Bacteria Reading Activity
advertisement

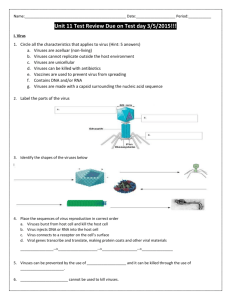
Name:_________________________________ Hour: _____ Honors Biology Unit 6 – Part 1: Bacteria and Viruses Exploring Bacterial Evolution: The Antibiotics Controversy Part 1: Background Information: Antibiotic Resistance Function and Origin of Antibiotics Antibiotics, also known as antibacterials, are types of medications that destroy or slow down the growth of bacteria, thus they are used to treat infections caused by bacteria. While many bacteria are either harmless or beneficial, some cause serious illness and disease in plants, humans, and other animals. The immune response systems of plants and animals are typically able to destroy foreign bacteria before is can multiply and cause symptoms. In humans, even if symptoms do occur, our immune system can often fight off the invasion; we have specialized white blood cells that attack the bacteria cells. However, sometimes the bacterial infection is too aggressive and cannot be fought off without the assistance of antibiotics. In 1944, Alexander Fleming discovered the first antibiotic: penicillin. This antibiotic was hailed as a miracle drug that killed bacteria but left the body unharmed. Unfortunately, because penicillin was the only antibiotic available, it was heavily used during the late 1940's. By 1949 (only 5 years after we began using it), 59% of the bacteria in sick patients were resistant to penicillin. How did this happen? Developing Antibiotic Resistance The overuse/improper use of antibiotics acts as a natural selection pressure that favors the survival and reproduction of resistant bacteria. Widespread use of antibiotics increases the proportion of resistant bacteria in a population. Over 100 antibiotics are currently available for use in infected patients today, but without stricter regulations, many of these will become ineffective in the next few years. Bacteria resist antibiotics through minor changes in their biochemistry. First, bacteria may possess enzymes that actually degrade antibiotics. Originally, only one group of bacteria had the genes for these enzymes (Streptomyces sp.), but due to genetic recombination, this enzyme is now found in a large number of bacteria groups. Second, bacteria can adapt mechanisms that alter how an antibiotic enters the cell, making it difficult or impossible for the antibiotic to disrupt the bacterial cell. They can also evolve to have modified target sites for the antibiotic (the specific structures within the bacteria that the antibiotic attacks or disrupts, such as ribosomes). Spreading Antibiotic Resistance These methods of resistance require relatively simple changes, in the DNA of the bacteria cells and are passed on to not only the offspring of those cells but also other species of bacteria that can easily incorporate them into their own genome. Bacteria have special DNA elements called R plasmids that often contain resistance genes and are easily passed to other bacteria (through conjugation). Bacteria may also take up random sequences of DNA encountered in their environment (through transformation). If this DNA contains resistance genes, the bacteria could become resistant. Viruses can also serve as a means of DNA transfer (through transduction). When bacteriophage viruses infect a host bacteria cell, DNA with resistance genes may accidently be incorporated into the new viruses that are produced. If those new daughter viruses infect other bacteria, the DNA for antibiotic resistance is spread to the other cells. Finally, bacteria can reproduce as rapidly as once every 15 minutes. If a cell contains resistance genes, all daughter cells will also have these genes. Misuse and Overuse of Antibiotics: Promoting Antibiotic Resistance In humans, antibiotics are often used when unnecessary, and when they are necessary, often the wrong antibiotic is prescribed, selecting for bacteria that have developed or received a resistance mechanism. Antibiotics are necessary when an infection cannot be eliminated through the body’s natural defenses; they are unnecessary when incorrectly prescribed for a viral infection like the "common cold." According to a study done by the Center for Disease Control, of the 150 million outpatient prescriptions each year in the United States, 50 million were estimated to be unnecessary. During hospital stays, patients are often prescribed broad-spectrum antibiotics that kill all types of bacteria, rather than targeting a specific population. Since broad-spectrum antibiotics affect all bacteria, they select for resistance in harmless bacteria, giving them the potential to become pathogenic. Antibiotics are also misused as growth enhancing supplements in food animals. Many of these animals are given antibiotics to reduce inflammation in the intestine and allow more efficient uptake of nutrients, enhancing growth. The large-scale use of antibiotics in livestock acts as a tremendous selection pressure encouraging the spread of resistance genes. Moreover, there is evidence to suggest that antibiotic resistant bacteria in food animals are able to pass their resistance to bacteria that naturally live in humans and other species. Part 2: Organizing Our Understanding Complete the table below using what you learned in class (notes), the information you recorded during the documentary clip, and the article from Part 1. How do bacteria reproduce and exchange genetic information (genetic recombination)? How do these methods of genetic recombination contribute to bacterial evolution? Part 3: Connecting Concepts: Bacterial Evolution and Antibiotic Resistance 1. What benefits do antibiotics provide to humans and other organisms (e.g. livestock)? 2. What human actions/practices lead to increases antibiotic resistance? 3. Because the use of antibiotics actually promotes the spread of bacterial resistance, many scientists believe that the use of antibiotics must be more heavily regulated. Given what you know about how antibiotic resistance spreads and the actions/practices that contribute to this spread, what steps do you think we should take to “regulate” antibiotic use? (Think: What does it mean to “regulate” our use of antibiotics? What would this look like?)