MODERATE BLOOD TRANSFUSION TRIGGERS AND SURGICAL
advertisement

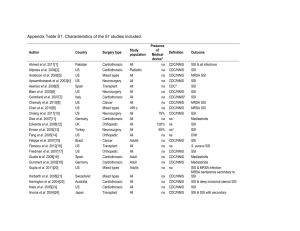
MODERATE BLOOD TRANSFUSION TRIGGERS AND SURGICAL SITE INFECTIONS IN COLORECTAL SURGERY Caitlin W. Hicks MD, MS1; Steven M. Frank MD2, Jack O. Wasey BM BCh2, Julie A. Freischlag MD1, Martin A. Makary MD, MPH1; Elizabeth C. Wick MD1 1 Department of General Surgery, Johns Hopkins Hospital, Baltimore, MD 21287 Department of Anesthesiology & Critical Care Medicine, Johns Hopkins Hospital, Baltimore, MD 21287 2 Background: The decision to transfuse can be difficult given the potential concern for ongoing bleeding in the context of physiologic fluid shifts following major surgical procedures. Guidelines support restrictive hemoglobin (Hb) transfusion triggers (7-8 g/dL) following major surgical procedures based on randomized trials demonstrating equivalent outcomes and observational studies showing decreased infections compared to higher transfusion triggers (10 g/dL). Our aim was to evaluate the association between moderate transfusion triggers (79g/dL) and surgical site infections (SSI). Methods: We prospectively followed all patients undergoing colorectal surgery at an academic tertiary medical center (07/2010-11/2012). SSI and blood utilization (blood transfusions and Hb prior to transfusion) were measured using ACS-NSQIP and institutional blood utilization databases. Multivariate regression was used to determine impact of transfusion on SSI. Results: 337/829 (38%) colorectal surgery patients had a nadir Hb of 7-9 g/dL during hospitalization. Transfused patients (35.9%, 121/337) were older (61±16 vs. 52±16 years; p<0.0001) with a higher proportion of males (47.1% vs. 34.3%; p=0.02) and higher mean ASA class [3 (IQR 3,3) vs. 3 (IQR 2,3); p<0.0001] compared to non-transfused patients. There were no differences in race, body mass index, wound classification, smoking history, or COPD between groups. On univariable analysis, SSI incidences were similar between transfused and non-transfused patients (Table). The risk-adjusted odds of SSI after transfusion was 1.1 (95% CI 0.63, 1.89; p=0.74) after accounting for standard general surgery NSQIP risk factors for SSI. Conclusion: Use of a moderate hemoglobin transfusion trigger (7-9 g/dL) does not increase risk of SSI. Blood transfusions can be used judiciously without increased risk of morbidity in colorectal surgery. Table. Univariable Analysis of Surgical Site Infections (SSI) and RBC Transfusion Infectious Outcome RBC Transfusion P value Yes (n=121) No (n=216) % (#) % (#) 23.1 (28) 23.6 (51) 0.92 Superficial SSI 16.5 (20) 17.1 (37) 0.89 Deep SSI 0.0 (0) 2.3 (5) 0.16 Organ space SSI 6.6 (8) 4.2 (9) 0.33 Any Surgical Site Infection