NRS1313 - Job Specification ( - 61 KB)

Clinical Nurse Specialist Diabetes
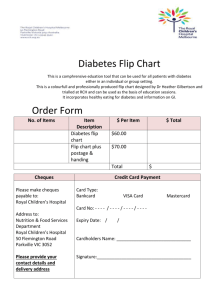
Job Specification Template, Terms & Conditions
Job Title and
Grade
Campaign
Reference
Closing Date
Proposed
Interview date(s)
Taking up
Appointment
Location of Post
Clinical Nurse Specialist Diabetes
(Grade Code: 2632)
NRS1313
Wednesday, 25 th February 2015 at 12 noon
Week Commencing 23 rd March 2015
A start date will be indicated at job offer stage
Organisational
Area
Details of Service
Reporting
Relationship
Purpose of the
Post
A panel will be created for the Diabetic Day Care Unit, Cork University Hospital, Wilton, Cork from which all permanent and specified purpose vacancies of full or part time duration will be filled.
HSE South
The Diabetes Day Care Unit offers a comprehensive specialised service for adults with diabetes. Referrals are accepted from county and general hospitals, general practice, CUMH, paediatrics and other specialities within the Cork University Hospital. The service is delivered on both an in-patient and out-patient basis.
The Diabetes Day Care Unit works to ensure that every individual receives the best care. This is done by empowering people with diabetes and their families to be active participants in their management with the goal of leading a healthy life. The team structure at present consists of
Consultant Endocrinologists, Diabetes Nurse Specialists, Dieticians, Podiatry and Secretarial
Support.
Professional Accountability: Director of Nursing.
Operational Accountability: Assistant Director of Nursing
Clinically responsible to: Consultant
The management of Diabetes demands a broad range of professional skills which includes communication, counselling, leadership, teaching and research. The Clinical Nurse Specialist
Diabetes is described as an administrator, leader, manager, collaborator, practitioner, advanced clinician, consultant, educator and researcher. The role has emanated from the premise for the need to provide social and psychological support and education on how to manage disease for patients and their families.
The Clinical Nurse Specialist Diabetes has the expertise and specialist knowledge to incorporate these skills into practice and develop standards of care that benefits the patient. It has been suggested that patient orientated outcomes are positively influenced and significant benefits accrue for patients with the involvement of the Clinical Nurse Specialist Diabetes .
The Clinical Nurse Specialist Diabetes is considered an important contribution to advancing clinical practice and nursing diagnosis and recognised as an advisor in setting standards and policies of care.
The Clinical Nurse Specialist Diabetes plays a pivotal role within the multi-disciplinary team.
The recognition of the contribution of the Clinical Nurse Specialist Diabetes in helping patients achieve good glycaemic control highlights his/her essential role in diabetes care. The Clinical
Nurse Specialist Diabetes works in collaboration with the team to ensure continuity of care lends towards more successful management. The role of the Clinical Nurse Specialist
Diabetes is defined as the provision of primary, secondary and tertiary care to people who are diagnosed with Diabetes where nursing intervention contribute to a healthy lifestyle and prevention of complications associated with diabetes.
1
Principal Duties and
Responsibilities
Clinical Focus
The Clinical Nurse Specialist Diabetes will:
Articulate and demonstrate the concept of nursing and midwifery specialist practice within the framework of relevant legislation, the Scope of Nursing & Midwifery Practice Framework
(ABA 2000), Code of Professional Conduct and Ethics for Registered Nurses and
Registered Midwives (Nursing & Midwifery Board of Ireland (NMBI), 2014)and Practice
Standards for Midwives (ABA, 2010).
Perform nursing / midwifery assessments and plan and initiate care and treatment modalities within agreed interdisciplinary protocols to achieve patient / client centred outcomes; evaluates their effectiveness
Identify health promotion priorities in the area of specialist practice
Implement health promotion strategies for patient / client groups in accordance with the public health agenda
Have a working knowledge of HIQA Standards as they apply to the role, including National
Standards for Safer, Better Healthcare (2012), National Standards for the Prevention and
Control of Healthcare Associated Infections (2009), National Hygiene Services Quality
Review (2008); Standards and Criteria etc. and comply with associated HSE protocols for implementing and maintaining these standards.
The clinical role of the Clinical Nurse Specialist Diabetes includes:
Organising the planning and implementation of care for people with diabetes and their significant others.
Encouraging a healthy lifestyle behaviour as part of health promotion strategy.
Working in collaboration with other colleagues and as a member of the multidisciplinary team to provide specialist advice for people with diabetes.
Providing a telephone advice service for ongoing assistance and advice.
Developing and providing a nurse-led clinic service where appropriate
Participating in the provision of a specialist outpatient service for people with diabetes.
Participating in the provision of psychological care for people with diabetes and their significant others.
Altering treatments within the prescribed clinical options recognising agreed protocols.
Maintaining accurate and completes nursing records.
Establishing clear referral patterns for communicating and co-operating with medical, nursing and other relevant professionals such as general practitioners, public health and practice nurses.
Providing a service that is evidence based and aims to improve quality of life for people with diabetes.
Improving the standards of care by promoting nursing research and developing nursing expertise.
Evaluating the effectiveness of education programmes on an on-going basis.
Direct care is defined as the assessment, planning, delivery and evaluation of care to patients and their families (NCNM, 2008).
Components of the role of the Clinical Nurse Specialist Diabetes include:
Patient assessment and diagnosis.
Care prioritized based on assessment.
Nursing interventions based on evidence based practice.
On-going assessment, monitoring and evaluation.
Patient education, discharge planning and referral to other sources of care within their specialist practice.
This is achieved by:
Setting realistic educational and treatment goals.
Assessing and evaluating the learning abilities of patients.
Educating people with diabetes so that they can manage their diabetes and enable
2
them to learn to lead a full, active and healthy life.
Involving significant others where appropriate in the teaching process.
Encourage people with diabetes to become active partners in their care.
Acting as a resource person for people with diabetes.
Providing individual and group education for people with diabetes and their families.
Providing a service for special needs groups with diabetes, such as paediatrics and adolescents, young adults, expectant mothers, ethnic minorities and those with learning difficulties.
Indirect care is defined as care, which relates to the activities which influence others in their provision of direct care (NCNM, 2008)
This includes:
Actively participating in the management of the Diabetes Service.
Making management decisions for which the Clinical Nurse Specialist Diabetes is professionally accountable.
Making autonomous decisions with/or on behalf of the patient and/or carer to augment and support their health potential and promote their continuity of care.
Promoting a safe environment for patients in accordance with Health and Safety,
Infection Control and Risk Management Guidelines.
Devising appropriate protocols, policies and guidelines with the multidisciplinary team.
Setting standards appropriate for a learning environment for patients and/or carer and staff.
Be actively involved in clinical decision making.
Be actively involved in the on-going development and implementation of service plans
with the relevant personnel.
Participating in the development and successful implementation of multidisciplinary care pathways incorporating national and local guidelines.
Establishing and maintaining links across services by providing a pivotal role between primary and secondary care.
Identifying service needs in relation to change and best utilizing available resources.
Patient Advocate
The Clinical Nurse Specialist Diabetes will:
Enable patients / clients, families and communities to participate in decisions about their
health needs
Articulate and represent patient / client interests in collaboration with the multidisciplinary team
Implement changes in healthcare service in response to patient / client need and service
demand
Organise, interpret, intervene and monitor care of the patient with diabetes.
Act as a patient advocate using clinical specialist knowledge and skills in the area of diabetes care.
Take responsibility for initiating primary, secondary and tertiary care for people with diabetes.
Act as a role model and uses non-cohesive influence to direct others.
Ensure that the approach to care recognises the unique needs and views of individual patients and their families.
Establish and maintain communication links with service users and voluntary groups to promote patient centred care.
Promote public and professional awareness for the care of people with diabetes.
3
Education and Training
The Clinical Nurse Specialist Diabetes will:
Provide mentorship, preceptorship, teaching, facilitation and professional supervisory skills for nurses and midwives and other healthcare workers
Educate patients / clients, families and communities in relation to their healthcare needs in
the specialist area of practice
Identify own continuing professional development needs and engage accordingly
The domain of diabetes nursing practice is underpinned by the concepts that guide the way in which diabetes nurses deliver care. The provision of diabetes education within the hospital setting is dependant on the diabetes nurses’ ability to: o o
Assess and respond to the educational needs of staff and students.
Continually liaise with the training and academic departments to deliver on-going o o o programmes of diabetes education both in the hospital and in the community.
Demonstrate responsibility for professional growth by ensuring personal and professional development.
Demonstrates a knowledge of, and work within the Code of Professional Conduct and
Ethics for Registered Nurses and Registered Midwives (NMBI, 2014).
Ensures that professional practice is researched based best practice and is clinically effective .
Audit and Research
The Clinical Nurse Specialist Diabetes will:
Identify, critically analyse, disseminate and integrate nursing / midwifery and other evidence into the area of specialist practice
Initiate and participate in evaluations and audits
Use the outcomes of audit to improve service provision
Contribute to service planning and budgetary processes through use of audit data and specialist knowledge
The scope of diabetes nursing practice is defined as the range of roles, functions, responsibilities and activities which diabetes nurses are educated to perform. This includes developing the evidence base of diabetes nursing practice by:
Being actively involved in research that is relevant to clinical practice.
Being actively involved in data collection for the purpose of auditing and evaluating the service provided.
Setting standards appropriate to a learning environment.
Devising and updating local written protocols and guidelines based on evidence based best practice that meets national and international standards.
Playing an active role in service development by working in conjunction with the multidisciplinary team and management in devising service plans based on audit and research.
Consultant
The Clinical Nurse Specialist Diabetes will:
Provide leadership in clinical practice and act as a resource and role model for specialist practice
Generate and contribute to the development of clinical standards of practice and guidelines
Use specialist knowledge to support and enhance generalist nursing / midwifery practice
Acts as a role model and resource by providing professional leadership in clinical practice.
Promote and foster good relationships with other professionals and departments to enhance multidisciplinary team working and develop efficient and effective patient care pathways.
Promote research and development and participate in local, national and international committees and conferences.
4
Eligibility Criteria
Qualifications and/ or experience
Health & Safety
Contribute to the development of policies, procedures, guidelines and safe professional practice and adhere to relevant legislation, regulations and standards
Have a working knowledge of HIQA Standards as they apply to the role, including National
Standards for Safer, Better Healthcare (2012), National Standards for the Prevention and
Control of Healthcare Associated Infections (2009), National Hygiene Services Quality
Review (2008); Standards and Criteria etc. and comply with associated HSE protocols for implementing and maintaining these standards.
Management
Provide an efficient, effective, and high quality service, respecting the needs of each patient / client
Effectively manage time and caseload in order to meet the needs of a changing and developing service
Continually monitor the service to ensure it reflects current needs, ensure that service users and others are treated with dignity and respect.
Act up when required in the Nursing Structure
Lead on Clinical Practice and Service Quality to include complaint management
Implement and manage identified changes
Ensure that confidentiality in relation to patient /client records is maintained
Maintain accurate and up to date statistics of the service provided, including audit of patient / client contacts
Represent the specialist service at local, national and international meetings as required
Maintain accurate and contemporaneous records / data on all matters pertaining to the planning, management, delivery and evaluation of this service in line with HSE requirements
The Clinical Nurse Specialist Diabetes will support, promote and actively participate in sustainable energy, water and waste initiatives to create a more sustainable, low carbon and efficient health service.
The above Job Description is not intended to be a comprehensive list of all duties involved and consequently, the post holder may be required to perform other duties as appropriate to the post which may be assigned to him/her from time to time and to contribute to the development of the post while in office.
Each candidate must, at the latest date for receipt of completed applications for the post:
Be registered in the General Division of the Register of Nurses of Bord Altranais agus
Cnáimhseachais na hÉireann (Nursing Midwifery Board Ireland) or be entitled to be so registered and
Have at least 5 years post registration experience in the Division of the register in which the applicant is currently practicing and
Have a minimum of 2 years experience in the Specialist area of Diabetes nursing care* and
Have the ability to practice safely and effectively fulfilling his/her professional responsibility within his/her scope of practice
5
Post Specific
Requirements and
Demonstrate evidence of continuing professional development and
Must hold a Level 8 post registration Quality and Qualifications Ireland major academic award relevant to the specialist area of Diabetes prior to application.
*Examples of experience would include working in General Medical Nursing where patient with diabetes are cared for, Emergency Departments, Endocrinology ward/departments
Note: Post holders must maintain annual registration with Bord Altranais agus Cnáimhseachais na hÉireann (Nursing Midwifery Board Ireland)
Age
No age restriction shall apply to a candidate where he/she is not classified as a new entrant
(within the meaning of the Public Service Superannuation Act, 2004). In this case the candidate must be under 65 years of age on the first day of the month in which the latest date for receiving completed application forms for the office occurs.
Health
Candidates for and any person holding the office must be fully competent and capable of undertaking the duties attached to the office and be in a state of health such as would indicate a reasonable prospect of ability to render regular and efficient service.
Character
Candidates for and any person holding the office must be of good character.
Demonstrate depth and breadth of experience in providing nursing care relevant to the area of diabetes to include experience of working autonomously in the Acute Hospital Services and experience of constructing diabetic care packages/treatment programmes for diabetic clients.
Access to transport as post may involve travel.
Other requirements specific to the post
Skills, competencies and/or knowledge
Candidates must demonstrate:
practitioner competence and professional credibility – demonstrates a high level of clinical
knowledge to effectively carry out the duties and responsibilities of the role the ability to lead on clinical practice and service quality promotion of evidence-based decision making; evidence-based clinical knowledge in making decisions regarding patient / client care the ability to plan and manage resource effectively effective analytical, problem solving and decision making skills strong interpersonal skills including the ability to build and maintain relationships effective communication and influencing skills initiative and innovation in the delivery of service resilience and composure openness to change integrity and an ethical stance a commitment to continuing professional development the ability to relate nursing research to nursing practice knowledge of quality assurance practices and their application to nursing procedures
awareness of relevant legislation and policy e.g. legislation relevant to the service area, health and safety, infection control etc. awareness of current and emerging nursing strategies and policies in relation to the
clinical/designated area awareness of the Health Service Structures a willingness to develop IT skills relevant to the role
6
Competition
Specific Selection
Process
Shortlisting /
Interview
Short listing may be carried out on the basis of information supplied in your application form.
The criteria for short listing are based on the requirements of the post as outlined in the eligibility criteria and skills, competencies and/or knowledge section of this job specification.
Therefore it is very important that you think about your experience in light of those requirements.
Failure to include information regarding these requirements may result in you not being called forward to the next stage of the selection process.
Those successful at the shortlisting stage of this process (where applied) will be called forward to interview.
Code of Practice
The Health Service Executive will run this campaign in compliance with the Code of Practice prepared by the Commission for Public Service Appointments (CPSA). The Code of Practice sets out how the core principles of probity, merit, equity and fairness might be applied on a principle basis. The Codes also specifies the responsibilities placed on candidates, feedback facilities for candidates on matters relating to their application, when requested, and outlines procedures in relation to requests for a review of the recruitment and selection process, and review in relation to allegations of a breach of the Code of Practice. Additional information on the HSE’s review process is available in the document posted with each vacancy entitled
“Code Of Practice, Information For Candidates”.
Codes of Practice are published by the CPSA and are available on www.hse.ie/eng/staff/jobs in the document posted with each vacancy entitled “Code of Practice, Information For
Candidates” or on www.cpsa-online.ie
.
The reform programme outlined for the Health Services may impact on this role and as structures change the job description may be reviewed.
This job description is a guide to the general range of duties assigned to the post holder. It is intended to be neither definitive nor restrictive and is subject to periodic review with the employee concerned.
7
Tenure
Remuneration
Working Week
Annual Leave
Clinical Nurse Specialist (Diabetes)
Terms and Conditions of Employment
The initial vacancy for this post is permanent whole time. This post is pensionable. A panel will be formed from this recruitment campaign and future permanent or specified purpose vacancies of whole-time or part-time duration will be filled from this panel. The tenure of these posts will be indicated at “expression of interest” stage
Appointment as an employee of the Health Service Executive is governed by the Health Act
2004 and the Public Service Management (Recruitment and Appointment) Act 2004.
The Salary Scale (as at 01/07/13) for the post is:
Euro 47,089 – 47,886 – 48,559 – 49,659 – 50,874 – 52,067 – 53,260 – 54,604 – 55,852 (pro rata)
The standard working week applying to the post is: 39 hours (pro rata)
HSE Circular 0032009 “Matching Working Patterns to Service Needs (Extended Working
Day / Week Arrangements); Framework for Implementation of Clause 30.4 of Towards 2016” applies. Under the terms of this circular, all new entrants and staff appointed to promotional posts from Dec 16 th 2008 will be required to work agreed roster / on call arrangements as advised by their line manager. Contracted hours of work are liable to change between the hours of 8am-8pm over seven days to meet the requirements for extended day services in accordance with the terms of the Framework Agreement (Implementation of Clause 30.4 of
Towards 2016).
The annual leave associated with the post is to be confirmed at job offer stage.
Superannuation
Membership of the HSE Employee Superannuation Scheme applies to this appointment.
Existing Members who transferred to the HSE on 1st January 2005 pursuant to Section 60 of the Health Act 2004 are entitled to superannuation benefit terms under the HSE Scheme
Probation
Every appointment of a person who is not already a permanent officer of the Health Service
Executive or of a Local Authority shall be subject to a probationary period of 12 months as stipulated in the Department of Health Circular No.10/71.
Protection of
Persons
Reporting Child
Abuse Act 1998 1
As this post is one of those designated under the Protection of Persons Reporting Child Abuse
Act 1998, appointment to this post appoints one as a designated officer in accordance with
Section 2 of the Act. You will remain a designated officer for the duration of your appointment to your current post or for the duration of your appointment to such other post as is included in the categories specified in the Ministerial Direction. You will receive full information on your responsibilities under the Act on appointment.
Infection Control Have a working knowledge of HIQA Standards as they apply to the role, including National
Standards for Safer, Better Healthcare (2012), National Standards for the Prevention and
Control of Healthcare Associated Infections (2009), National Hygiene Services Quality
Review (2008); Standards and Criteria etc. which are no less favourable to those to which they were entitled at 31st December 2004.
Appointees to posts in the Mental Health Services which formerly attracted fast accrual of service should note that the terms of Section 65 of the Mental Treatment Act 1945 do not apply to New Entrant Public Servants as defined by Section 12 of the Public Service
Superannuation (Miscellaneous Provisions) Act 2004.
8