as secondary; + IgM increase (Hyper IgM gammaglobulinemia) iii. Assoc with Ulcerative Colitis and can lead to secondary biliary cirrhosis and cholangiocarcinoma (cancer of bile ducts) iv. Histo: periductal portal tract fibrosis & stenosis of ducts Drug Induced Liver Disease—Chart pg 158 a. Cholestasis—Anabolic & Contraceptive Steroids; Estrogen replacement therapy b. XVII. XVIII. XIX. XX. (Bland/Pure Cholestasis)—condition in which the flow of bile from the liver slows or stops; http://livertox.nih.gov/Phenotypes_bland.html c. Cholestatic hepatitis—many antibiotics, phenothiazines d. Steatosis—Ethanol, methotresxate, corticosteroids, total parenteral Nutrition i. Reversible “Macrovesicular” fatty change of the liver e. Steatohepatitis—Amiodarone; Ethanol f. Fibrosis & Cirrhosis—Methotrexate, isoniazind, enalapril g. Granulomas—Sulfonamides h. Vesicular Lesions i. Sinusoidal obstruction syndrome (veno-occlusive disease); obliteration of central veinschemotherapy, herbal teas ii. Budd Chiari Syndrome—oral contraceptives iii. Sinusoidal Dilatation—oral contraceptives iv. Peliosis hepatis—blood filled cavities not lined by endothelial cellsanabolic steroids, Tamoxifin i. Neoplasms i. Hepatic Adenoma—oral contraceptives, anabolic steroids ii. Hepatocellular Carcinoma, Cholangiocarcinoma—Thorotrast iii. Angiosarcoma—Thorotrast, vinyl chloride Alcoholic Liver Disease a. Etiology: 8 beers or more a day b. Pathenogenesis: i. Induce cyt P450 and immunologic attack on liver ii. Free Radical Formation iii. Alcohol directly toxic to mitochondria and microtubules iv. Acetaldehyde by-produce induces lipid peroxidation and damage c. Hepatic Steatosis—Why Alcohol makes you fat i. Alcohol Dehydrogenase uses up NAD+ (needed for FA-Oxidation; if FA-Oxidation is “off” then concomittently FA-Synthesis is “on”) ii. Acetaldehyde metabolized into Acetyl-CoA (building block for FA); increased levels lead to FA-Synthesis iii. High NADH/NAD ratio decreases glycolysis (NAD needed) and increases gluconeogenesis and glycerol 3 phosphate which is shunted into lipid synthesis (glycerol backbone) d. Alcoholic Hepatitis e. Alcoholic Cirrhosis Side Note: according to http://www.brown.edu/Courses/Digital_Path/systemic_path/hepatobiliary/cardiacsclerosis.html, Passive Congestion leads to…Cardiac Sclerosis = Cardiac Cirrhosis = Congestive Hepatic Fibrosis Impaired Blood Flow into The Liver a. Passive Congestion and Centrilobular Necrosis (leads to cardiac cirrhosis if severe) b. Peliosis Hepatitis = primary dilatation of sinusoids (drug induced)*see above Hepatic Venous Outflow Obstruction a. Veno-occlusive Disease = Sinusoidal Obstruction Syndrome (small veins of liver are occluded; due to chemotherapy and herbal teas *see above) b. Budd Chiari Syndrome—Hepatic v. thrombosis; can be acute, subacute, chronic; heptomegaly, weight gain, ascites, abdominal pain. May develop varices and visible back & abdominal veins. Absence of JVD. Assoc with hypercoaguable states, polycythemia vera, pregnancy and hepatocellular carcinoma. XXI. XXII. XXIII. XXIV. c. Passive congestion = stasis of blood in liver (“Nutmeg Liver”) due to impaired hepatic v. drainage caused by heart failure (right sided usually); can progress to cardiac sclerosis and can also get centrilobular congestion and necrosis Hepatic Diseases in Pregnancy a. Pre-eclampsia = (gestational hypertension) new-onset of HTN in pregnant woman; or increase in BP in prego who was previously hypertensive b. Eclampsia = Hypertensive emergency (severe elevation of BP >180/120) c. HELLP Syndrome: Hemolysis, Elevation of Liver enzymes, Low Platelets; considered by some an extension of severe pre-eclampsia. Complication = DIC. Neoplasms a. Benign Tumors i. Cavernous Hemangiomas 1. Present age 30-50; biopsy contraindicated!! (risk of hemorrhage) ii. Adenomas 1. Related to estrogen and anabolic steroid use; risk of rupture (abdominal pain and shock) b. Malignant Tumors i. Hepatoblastoma: mixed epithelial and mesenchymal; caused by chromosomal deletions ii. Angiosarcoma 1. Endothelial origin; assoc with arsenic, vinyl chloride exposure with long latent period. Primary Carcinoma of the liver = Hepatocellular Carcinoma a. Risk Factors: HBV, HCV, Wilson Disease, Hemochromatosis, alpha-1-antitrypsin deficiency, alcoholic cirrhosis, aflatoxins from Aspergillus. b. Marker = elevated alpha-fetoprotein Metastatic Tumors a. Most common type of tumors in liver; Multiple; commonly come from breast, lung, colon and pancreas metastases. b. Lesions outgrow blood supply leading to necrosis