Using the MBS to access services for children with behavioural
advertisement

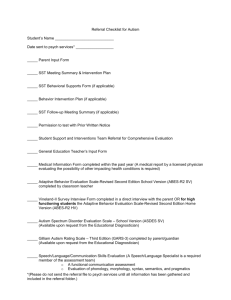
Using the MBS to access services for children with behavioural disorders. Under the MBS there are 2 options to assist children and their families with management of behavioural disorders 1. Helping Children with Autism or any other Pervasive Developmental Disorder (PDD) MBS initiative 2. Better access to psychiatrists, psychologists and general practitioners through the MBS (Better Access) initiative 1 Helping Children with Autism or any other Pervasive Developmental Disorder (PDD) The Helping Children with Autism or any other Pervasive Developmental Disorder (PDD) MBS initiative created items in the Medicare Benefits Schedule; and provides early intervention and individual assistance packages for children and their families. It assists children with autism or any other pervasive developmental disorders See DSM-IV-TR criteria Note: GPs may have patients referred by teachers for assessment of eligibility under this package and thereby enable increased classroom support. However strict criteria define access to this suite of MBS items and GPs can assist through ensuring appropriate referral. The collection of relevant information should be completed prior to the referral. The Helping Children with Autism package provides rebates for: consultant physicians (paediatricians and psychiatrists) to diagnose and develop a treatment plan for children aged under 13 years on referral from a GP Psychologists, speech pathologists and occupational therapists to provide up to four services in total per child per lifetime to collaborate with the psychiatrist or paediatrician on the assessment where required ( ie assist with diagnosis of PDD) Psychologists, speech pathologists and occupational therapists to provide early intervention treatment following diagnosis for the child’s particular condition and consistent with the treatment and management plan prepared by the referring practitioner. Twenty services in total per lifetime may be provided for a child aged under 15 years, who was under 13 years at the time of receiving the PDD treatment and management plan. The psychiatrist or paediatrician may need to see the child more than once, and may decide to seek assistance with either diagnosis or the treatment of the child. Under Medicare this may involve a consultation with one or more psychologists, speech pathologists or occupational therapists. Only one treatment and management plan for PDD, with either a psychiatrist or a paediatrician, can be rebated by Medicare. PDF printable version of Fact Sheet: helping children with autism (PDF 80 KB) Referral process and Recommendations for GPs prior to referral Medicare Australia requires that GPs refer to a Paediatrician or Psychiatrist who would then either determine: 1. Patient meets diagnostic criteria - complete treatment /management plan item 135 or 289 respectively then refer for the early intervention treatment – up to 20 services. OR 2. Insufficient evidence that patient meets diagnostic criteria – Refer for up to 4 allied health ( psychologist, speech pathologist or OT) services to assist with the diagnosis or contribute to the treatment plan. Following assessment and if patient meets diagnostic criteria the Paediatrician or Psychiatrist will then complete treatment /management plan item 135 or 289 respectively then refer for the early intervention treatment – up to 20 services. To help children with autism it is essential to focus on the earliest years of development, since this is a critically important time for early learning which powerfully affects the child's future life course. It has been shown that diagnosis can be valid and reliable at 2 years of age, and signs can be recognisable and predictive of autism even from early in the second year of life. To assist diagnostic evaluations it is important that as much information is available at the time of the assessment. This may require patient to be referred for additional assessment prior to diagnosis. Therefore at the time of referral it is important to ensure the following information is collated. Referral should include reference to: Information regarding the child's developmental history and family history, Information from all professionals involved in the care of the child including previous assessments and interventions. This would include where available: Paediatric, psychological, and speech pathology examinations that assess communication, relevant health conditions including motor skills, vision, hearing, and any associated problems such as intellectual disability and anxiety. Any observations of the child in the assessment of cognitive, social, communicative (verbal & nonverbal), fine and gross motor, and adaptive functioning using both standardised tests and informal procedures. Cognitive reports- Reports from teachers and school reports should be collected. Schools are in an effective position to assess students who have early signs of mental health difficulties, due to the significant amount of contact that they have with students and their families. 2 GP Mental Health Care Medicare Items These items are part of the Better access to psychiatrists, psychologists and general practitioners through the MBS (Better Access) initiative . The GP Mental Health Care items provide a structured framework for GPs to undertake early intervention, assessment and management of patients with mental disorders, as well as providing referral pathways to psychiatrists, clinical psychologist and allied mental health service (registered psychologists and appropriately trained social workers and occupational therapists) Refer available for child with the following conditions: Hyperkinetic (attention deficit) disorder Conduct disorder Enuresis (non-organic) Eating disorders The referral may be used to support the child, parents or entire family for example though providing 1 Parental education –teaching parents how to communicate with and manage their children 2 Functional family therapy – the entire family is helped to improve communication and problem-solving skills. 3 Individual therapy -Focussed Psychological Strategies 1) Psycho-education including. 2) Cognitive-behavioural therapy including: a Behaviour modification b Exposure techniques c Activity scheduling 3) Skills Training a Problem solving skills and training b Anger management c Social skills training d Communication training e Stress management f Parent management training 4) Relaxation Strategies including progressive muscle relaxation / controlled breathing 5) Interpersonal Therapy There is flexibility to include narrative therapy for Aboriginal and Torres Strait Islander people Recommendations for GP referral 1. A GP Mental Health Treatment Care Plan must be in place (and item 2710 billed) or a GP Mental Health Plan item 2702 ( for GPs who have not undertaken Mental Health Skills Training) 2. Patients with a Referred Assessment and Management Plan from a psychiatrist or paediatrician are also eligible 3. No specific referral form is required (GPs may wish to consider providing a copy of the plan) 4. Each patient eligible for 12 individual + 12 group sessions per calendar year 5. 12 session cap is inclusive of division run ATAPS services 6. Allied health professional must report back to the GP after each block of 6 sessions 7. GP needs to review the patient and confirm the referral in writing after each block of 6 sessions List of providers: Darwin Directory of Psychological Services that have an interest in child behaviour disorders. Other Resources Autism NT Shop 19, Nightcliff Shopping Centre Dick Ward Drive Coconut Grove NT 0810 Head: Alison Bird (Director) Phone: (08) 8948 4424 (9-1pm) Email: autismnt@bigpond.net.au Autism NT inc is a non government, not for profit organisation which aims to offer support and information to those who are living and working with autism spectrum disorders as well as the general public throughout the Northern Territory. Autism NT has a volunteer committee and maintains a database of services through which parents can also access online support and learning programs. Helping Children with Autism http://www.health.gov.au/internet/main/publishing.nsf/Content/autism-children Early intervention for children with autism spectrum disorders: guidelines for best practice http://www.health.gov.au/internet/main/publishing.nsf/Content/mental-pubs-e-autbro Parentline - Provides support, counselling and parent education for the cost of a local call. Parentline operates in Queensland and the Northern Territory. Mobile phone charges apply. Call 1300 30 1300 from 8am-10pm, 7 days a week. Web: http://www.parentline.com.au/ Parentline offers individually-paced telephone and web based parenting programs for parents and carers . It uses the Triple P-Positive Parenting Program® is a parenting and family support strategy. Kids Help Line - a national telephone counselling service for young people aged 5 to 18 years 1800 55 1800 Online counselling available at www.kidshelpline.com.au Raising Children Network The complete Australian parenting resource from newborns to teens Comprehensive section for professionals includes tools, resources, links to relevant organisations around the country and printable handouts. Range of videos, parents share their experiences of loving and caring for their preschoolers. Experts talk about preschooler health and nutrition. You can also see practical demonstrations of first aid, eating strategies, positive behaviour techniques, and much more.