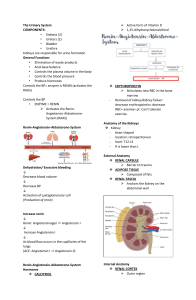
Renin Angiotensin System
advertisement
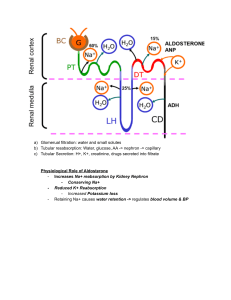
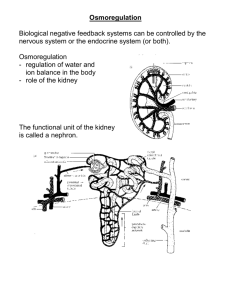
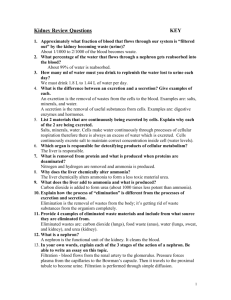
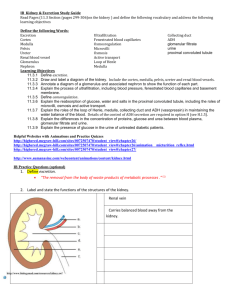
Renin Angiotensin System A second regulatory mechanism involves a special tissue called the juxtaglomerula apparatus (JGA), located near the afferent arteriole the supplies blood to the glomerulus. 1. When blood pressure or blood volume in the afferent arteriole drops, the enzyme renin initiates chemical reaction that convert a plasma protein angiotensinogen to a peptide called angiotensin II. a. Acting as a hormone, angiotensin II increases blood pressure and blood volume in several ways. b. It raises blood pressure by constricting arterioles, decreasing blood flow to many capillaries, including those of the kidney c. It also stimulates the proximal tubules to reabsorb more NaCl and water. 2. This reduces the amount of salt and water excreted and consequently, raises blood pressure and volume. It also stimulates the adrenal glands, located atop the kidneys to release aldosterone. This acts on the distal tubules, which reabsorb Na+ and water, increasing blood volume and pressure. In summary, the renin-angiotensin-aldosterone system (RASS) is part of a complex feedback circuit that functions in homeostasis. 1. A drop in blood pressure triggers a release of renin from the JGA 2. In turn, the rise in blood pressure and volume resulting from the various actions of angiotensin II and aldosterone reduces the release of renin 3. While both ADH and RAAS increase water reabsorption, they counter different osmoregulatory problems. a. They release of ADH is a response to an increase to an increase in the osmolarity of the blood, as when the body is dehydrated from excessive loss or inadequate intake of water. b. However, a situation that causes excessive loss of salt and body fluids-an injury or severe diarrhea, for example-will reduce blood volume without increasing osmolarity. c. The RAAS will detect the fail in blood volume and pressure and respond by increasing water and NA reabsorption. 4. Normally. AHD and the RAAS are partners in homeostasis. a. ADH alone would lower blood Na concentration by stimulating water reabsorption in the kidney. b. But the RAAS helps maintain balance by stimulating Na reabsorption. Excretory System Disorders Bright’s disease or Nephritis Not a single disease but a broad description of many diseases all caused by inflammation of the nephron (infections, fever, parasite) Permeability of nephron is altered so large molecules (proteins) pass into the nephron and can’t be reabsorbed. This draws water by osmosis increasing urine output. Diabetes Insipidus Destruction of ADH producing cells or nerve pathways loss of ADH increases urine output dramatically (>20L/day) loss of water in urine thus increase in thirst Kidney stones Precipitation of salt crystals usually from calcium and oxalic, uric, or phosphoric acid in urine results in stones that block the ureters causing swelling and urine back-up in kidneys Review Questions 1. A blood clot lodges in the renal artery and restricts blood flow to the kidney. Explain why this condition leads to high blood pressure. 2. A pH analysis of urine reveals that the urine of humans fluctuates between acidic and basic depending on the diet. How does the kidney help to maintain a constant blood pH? 3. Researchers found that a camel standing in the sun required much more water when its fur was shaved off although its body temperature remain the same. What can you conclude about the relationship between osmoregulation and the insulation provided by fur? 4. Many medications make the lining of the collecting duct less permeable to water. How would taking such a drug affect kidney output? Answers 1. It’s making the pathway smaller restricting blood from going through. The kidney will not filter as efficiently and over time, junk will pile up in the blood therefore blood pressure goes up. 2. 3. The fur keeps the camel from sweating and the water from evaporating. Also the fur helps insulate against heat by trapping the cool air and with the bright colour fur it reflects more light. 4.