Scientists are on the cusp of using DNA from a third parent to
advertisement

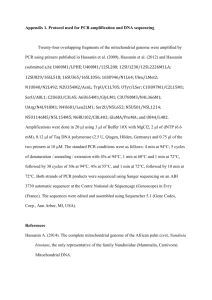
THE GENOME NEWSLETTER Sign up for our newsletter and get Genome updates in your inbox. Subscribe Search Genome Your Health Is Personal 1. newsletter 2. subscribe 3. browse 1. By Issue 1. Spring 2014 2. Summer/Fall 2014 2. By Condition 1. Alzheimer's 2. Asthma 3. Autism 4. Breast Cancer 5. Cancer 6. Colon Cancer 7. Crohn's Disease 8. Cystic Fibrosis 9. Down Syndrome 10. Heart Disease 11. IBD 12. Lung Cancer 13. Obesity 3. By Topic 1. Cover Story 2. Deep Dive 3. Editor's Note 4. From the Magazine 5. Genetics 6. Innovation 7. Policy 8. Research 9. Technology 10. Treatment 1. newsletter 2. browse 1. By Issue 2. By Topic 3. By Condition 3. subscribe T E CHNOLOGY 7 M I N RE AD Designing Healthy Babies Scientists are on the cusp of using DNA from a third parent to eliminate deadly mitochondrial genetic diseases. By Brantley Hargrove August 24, 2014 | Print | 0 Comments Shoukhrat Mitalipov works in his lab at Oregon Health and Science University in Portland. Mitalipov has developed a method to replace a mother’s mutated mitochondrial DNA with that of a healthy donor’s. The U.S. Food and Drug Administration’s decision to evaluate the procedure for possible human trials has been a source of controversy. Photographs by Robbie McClaren Lori Martin knows it is irrational to blame herself for what is happening to her son. She was a healthy 28-year-old woman when she gave birth to Will, and she had no reason to suspect he would be anything but healthy. But when they saw a pediatrician for Will’s first birthday, the doctor knew something wasn’t quite right. Will was, as Martin puts it, “floppy,” even for his age. He could bear no weight on his legs, and little muscle had developed on his growing frame. When he continued to lag behind same-age children a year later, the young Houston mother took him to a succession of specialists. The MRI a neurologist ordered gave them their first big clue. Will had lesions on his cerebellum, a region of the brain known to control motor function. Genetic testing of his spinal fluid identified the markers of Leigh syndrome, a neurological disorder characterized by the progressive loss of movement and mental abilities. The lesions often spread, causing respiratory failure and death within the first few years of life. The condition results from mutations in the mitochondrion, a ubiquitous structure acting as the cellular power plant. Unlike nuclear DNA, mitochondrial DNA doesn’t contain the kind of genetic information that will determine whether a child inherits his mother’s smile or his father’s eyes. In fact, the mitochondrion makes up a vanishingly small percentage of the human genome. Yet it is found in each and every tissue of the body. And when the mitochondrial DNA contains enough of certain mutations, it can produce an array of disorders capable of affecting nearly every organ, especially the energy-consuming neurological, muscular, digestive, and respiratory systems. About 1 in 5,000 is afflicted with an inherited mitochondrial disease. Will is 5 years old now, and he will never run, skip, or jump. He tires easily, and he can’t tolerate heat above 80 degrees. To steady his wobbling legs, he wears braces he calls boots because he wants to be a cowboy. Maintaining the progress he has made so far in his short life is a fight without an end for his parents. Martin knows it is possible she will outlive her smiling, blondhaired son. This ever-present truth is made more painful by the fact that the mitochondrial mutation that could take him away from her can only be passed down by the mother. “I’m going to be in years of therapy figuring that one out,” she says. “It’s a massive amount of guilt. I wonder if my husband blames me. I know he doesn’t, but how could some little part of you not be really angry with me?” Science has as of yet no treatment that will cure Will. But an in vitro procedure under consideration by the U.S. Food and Drug Administration may one day help prevent carriers like Martin from passing mitochondrial mutations on to their children. Shoukhrat Mitalipov, a Kazakhstan-born senior scientist at Oregon Health and Science University, has developed a method to replace the mother’s mutated mitochondrial DNA with that of a healthy donor’s. He has conducted his research without federal funding in a National Institutes of Health mirror lab because the process involves the destruction of some embryos. The research so far is at an early stage; the procedure has only been performed on non-human primates (Rhesus monkeys) and on fertilized human eggs grown to the blastocyst stage (a cluster of a few hundred cells). By imaging the mother’s immature egg and a fragile structure called the spindle, which segregates chromosomes during cell division, Mitalipov extracts the nuclear DNA. He then inserts the mother’s genetic information into a healthy egg whose nucleus has been removed. The egg, now containing mutation-free mitochondrial DNA from the donor and nuclear DNA from the mother, can then be fertilized in vitro. Research associate Nuria Marti-Gutierrez works in Mitalipov’s lab at OHSU. The genetic bond between mother and offspring remains intact, but the mitochondrial DNA the child inherits comes from the donor. “I think of it as a battery transplant,” says Arthur Caplan, a bioethicist at New York University’s Langone Medical Center. It sounds simple enough, but the specter of a child who technically bears the DNA of three parents has been a source of the controversy surrounding the FDA’s decision to evaluate the process for possible human trials. At a February hearing in Gaithersburg, Maryland, the slippery slope toward eugenics was invoked by a few guest speakers. Taken to its logical extreme, it sounds a bit like Gattaca, the film in which humans are genetically purged of disease, weakness, and criminality and where racial discrimination is supplanted by “genoism.” Salvatore DiMauro, a Columbia University Medical Center professor who gave a primer to the FDA panel on mitochondrial diseases, says the issue is a distraction. The same hand-wringing was seen during the proliferation of preimplantation genetic diagnosis, a procedure where embryos can be screened for genetic disease and a predisposition for cancer. Where would PGD take humanity along the continuum between disease prevention and engineering perfection, some wondered. But the field, DiMauro says, is a long way from selecting for specific traits like eye color and height. “It’s absurd. This is not eugenics. We’re not choosing anything. The mitochondrion is not designed; it’s donated. It’s like a kidney transplant.” Still, the FDA panel registered concerns that may need to be addressed before clinical trials get the green light. For starters, the testing was performed only on healthy human eggs. And in primate testing, there is no comparable mutation in their mitochondria. Critics contend that we don’t yet fully understand how the abnormal mitochondrial DNA segregates out as human cells divide. If you could make changes that were obviously therapeutic — not eugenical, but simply trying to repair a disease — that seems to me morally defensible. The closest parallel the field has seen took place in the late 1990s. A clinician named Jacques Cohen of Saint Barnabas Medical Center in Livingston, New Jersey, transferred the mitochondria and cytoplasm from healthy donors’ eggs into those of his infertile patients. It’s estimated that by 2001, some 100 children who had inherited mitochondrial DNA from a third party had been delivered worldwide before the FDA required the facilities to either stop their work or to first request permission. Two of the pregnancies stemming from Cohen’s facility resulted in fetuses with Turner syndrome, a condition that affects girls who are missing one sex chromosome. (One woman miscarried, and the other had an abortion.) At least two other pregnancies displayed heteroplasmy, meaning the birth mother’s mitochondrial DNA was mixed with the donor’s, creating a mismatch that can cause mental deficits and diabetes. Little follow-up of the children was performed. And it is not known if the abnormalities were connected to Cohen’s procedure, which is markedly different from the one under consideration by the FDA. Unlike Cohen’s procedure, Mitalipov’s spindle transfer eliminates nearly all of the mother’s mitochondrial DNA. But uncertainties remain. The four male monkeys produced by this transfer procedure appear healthy, yet they have only just reached maturity. If there are any side effects, like sterility, they may not have had time to manifest. “The idea that the genome is like a LEGO set that you can simply interchange parts really does not seem logical on its face,” says Jeremy Gruber, president of the Council for Responsible Genetics. “I think it’s incredibly arrogant, quite frankly, to push so rapidly for clinical trials when there’s no scientific consensus on safety.” DiMauro, for his part, believes the procedure is ready to be tested on humans. In fact, the FDA panel discussed at length how human trials might be structured. Mitalipov conceded that ovaries harvested from female monkey fetuses produced by the transfer technique bore a few eggs apiece that were heteroplastic, meaning they carried a potentially dangerous genetic mismatch. Extend this finding to humans with mutations, and the levels would probably be too low to cause disease. There is, however, a potential danger for the next generation. Mitalipov suggested the trials could be limited to male offspring to ensure that no mutations are passed along. For potential candidates, he recommended women like Martin, who have had a child with Leigh syndrome, primarily because the disease appears in early development. This way, the procedure’s success would be borne out quickly. To qualify as a participant, one panelist asked, should the woman be unable to produce normal embryos that don’t carry a significant mutation load? If a birth defect should appear, asked another, how should the researchers determine whether it was caused by the procedure, carryover mitochondrial DNA from the mother, or something else? And, for the children who result, how much follow-up is enough before the procedure is considered safe and effective? No single answer for these questions was given during the hearing. Caplan, the New York University bioethicist, suspects that the FDA may require more animal trials before signing off on the next step. Yet he believes human clinical trials are not only ethical, but also an inevitability whose time will come. “The only way it’s worrisome is that it’s crossing a line into making a change that’s heritable,” Caplan says. “That’s breaking a barrier. However, to me, that barrier was always ethically sullied because of exactly this point: If you could make changes that were obviously therapeutic — not eugenical, but simply trying to repair a disease — that seems to me morally defensible. The goal of fixing a terrible inherited disease seems to me to be a good one.” The first clinical trials may take place not in the U.S., but in England. The government there has already issued for public comment draft rules that detail how the procedure would be regulated. When and if the procedure is deemed safe, Martin says she would consider using it to have another child. In January, she gave birth to a healthy baby girl, created by a donor’s egg and her husband’s sperm. She loves the child as much as the son who shares her DNA, but she can’t help but yearn for another child who might have her eyes, her smile, but none of the mutations that may take her son someday. “Nobody’s trying to make a perfect Gerber baby,” she says. “It’s about giving our kids a chance to be healthy and happy and out of the hospital.” TAGS: designer babies DNA ethics Leigh syndrome mitochondria three parents Turner syndrome TOP STORIES T E CHNOL OGY In My Genes By Jeanette McCarthy 10 shares DE E P DIV E How Personalized Medicine Is Changing: Alzheimer’s Disease By Charlotte Huff 11 shares RE S E ARCH Change Your Microbiome, Change Yourself By Kendall K. Morgan 345 shares View All » PRINT EDITION GE NOM E M AG AZI N E Summer/Fall 2014 Subscribe RELATED READING 0 Comments T E CHNOLOGY Written in the Blood By Jeanne Erdmann Cancer doesn’t always stay in one place. Often tumor cells break free and ride the bloodstream, settling in distant organs and changing the course of… 0 Comments E DI T OR' S N OT E GE N ET I C S T E C H N OLOGY In My Genes By Jeanette McCarthy I am finally getting my genome sequenced! Well, not my whole genome, just my exome, the part made up of genes. Although it represents only… 1 Comment I NNOV AT I ON T E C H N OL OGY You Are Your Data By Leslie Minora 01 Imagine a bra that you (or ladies you know) could purchase over the counter and wear for one day to screen for breast cancer…. Genome explores the world of personalized medicine and the genomic revolution that makes it possible, empowering you to make informed health decisions that will help you live better, longer. www.genomemag.com About Us Partners & Allies Media Kit Privacy Policy Terms & Conditions Contact Us