outline29753
advertisement
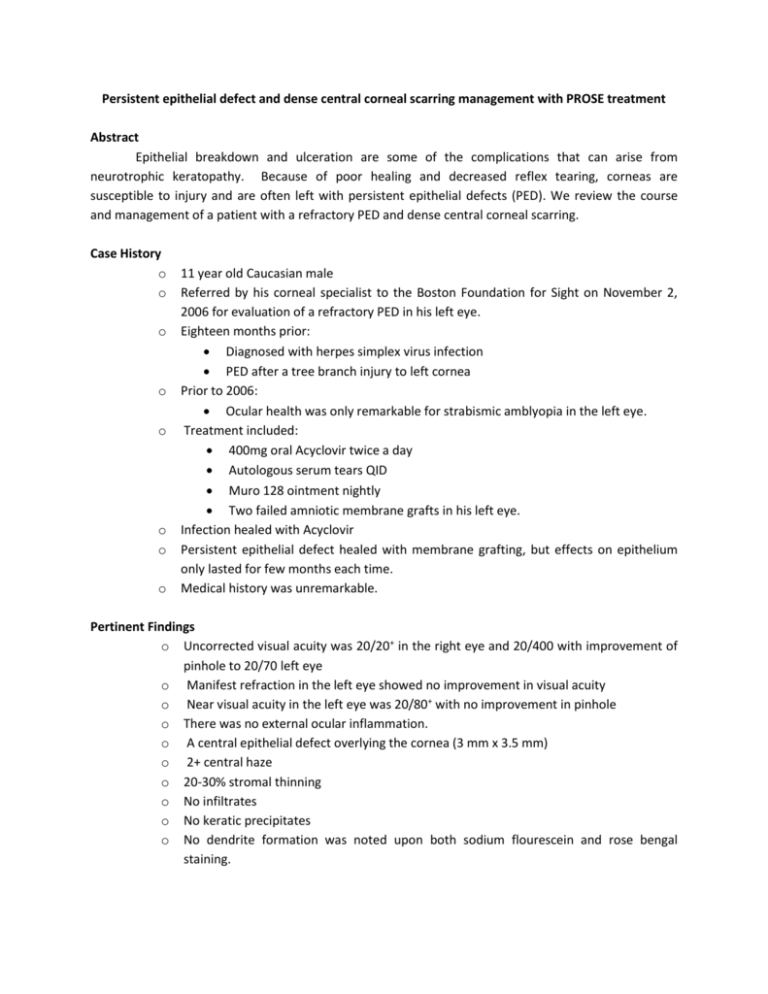
Persistent epithelial defect and dense central corneal scarring management with PROSE treatment Abstract Epithelial breakdown and ulceration are some of the complications that can arise from neurotrophic keratopathy. Because of poor healing and decreased reflex tearing, corneas are susceptible to injury and are often left with persistent epithelial defects (PED). We review the course and management of a patient with a refractory PED and dense central corneal scarring. Case History o o o o o o o o 11 year old Caucasian male Referred by his corneal specialist to the Boston Foundation for Sight on November 2, 2006 for evaluation of a refractory PED in his left eye. Eighteen months prior: Diagnosed with herpes simplex virus infection PED after a tree branch injury to left cornea Prior to 2006: Ocular health was only remarkable for strabismic amblyopia in the left eye. Treatment included: 400mg oral Acyclovir twice a day Autologous serum tears QID Muro 128 ointment nightly Two failed amniotic membrane grafts in his left eye. Infection healed with Acyclovir Persistent epithelial defect healed with membrane grafting, but effects on epithelium only lasted for few months each time. Medical history was unremarkable. Pertinent Findings o Uncorrected visual acuity was 20/20+ in the right eye and 20/400 with improvement of pinhole to 20/70 left eye o Manifest refraction in the left eye showed no improvement in visual acuity o Near visual acuity in the left eye was 20/80+ with no improvement in pinhole o There was no external ocular inflammation. o A central epithelial defect overlying the cornea (3 mm x 3.5 mm) o 2+ central haze o 20-30% stromal thinning o No infiltrates o No keratic precipitates o No dendrite formation was noted upon both sodium flourescein and rose bengal staining. o o o o o Corneal sensitivity assessed using a Luneau Cochet-Bonnet Aesthesiometer; 0.5 mm right eye and 7 mm left eye. Intraocular pressure by Tonopen was 11 mmgH in both eyes. Other anterior segment structures, the lens, and the anterior chamber were normal. Undilated fundus examination with a 90D lens was difficult to attain secondary to extreme photophobia. Fleeting views of fundus showed a normal macular structure and unremarkable optic nerve. Differential Diagnosis o Diagnosis: Refractory persistent epithelial defect from neurotrophic keratopathy Status post herpes simplex virus infection o Differential Diagnoses: Infectious corneal ulcer Neurotrophic corneal melting Diagnosis and Discussion o Neurotrophic keratopathy is a degenerative corneal disease that can lead to: Poor healing Decreased reflex blinking Persistent epithelial defects Ulceration Infection Corneal melting Perforation Permanent vision loss o Further risks: Corneal hypoaesthesia Complete corneal anesthesia In pediatric patients: amblyopia Delayed recognition of corneal complications until: Visual acuity is impaired Visual cues to hazy appearance of cornea o This case: Persistent epithelial defect was central Significant stromal haze and scarring was present Previous topical and surgical interventions failed Treatment and Management o Prosthetic replacement of the ocular surface system (PROSE) treatment o o Use of scleral prosthetic devices. These are FDA-approved custom designed and fabricated prosthetic devices: Restore vision, Support healing Reduce symptoms Improve quality of life for patients suffering with complex corneal disease Large diameter (average 15.5–23 mm) Designed to rest entirely on the sclera Vault entirely the cornea Creating a space filled with preservative-free artificial tears or saline They are fluid-ventilated Allow the containment of an oxygenated pool of artificial tears free of air bubbles over the cornea This case: CC was custom-fitted with a scleral prosthetic device Device was worn on a daily wear schedule Nightly disinfection with hydrogen peroxide system Erythromycin ointment use every night Progression of persistent epithelial healing over the course of two weeks PED healed in 2 weeks Contrast to 18 months of failed traditional therapeutic/surgical approaches Prevention of further epithelial breakdowns until present (6 year time period) PROSE treatment: Adequate ocular surface support in refractory disease Viable and excellent choice for neurotrophic keratopathy Best corrected vision after healing was 20/70-2 PH 20/50-2 Residual dense central scarring and haze No intervention with topical steroids Monitored patient over the course of six years Unexpected by-product of PROSE treatment: Complete corneal re-mottling Minimum to no corneal haze and scarring Passive and non-invasive treatment No steroids No surgical intervention Precludes need for further surgical intervention need Improved best corrected visual acuity from corneal re-mottling Vision 20/50-2 PH NI Amblyopia likely limiting factor Conclusion o o o o o Neurotrophic Keratopathy can lead to serious complications despite: Increased awareness Identification of potential risk factors Continued evolving surgical interventions, i.e. amniotic membrane grafting Continued evolving pharmacological approaches Persistent epithelial defects (PED) often develop. PED can lead to Infection Melting Perforation Vision loss PROSE treatment is viable treatment Even when traditional therapeutical approaches fail Adequate management with PROSE treatment may: Further delay or eliminate the need for further surgical interventions Provide sustainable and longstanding support of ocular surface Provide cornea with adequate environment to remottle Significantly decreasing dense haze Significantly decreasing dense scarring Minimize impact of scarring over amblyopia References 1. Rosenthal P, C. A. Eye Cont Lens 2005, (31) 130-134. 2. Jacobs DS, R. P. Cornea 2007, (26) 1195-1199. 3. Jacobs, D. Curr Opin Ophthalmol. 2008, 19(4) 298-301 4. Carr JD, Patel R, Hersh PS. J. Refract Surg 1995 (3 Suppl): S309-13