Structure Outline -- Intros
advertisement
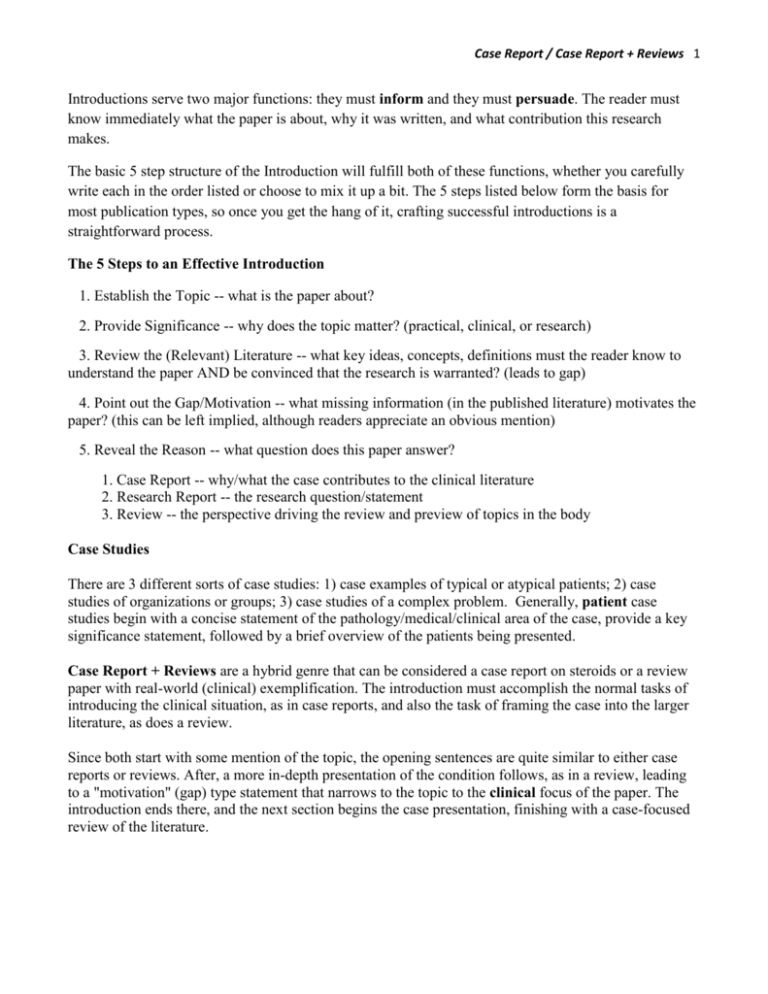
Case Report / Case Report + Reviews 1 Introductions serve two major functions: they must inform and they must persuade. The reader must know immediately what the paper is about, why it was written, and what contribution this research makes. The basic 5 step structure of the Introduction will fulfill both of these functions, whether you carefully write each in the order listed or choose to mix it up a bit. The 5 steps listed below form the basis for most publication types, so once you get the hang of it, crafting successful introductions is a straightforward process. The 5 Steps to an Effective Introduction 1. Establish the Topic -- what is the paper about? 2. Provide Significance -- why does the topic matter? (practical, clinical, or research) 3. Review the (Relevant) Literature -- what key ideas, concepts, definitions must the reader know to understand the paper AND be convinced that the research is warranted? (leads to gap) 4. Point out the Gap/Motivation -- what missing information (in the published literature) motivates the paper? (this can be left implied, although readers appreciate an obvious mention) 5. Reveal the Reason -- what question does this paper answer? 1. Case Report -- why/what the case contributes to the clinical literature 2. Research Report -- the research question/statement 3. Review -- the perspective driving the review and preview of topics in the body Case Studies There are 3 different sorts of case studies: 1) case examples of typical or atypical patients; 2) case studies of organizations or groups; 3) case studies of a complex problem. Generally, patient case studies begin with a concise statement of the pathology/medical/clinical area of the case, provide a key significance statement, followed by a brief overview of the patients being presented. Case Report + Reviews are a hybrid genre that can be considered a case report on steroids or a review paper with real-world (clinical) exemplification. The introduction must accomplish the normal tasks of introducing the clinical situation, as in case reports, and also the task of framing the case into the larger literature, as does a review. Since both start with some mention of the topic, the opening sentences are quite similar to either case reports or reviews. After, a more in-depth presentation of the condition follows, as in a review, leading to a "motivation" (gap) type statement that narrows to the topic to the clinical focus of the paper. The introduction ends there, and the next section begins the case presentation, finishing with a case-focused review of the literature. Case Report / Case Report + Reviews 2 #1: Lethal giant cell arteritis with multiple ischemic strokes despite aggressive immunosuppressive therapy / http://www.ncbi.nlm.nih.gov/pubmed/20609853 Giant cell arteritis (GCA), also called temporal arteritis, is the most common form of systemic vasculitis in adults, typically involving large and medium-sized vessels in patients over the age of 50. The majority of patients respond well to treatment with high-dosed steroids. A subset of patients develops a more malignant course with recurrent ischemic strokes from involvement of the distal vertebral or internal carotid arteries. We present two patients with GCA involving both the bilateral distal vertebral and internal carotid arteries with repeated infarcts and death despite escalating immunosuppressive therapies. Medical condition/situation Problem presented by case Brief intro to patient cases, including outcomes #2: Two cases of recurrent stroke in treated giant cell arteritis: diagnostic and therapeutic dilemmas / http://www.ncbi.nlm.nih.gov/pubmed/20661069 Stroke is the most common cause of death in giant cell arteritis (GCA),1 occurring in 3% of patients in the 10 weeks following the diagnosis of GCA.2 The extent to which persistent inflammatory vasculitic occlusion, thrombocytosis, procoagulant effect of inflammatory mediators, iatrogenic effect of steroids, or coexisting atherosclerosis might contribute to this risk is unclear.3,4 This creates a diagnostic and therapeutic dilemma in treating patients recently diagnosed with GCA, who present with stroke after initiation of steroid therapy. We report 2 patients with GCA who developed repeated strokes in different circulatory territories following steroid initiation, despite resolution of cranial symptoms and normalization of inflammatory markers. The extensive and frequent pattern of onset was disproportionate to their risk factor profile for atherosclerosis. In the first case, MRI imaging and repeat temporal artery biopsy (TAB) suggested persistence of arteritis, and an increase in immunosuppressive treatment was associated with an arrest in the sequence of recurrent strokes. Autopsy findings in the second case suggested persistence of arteritis. This progressive pattern of stroke onset following corticosteroid initiation has not been previously reported. Medical condition/situation Problem presented by case Brief patient introduction, including outcomes Significance of case within the literature – may be here or in discussion Case Report / Case Report + Reviews 3 #3: Neurological Evaluation by Intraoperative Wake-up During Carotid Endarterectomy Under General Anesthesia / http://www.ncbi.nlm.nih.gov/pubmed/15211163 Local anesthesia during carotid endarterectomy (CEA) is popular, and maintenance of consciousness enables close evaluation of cerebral function during carotid cross-clamping. 1–4 However, patients often experience pain, discomfort, or anxiety induced by the surgical procedure and by lying still for a long period, particularly when anatomic difficulties associated with a short neck, obesity, or high carotid bifurcation are encountered. 5 General anesthesia can relieve patients from such stressors. However, neurologic assessment is less reliable under general anesthesia than under local anesthesia, as the clinician must rely on electroencephalography (EEG), somatosensory evoked potentials (SEP), stump pressure, or intracranial hemoglobin oxygen saturation as determined by infrared spectroscopy (rSO2), all of which represent indirect methods for neurologic assessment. 2–4,6 The present report describes a unique anesthetic management strategy for CEA patients incorporating the advantages of both general and local anesthesia. Basically, general anesthesia is combined with local anesthesia for the surgical field and airway. This technique allows not only minimization of patient stress but also thorough assessment of neurologic function by waking the patient from general anesthesia during carotid cross-clamping. Medical condition/situation Problem presented by case Medical condition/situation Problem presented by case Brief intro to patient cases, including outcome Your Case Report Introduction 1. What is the medical condition or situation? 2. What is the problem the case presents vis-à-vis the medical condition or situation? 3. Provide brief patient introduction: make the problem in (2) clearly related and include a brief outcome. 4. What is the significance of this case for readers or within the literature? #1: Gamma knife radiosurgery for essential tremor: A Case report and review of the literature / http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2851695/?tool=pubmed Essential tremor is a common type of movement disorder that normally affects people over the age of 65; however, this illness can occur in younger patients as well. In recent years, ET has been categorized as a heritable condition, which can be transferred to family members in an autosomal dominant fashion [1]. The primary symptom of ET involves shaking of the hands during voluntary movements, but it may also present with movements of the head, face, tongue, and lower limbs [13]. Other than tremors, there are no other direct medical symptoms associated with ET and it does not decrease life expectancy. However, many patients with ET have difficulties accomplishing their daily tasks or other activities that affect quality of life, which is how this disorder elicits a negative impact on the social and mental wellness of the patients who bear this illness [1,4]. There are multiple treatment options for ET patients. The most common medications utilized are beta-blockers. Unfortunately, these are contraindicated for many patients with asthma, diabetes, and certain heart conditions. Anti-seizure medications and botulinum toxin injections are also used, but they are known to cause unwanted side effects. Stereotactic RF thalamotomy is the most common neurosurgical procedure for treating ET. It involves MR imaging of the thalamic target (ventralis intermedius nucleus), placement of an electrode neurosurgically, stimulation of the target, and creation of a lesion through tissue ablation [5]. DBS is also an invasive surgical procedure performed as an alternative to RF thalamotomy. DBS involves the implantation of a device that utilizes electrical impulses to block abnormal nerve signals [5,6]. Even though surgical treatments such as RF thalamotomy and DBS are effective in many patients with ET, there are those who are not qualified candidates for invasive neurosurgery because of comorbid medical conditions. These include patients who use anticoagulants, who have advanced cardiac or respiratory disease, who are known to be noncompliant, and who are of advanced age. An alternative for such patients is thalamotomy using GK radiosurgery. GK thalamotomy is a safe alternative to invasive neurosurgery, and evidence shows it is successful in the treatment of ET and similar movement disorders [5,711]. Also, because this disorder often occurs at a late age, and pharmaceuticals can have significant side effects, GK can be the only treatment option for this population of medication-intolerable patients. We present an inspiring case of an ET patient, whose daily life was drastically modified by the severity of her hand tremors, until GK thalamotomy treatment restored her ability to control movement and pursue her passion of painting. Case Report / Case Report + Reviews 4 Topic sentence – identifies condition Extended definition/basic introduction to condition -also provides significance (in gray) Lit review narrowing to clinical focus Well-developed problem statement – motivation for case and also justifies review Patient case, including outcome #2: Cerebral amyloid angiopathy related inflammation: three case reports and a review / http://www.ncbi.nlm.nih.gov/pubmed/20935328 Cerebral amyloid angiopathy (CAA) is characterised by β amyloid deposition in the walls of small to medium sized arteries, and less frequently veins and capillaries, of the leptomeninges and brain.1 2 CAA can occur sporadically or rarely as a hereditary syndrome.3 The pathogenesis remains uncertain but it is likely that amyloid is produced locally in the brain and accumulates as a result of reduced clearance.4–6 CAA is found in between 23% and 57% of an asymptomatic elderly population on histopathology examination.7 CAA is also found in a number of disease states, most commonly dementia and intracerebral haemorrhage (ICH). In a review of four population studies with histopathological data, 55–59% of patients with dementia had evidence of CAA compared with 7–24% of patients without dementia.8 CAA associated ICH accounts for 10–34% of ICH and typically occurs in patients in their eighth decade or older. CAA associated ICH is more likely to be lobar in location, is often multifocal and tends to recur more frequently than hypertensive haemorrhage. CAA is also associated with transient neurological symptoms, particularly in older patients, who may present with multiple, stereotyped episodes of predominantly sensory symptoms. These transient symptoms are presumed to be focal seizures and the episodes often respond to antiepileptic medication. A less common manifestation is CAA related inflammation (CAA-I). CAA-I presents with acute or subacute onset of headaches, cognitive and behavioural changes, seizures and focal neurological deficits. In addition to CAA-I, this condition has been labelled primary angiitis of the CNS associated with CAA; amyloid angiopathy and granulomatous angiitis of the CNS; cerebral amyloid inflammatory vasculopathy; cerebral amyloid angiitis; cerebral amyloid angiopathy associated with giant cell arteritis; and amyloid β related angiitis.9–15 All of these names emphasise the association between cerebral amyloid angiopathy and inflammation of blood vessels. We prefer the label CAA-I as perivascular inflammation may also be found. We report three patients with pathologically confirmed sporadic CAA-I who presented between 2001 and 2007. Patients were included if they presented with encephalopathy and had histopathological evidence of perivascular or intramural vascular inflammation and deposition of amyloid in blood vessels in those parts of the cerebral cortex and leptomeninges affected by the inflammatory changes. The findings from 69 previously published cases are summarised. We propose diagnostic criteria for CAA-I. Case Report / Case Report + Reviews 5 Topic – identifies condition/medical situation More basic info – incudes hint of research significance signaled by the word “uncertain” Significance (practical and clinical) + lit review Relevant clinical information + motivation for case/review Patient case, including outcomes + review and its contribution Case Report / Case Report + Reviews 6 Structure of the Case Report + Review Introduction 1. What is the medical condition or situation? (sometimes includes more information, an extended definition) What is the significance of this condition/situation? 2. Lit Review that focuses on motivation for case report and review 3. What is the problem the case presents vis-à-vis the medical condition or situation? 4. Provide brief patient introduction: make the problem in (2) clearly related and include a brief outcome. 5. What is the significance of this case for readers or within the literature? Provide a preview or focus statement of the body sections.